
Am Fam Physician. 2020;102(8):465-477
Related letter: Prolotherapy: An Evidence-Based Adjunctive Therapy for Knee Osteoarthritis
Author disclosure: No relevant financial affiliations.
Chronic low back pain, neck pain, hip and knee osteoarthritis, and fibromyalgia are the most common types of chronic musculoskeletal pain. Because no individual therapy has consistent benefit, a multimodal treatment approach to chronic musculoskeletal pain is recommended. Many nonpharmacologic, noninvasive treatment approaches yield small to moderate improvement and can be used with pharmacologic or more invasive modalities. Systematic reviews and guidelines support the effectiveness of various forms of exercise in improving pain and function in patients with chronic pain. Cognitive behavior therapy and mindfulness techniques appear to be effective for small to moderate short- and long-term improvement of chronic low back pain. Cognitive behavior therapy may also be effective for small short- and intermediate-term improvement of fibromyalgia. Spinal manipulation leads to a small benefit for chronic neck and low back pain. Acupuncture has a small to moderate benefit for low back pain and small benefit for nonpain fibromyalgia symptoms. Massage or myofascial release yields a small improvement in low back pain, hip and knee osteoarthritis, and fibromyalgia. Low reactive level laser therapy may provide short-term relief of chronic neck and low back pain, and ultrasound may provide short-term pain relief for knee osteoarthritis. Multidisciplinary rehabilitation may be effective for short- and at least intermediate-term improvement in pain and function for chronic low back pain and fibromyalgia. Patients should be encouraged to engage in a variety of therapies aligned with their preferences and motivation.
A chronic musculoskeletal pain disorder is the underlying diagnosis for 70% to 80% of those living with chronic pain.1 Among the top 12 causes of disability in the United States, musculoskeletal disorders cause more than one-third of years lived with disability and are among the leading causes of disability worldwide.2,3 Chronic low back pain, neck pain, hip and knee osteoarthritis, and fibromyalgia are the most common types of chronic musculoskeletal pain.
No one pain therapy alone consistently confers meaningful benefit for chronic musculoskeletal pain. On average, patients with chronic musculoskeletal pain experience small to moderate improvement in pain intensity and function from any single therapy; therefore, a multimodal treatment approach that maximizes likelihood of benefit and minimizes risk of harm is recommended.4
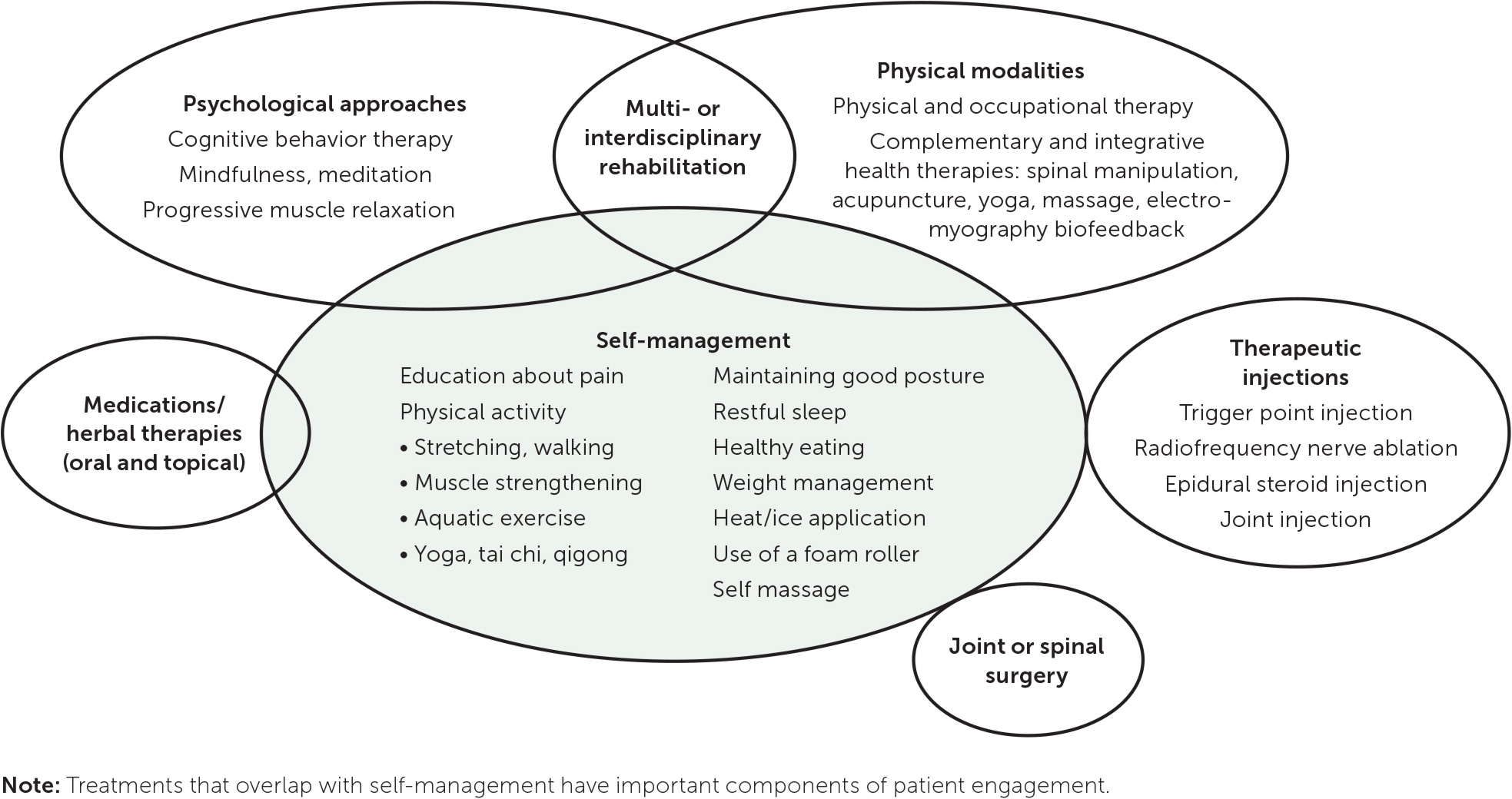
A multimodal pain treatment plan (Figure 1) should emphasize self-management and may include the physical and psychological approaches summarized in this evidence review, as well as medications and herbal therapies, therapeutic injections, and surgery, which are beyond the scope of this article. Patients should be encouraged to engage in a variety of therapies aligned with their preferences and motivation.
Patient Education
Patient education on neurophysiology, as part of a multicomponent self-management program, has demonstrated effectiveness for chronic low back pain.5 Patient education may also reduce pain and nonpain symptoms in fibromyalgia.6 Patient education on the diagnosis and on activity, lifestyle modification, and weight reduction, if indicated, is recommended but not empirically proven for osteoarthritis.7 No benefit has been established for chronic neck pain.8 The evidence for patient education is summarized in Table 1.5–37
Physical Activity
Physical activity that enhances or maintains muscle strength, physical fitness, flexibility, or overall health is recommended for most types of chronic pain.38
