
Am Fam Physician. 2020;102(8):487-492
Patient information: See related handout on inguinal (groin) hernias, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Groin hernias are caused by a defect of the abdominal wall in the groin area and comprise inguinal and femoral hernias. Inguinal hernias are more common in men. Although groin hernias are easily diagnosed on physical examination in men, ultrasonography is often needed in women. Ultrasonography is also helpful when a recurrent hernia, surgical complication after repair, or other cause of groin pain (e.g., groin mass, hydrocele) is suspected. Magnetic resonance imaging has higher sensitivity and specificity than ultrasonography and is useful for diagnosing occult hernias if clinical suspicion is high despite negative ultrasound findings. Herniography, which involves injecting contrast media into the hernial sac, may be used in selected patients. Becoming familiar with the common types of surgical interventions can help family physicians facilitate postoperative care and assess for complications, including recurrence. Laparoscopic repair is associated with shorter recovery time, earlier resumption of activities of daily living, less pain, and lower recurrence rates than open repair. Watchful waiting is a reasonable and safe option in men with asymptomatic or minimally symptomatic inguinal hernias. Watchful waiting is not recommended in patients with symptomatic hernias or in nonpregnant women.
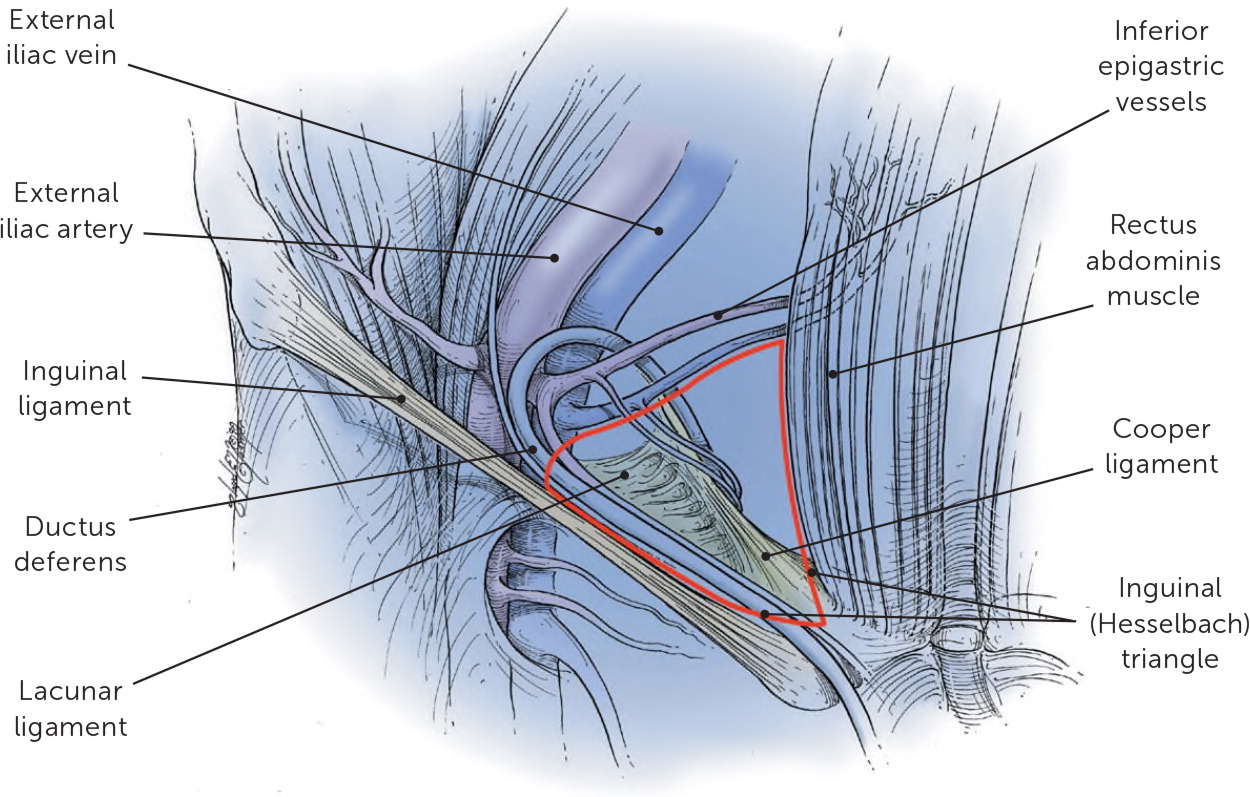
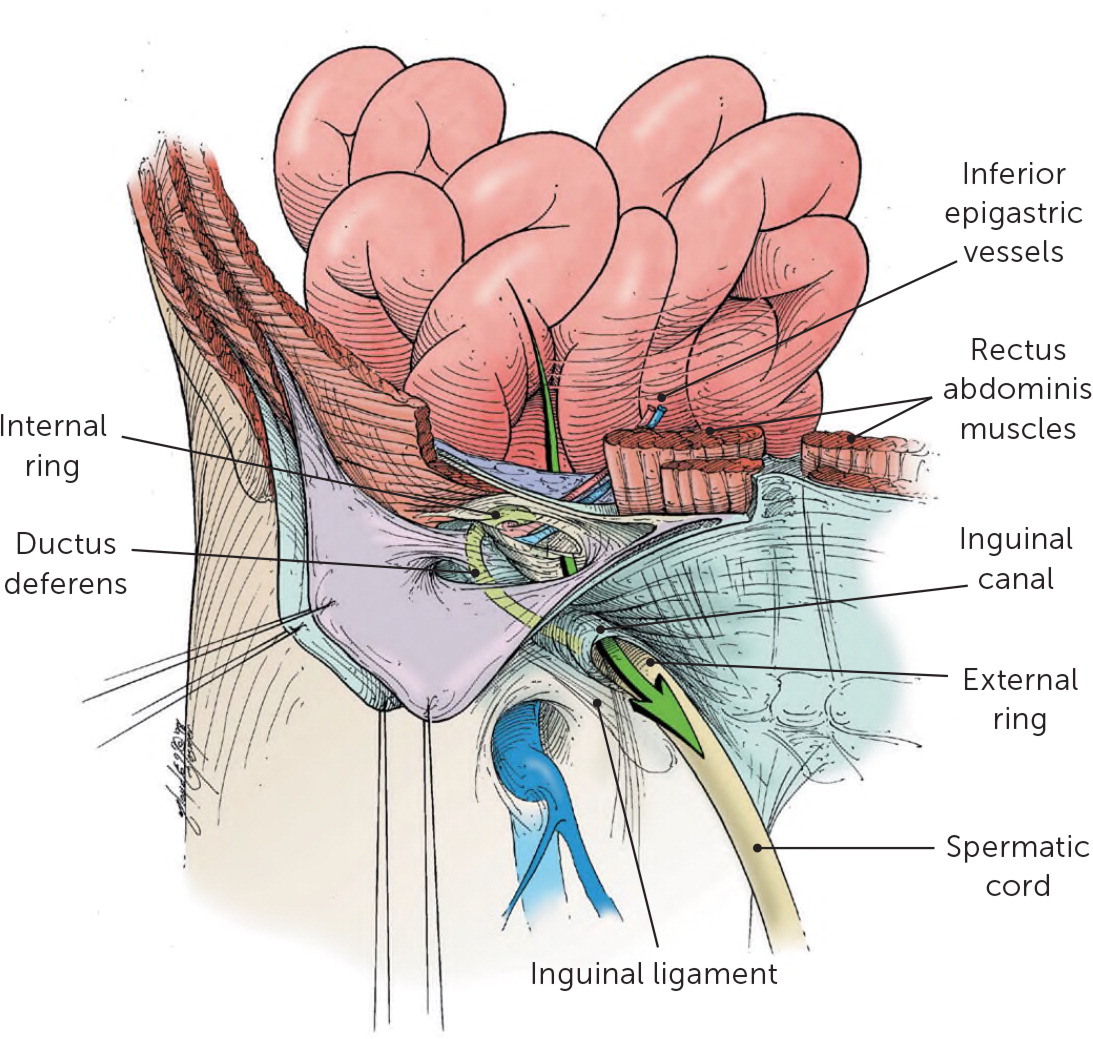
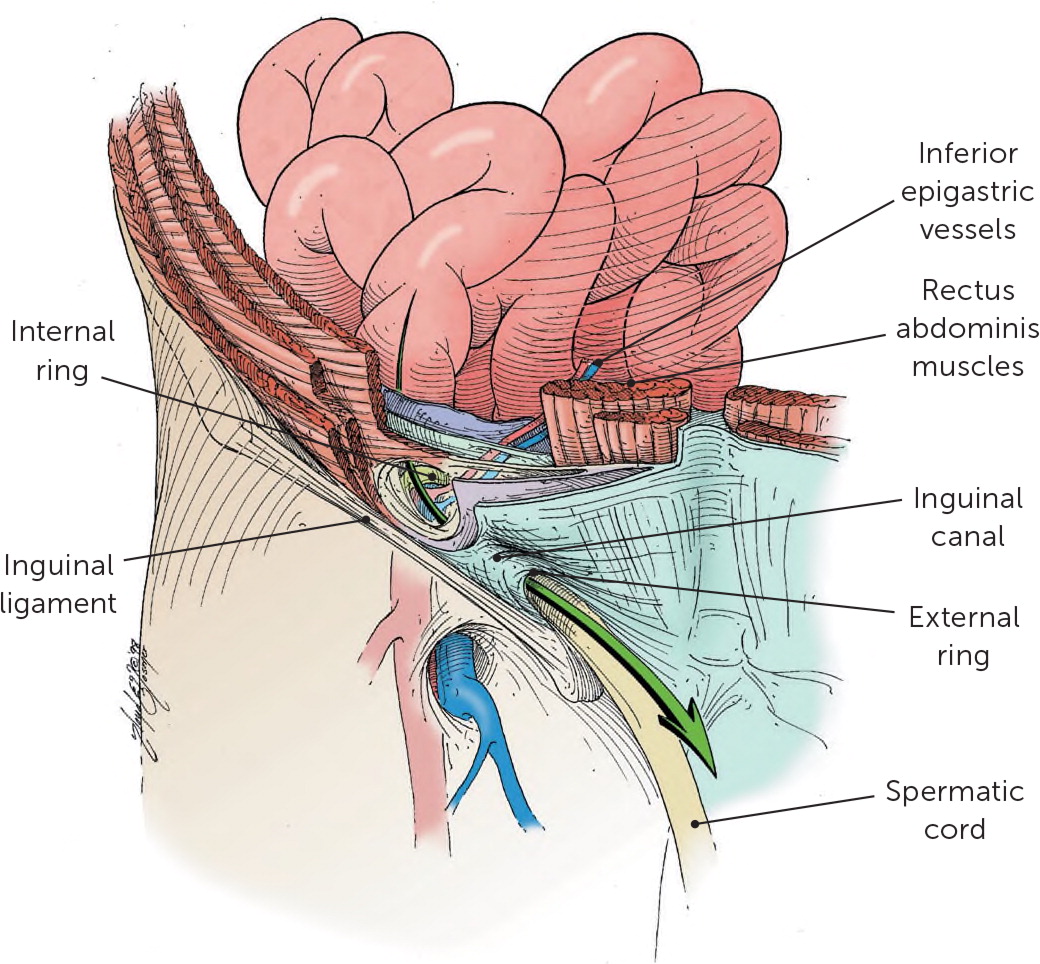