CHRONIC LOW BACK PAIN
Research on exercise in general shows that in patients who have low back pain with or without lumbar radiculopathy, exercise leads to a small to moderate improvement in pain and a small improvement in function in the short term10–12 (one to less than six months), small improvement in pain in the intermediate term (six to less than 12 months), and moderate improvement in pain in the long term (12 months or more).10
Motor control exercise is initially guided by a therapist, then continued independently, and focuses on improving coordination and function of the deep muscles that support the spine. It provides a moderate pain benefit and small functional benefit for low back pain that is slightly better than with general exercise for low back pain.11,12,23
Several movement disciplines improve pain and function. Yoga is recommended for chronic low back pain and results in small to moderate pain and functional benefits in the short and intermediate term.5,10–12,25–28 Tai chi (a flowing series of movements that are coordinated with breathing) results in moderate pain benefit (equivalent to swimming) and small functional benefit for low back pain.10–12
CHRONIC NECK PAIN
Motor control exercise provides moderate pain relief and small functional benefit for neck pain.24 Evidence reviews of yoga for chronic neck pain have mixed results, with one review reporting a large decrease in pain and moderate improvement in function and another reporting insufficient evidence.25,29 Tai chi leads to a small benefit for neck pain and function.25,33
HIP AND KNEE OSTEOARTHRITIS
Exercise improves symptoms of hip and knee osteoarthritis.7,10 Clinical trials of knee osteoarthritis have studied walking, gait training, mobility exercise, and exercise combinations. Trials of hip osteoarthritis have included strength training, stretching, neuromuscular control exercises, and endurance training. For knee osteoarthritis, exercise results in small to moderate improvements in pain and function in the short and intermediate term, as well as small long-term improvements in function but not pain.10,16 For hip osteoarthritis, exercise leads to small short-term improvements in pain and function and small intermediate-term improvements in function but not pain.10
Aquatic exercise results in small short-term improvements in pain, function, and health-related quality of life for hip and knee osteoarthritis.18 Yoga results in improved pain, mobility, and function for knee osteoarthritis.30,31 There is mixed evidence for tai chi in the treatment of knee osteoarthritis.10,34
FIBROMYALGIA
Clinical trials of specific forms of exercise for fibromyalgia show that resistance exercise such as lifting weights, aerobic exercise such as walking, aquatic exercise, and various combinations of exercise all yield small improvements in pain and function, and some exercise types are beneficial for other fibromyalgia symptoms.19–22 Yoga improves pain, fatigue, depression, health-related quality of life, and function in patients with fibromyalgia.30,32 Tai chi or qigong (many single movements, each of which may be repeated to address a specific concern) improves short-term pain and function.10 Tai chi also improves other common fibromyalgia symptoms.32
SUMMARY
Regular engagement in physical activity through exercise, physical therapy, and/or movement disciplines is among the most consistently beneficial approaches to the treatment of chronic musculoskeletal pain and should be the foundation of a multimodal treatment plan. Because no specific type of exercise is clearly superior, patients should be encouraged to engage in the type of low-impact exercise they prefer. The evidence for physical activity is summarized in Table 1.5–37
Psychological Therapies, Mindfulness, and Muscle Relaxation
LOW BACK PAIN
Research on psychological therapies for chronic musculoskeletal pain has focused primarily on cognitive behavior therapy (CBT) and confirms its benefit for low back pain, including small to moderate short-, intermediate-, and long-term improvement in pain. In addition, CBT confers small functional improvement in the short, intermediate, and long term.10–12,25 The most recent reviews of CBT also report improvement in function for up to two years.10,25 Operant therapy, which focuses on eliminating harmful pain behaviors and increasing beneficial behaviors by using the brain's reward system, has a small benefit for low back pain but not function.11 Evidence is insufficient regarding the effects of psychological therapies for lumbar radiculopathy.11
Mindfulness-based stress reduction (the daily practice of focusing attention on the present moment in a nonjudgmental way) results in small to moderate short-term improvement and small intermediate-term improvement in low back pain.10–12,25 Findings differ regarding its impact on function and long-term outcomes.10–12,25 One trial comparing mindfulness-based stress reduction or CBT with usual care for low back pain found that both approaches had moderate benefit for pain and function, with improvements roughly equivalent after one year; the benefit persisted after two years but was not statistically significant.39
Progressive muscle relaxation (reducing muscle tension by intentionally tensing, then relaxing, successive muscle groups) results in moderate improvement of low back pain and function.11,12 Low-quality evidence suggests that electromyography biofeedback leads to a moderate reduction in low back pain.11,12
NECK PAIN
OSTEOARTHRITIS AND FIBROMYALGIA
Psychological therapies yield small short-term improvement of knee osteoarthritis pain but not function.10 For fibromyalgia, CBT has a small short-term benefit for pain, mood, and disability and intermediate-term benefit for function. Interpretation of evidence differs regarding short-term functional impact and intermediate-term pain impact.10,41,42 One trial found that, when compared with pharmacologic therapies, CBT provided equivalent pain relief and superior functional benefit after six months in patients with fibromyalgia.10 Mindfulness-based stress reduction leads to small improvements in pain and function for fibromyalgia in the intermediate term.10,43 Biofeedback has no clear benefit for fibromyalgia.41
SUMMARY
CBT and mindfulness-based stress reduction appear to be effective for small to moderate short- and long-term improvement of low back pain. Biofeedback and progressive muscle relaxation may also be short-term treatment options for chronic low back pain. CBT appears to be effective for small short-term improvement of knee osteoarthritis pain and short- and intermediate-term improvement of fibromyalgia. Mindfulness-based stress reduction improves intermediate-term pain and function in fibromyalgia. The evidence for these techniques is summarized in Table 2.5,10–12,25,39–42,44–46
Manual Therapies and Acupuncture
Spinal manipulation (osteopathic or chiropractic) for low back pain leads to small short-term improvements in function, and inconsistent reports show small to no improvement in short-term pain intensity.10–12,47 Spinal manipulation results in small improvements in low back pain and function in the intermediate term, but there is insufficient evidence regarding long-term effects.10 Evidence on the effectiveness of spinal manipulation for lumbar radiculopathy is mixed.11,12 Spinal manipulation improves chronic neck pain and function, but interpretation of evidence differs on whether thoracic is superior to cervical manipulation.48–50 Evidence is insufficient regarding the effectiveness of spinal manipulation for fibromyalgia.51