Hernias are a common reason for primary care physicians to refer patients for surgical management. There are many different types of hernias, with most occurring in the abdomen or groin. The term groin hernia comprises three types of hernias depending on location relative to the inguinal (Hesselbach) triangle (Figure 11): direct inguinal, indirect inguinal, and femoral. A direct inguinal hernia is a protrusion of tissue through the posterior wall of the inguinal canal, medial to the inferior epigastric vessels (Figure 21), whereas an indirect inguinal hernia protrudes through the internal inguinal ring, lateral to the inferior epigastric vessels (Figure 31). A femoral hernia is the protrusion of tissue below the inguinal ligament, medial to the femoral vessels.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Ultrasonography can be used to diagnose occult groin hernias.17 | B | Systematic review of lower-quality studies |
| Watchful waiting is reasonable and safe in men if the patient's usual activities are not limited by pain and discomfort and there is no difficulty reducing the hernia.20 | A | Randomized controlled trial |
| Laparoscopic hernia repair is associated with shorter recovery, earlier resumption of activities of daily living, and less pain compared with open repair.29 | A | Systematic review of randomized controlled trials |
| Recommendation | Sponsoring organization |
|---|---|
| Avoid the routine use of ultrasonography in evaluating a clinically apparent inguinal hernia. | Society of American Gastrointestinal and Endoscopic Surgeons |