Acupuncture provides small to moderate short-term and small long-term, but not intermediate-term, benefit for low back pain when compared with sham acupuncture.10–12,52 Overall, the quality of studies on acupuncture is low. Impact on function varies from small short-term benefit to no benefit.10–12 Evidence is insufficient regarding the effectiveness of acupuncture for lumbar radicular pain.11 Acupuncture improves function for chronic neck pain, but the effect on pain is inconsistent.10,52 The effect of acupuncture on knee osteoarthritis varies, with some studies finding a small benefit for pain in the short and long term and others finding no benefit.10,52 Acupuncture has no clear benefit for hip osteoarthritis.53 For fibromyalgia, acupuncture improves function and stiffness but has no effect on pain.10,54 Dry needling (insertion of acupuncture needles into myofascial trigger points) provides short-term relief for low back and neck pain.55–57
Massage leads to short-term improvement in low back pain and function; there is no pain benefit, conflicting interpretation of functional impact at intermediate-term follow-up, and insufficient evidence of long-term benefit.10,58,59 Compared with exercise, massage provides no additional benefit for pain or function in the intermediate term.10 Evidence is insufficient regarding the effectiveness of massage for lumbar radiculopathy.11 For neck pain, massage provides moderate pain relief and small functional improvement in the short term.10
Massage for knee osteoarthritis provides short-term benefit for pain and function.60 Other manual therapies for knee osteoarthritis provide moderate benefit for function but have no impact on pain.61 For hip osteoarthritis, manual therapies provide a small short-term improvement in pain and function and a small intermediate-term improvement in function.10 Evidence regarding the short-term impact of massage for fibromyalgia is mixed.26,62 Myofascial release for fibromyalgia yields a small intermediate-term increase in function and a small long-term reduction in pain.10
SUMMARY
Among manual therapies and acupuncture, mostly limited to short-term results, spinal manipulation is modestly effective for chronic low back and neck pain; acupuncture may be modestly to moderately effective for low back pain and nonpain symptoms of fibromyalgia and modestly or inconsistently effective for neck pain; and massage and/or myofascial release may be moderately effective for neck pain and modestly effective for low back pain, hip and knee osteoarthritis, and fibromyalgia. The evidence for manual therapies and acupuncture is summarized in Table 3.10–12,26,47–63
Treatment Devices
There is insufficient evidence for the effectiveness of transcutaneous electrical nerve stimulation in the treatment of chronic low back pain with or without associated lumbar radiculopathy, neck pain, knee osteoarthritis, or fibromyalgia.10,11,64–66 There is insufficient evidence for the use of lumbar supports for low back pain or braces for knee osteoarthritis.5,11,67 There is no short-term benefit of traction for low back pain with or without radiculopathy and insufficient evidence of benefit for chronic neck pain.10,11,68
For low back pain, low reactive level laser therapy (LLLT; the application of light in wavelengths that penetrate the skin, triggering biochemical changes to reduce pain and inflammation) provides a small to moderate short-term improvement in pain and a small improvement in function, based on low-quality evidence.10,11 For chronic neck pain, moderate evidence shows that LLLT provides moderate short-term benefit for pain and function.10 LLLT may provide short-term relief of pain and nonpain fibromyalgia symptoms.69 There is insufficient evidence for the benefit of LLLT in the treatment of lumbar radiculopathy or knee osteoarthritis.10,11 Ultrasound is not effective for low back pain or knee osteoarthritis.10,11
SUMMARY
LLLT may have short-term benefits for low back pain, neck pain, and fibromyalgia. Available evidence does not support use of other devices, including transcutaneous electrical nerve stimulation, traction, lumbar supports, and ultrasound. The evidence for treatment devices is summarized in Table 4.5,10–12,64–69
Multi- or Interdisciplinary Pain Rehabilitation
Multi- or interdisciplinary pain rehabilitation includes coordinated care by a team comprised of combinations of clinicians, physical or occupational therapists, and behavior therapists.70 It is recommended for patients with low back pain that does not respond sufficiently to first-line therapies. Multi- or interdisciplinary pain rehabilitation provides small to moderate short-term improvement in pain, function, and disability and small intermediate-term benefit for pain and function.10–12,71 Assessments of long-term benefit vary from small to no benefit.10–12,71 There is insufficient evidence regarding the effectiveness of multi- or interdisciplinary pain rehabilitation for lumbar radiculopathy.11
A Cochrane review showed that pain, disability, and work outcomes among candidates for spinal fusion were similar at two years between those treated surgically and those treated with multi- or interdisciplinary pain rehabilitation.71 Multi-or interdisciplinary pain rehabilitation results in short-, intermediate-, and long-term functional improvement and intermediate-term pain reduction in patients with fibromyalgia.10 The cost-effectiveness of this treatment approach may be enhanced by targeting patients who are most likely to benefit (e.g., those with severe functional deficits, lack of response to less intensive therapies, or significant psychosocial components).11
SUMMARY
Multi- or interdisciplinary pain rehabilitation appears effective for short- and intermediate-term improvement of low back pain and fibromyalgia, and cost-effectiveness may be enhanced by careful patient selection. The evidence for multi- or interdisciplinary pain rehabilitation therapy is summarized in Table 5.10–12,71
Data Sources: An Ovid search was completed using the following key terms: low back pain, chronic pain, neck pain, osteoarthritis, fibromyalgia. The following treatment categories were searched: exercise therapy, physical therapy modalities, braces, mind-body therapies, acupuncture therapy, rehabilitation, psychotherapy, musculoskeletal manipulations. Other search terms included noninvasive or non-invasive, nonpharmacologic* or non-pharmacologic*; exercise or physical therapy or cognitive or behavioral or feedback or relaxation or acceptance or commitment or traction or ultrasound or stimulation or laser or magnet* or inferential or electromuscular or diathermy or heat or cold or manipulation or manual or craniosacral or mindfulness or meditation or mind-body or yoga or pilates or Qigong or acupuncture or functional restoration or multidisciplin* or interdiscipin*. The search included meta-analyses or systematic reviews published in English since January 2018 and studied humans; 2018 was selected as the start date because the AHRQ review included the same search terms through mid-December 2018. Meta-analyses or systematic reviews of trigger point or dry needl* or imagery (therapies not included in the AHRQ review) were searched for the period 2010 to 2020. Also searched were the Agency for Healthcare Research and Quality Effective Healthcare Reports, the Cochrane database, and AFP POEMs (Patient-Oriented Evidence that Matters) since 2010. Search date: July 20, 2020.
The views expressed are those of the author and do not reflect the official policy of the Department of the Army, the Department of Defense, or the U.S. government.