In the United States, 1.6 million groin hernias are diagnosed annually, and 700,000 are repaired surgically.2 The lifetime prevalence of groin hernias is 27% in men and 3% in women.3 The frequency of groin hernia repair rises from 0.25% in patients 18 years of age to 4.2% in patients 75 to 80 years of age.3
In the United States, approximately 96% of groin hernias are inguinal hernias, about 20% of which are bilateral.1 Femoral hernias comprise the remaining 4% of groin hernias and are more common in women (16% to 37% of women).4 Risk factors for inguinal hernias include a family history of the condition, male sex, older age, low body mass index, systemic connective tissue disease, and history of radical prostatectomy or radiation therapy.5–8 In women, inguinal hernias have also been associated with taller height, chronic cough, umbilical hernia, and rural residence.6 No association has been found between smoking or alcohol use and hernias.4
Presentation
Patients with a groin hernia may report a bulge in the groin that becomes progressively larger over time. Most patients with groin hernias report pain or vague discomfort, but up to one-third of patients have no symptoms.9 Symptoms may worsen with standing, straining, lifting, or coughing. These movements increase intra-abdominal pressure, causing intra-abdominal contents to be pushed through a hernial defect.10 Patients may report having symptoms only at the end of the day or after prolonged activity and that the bulge disappears when they are lying flat. However, the absence of a reducible mass or palpable defect does not rule out a hernia. In a subset of patients, groin or pelvic pain is caused by an occult, or hidden, hernia.
Groin pain, if present, is described as a dull aching, pulling, or burning sensation. Localized discomfort may develop from stretching or tearing of the tissue at or around the site of the hernial defect. As this occurs, the hernia usually increases in size. Severe pain could suggest that the hernia has become incarcerated and may require emergent surgical intervention. Table 110,11 and Table 210 list other diagnoses to consider in patients presenting with groin pain with or without a scrotal mass. However, asymptomatic hernias may be found incidentally on physical examination.
| Visceral Abdominal hernia Adhesion Appendicitis Diverticulosis Inguinal or femoral hernia Testicular torsion Varicocele Associated with the hip Acetabular labral tear and femoroacetabular impingement Avascular necrosis Iliotibial band syndrome Osteoarthritis Snapping hip syndrome and iliopsoas tendinitis Infectious Abscess Diverticulitis Herpes infection Osteomyelitis Septic arthritis Urinary tract infection Inflammatory Endometriosis Epididymitis and orchitis Inflammatory bowel disease Pelvic inflammatory disease Prostatitis Synovitis Traumatic Muscle contusion Stress fracture Tendon avulsion Neurologic Nerve compression syndrome Referred pain (sacroiliitis, hamstring pain, knee pain) |
| Diagnosis | Clinical presentation |
|---|---|
| Ectopic testis | Absence of a testis in the scrotum |
| Epididymitis | Severe pain surrounding the testis, tenderness, fever, chills |
| Femoral adenitis/adenopathy | Bilateral, firm, tender nodes; fever |
| Femoral arterial aneurysm | Older patient, pulsatile mass, no systemic symptoms |
| Hematoma | Associated trauma, ecchymoses, tenderness, no change with Valsalva maneuver |
| Hidradenitis | Draining abscesses in intertriginous skin of the groin |
| Hydrocele | Mass in the scrotum or inguinal canal that transilluminates |
| Inguinal adenitis/adenopathy | Tenderness and redness possible, often bilateral, systemic symptoms |
| Inguinal or femoral hernia | Bulge or impulse detected in inguinal canal with Valsalva maneuver or coughing |
| Lipoma | Soft, asymptomatic mass; does not change in size |
| Lymphoma | Firm, tender mass; may increase in size; organomegaly; systemic symptoms |
| Metastatic neoplasia | Firm, tender mass; may be enlarging; systemic symptoms or weight loss |
| Psoas abscess | Flank or back pain, fever, inguinal mass, limp, weight loss |
| Sebaceous cyst | Soft, nontender mass; more superficial; no change with Valsalva maneuver |
| Testicular torsion | Acute onset of pain with a high-riding testis, swelling, very tender |
| Varicocele | Usually asymptomatic or dull ache, unilateral “bag of worms” in the scrotum |
Physical Examination
In men, the examination should begin with the patient standing and the physician seated in front of the patient. The groin should be inspected for an obvious bulge. The physician should observe for any expansile bulge while the patient “bears down” (Valsalva maneuver). An indirect hernia is often piriform in shape—broad in the scrotum and narrow over the medial half of the inguinal ligament. A direct hernia is globular in shape over the medial half of the inguinal ligament and usually does not enter the scrotum.12
If a hernia is not visualized, additional maneuvers should be performed. Using an index finger, the physician should palpate the base of the scrotum and gently invaginate the redundant skin of the scrotum into the inguinal canal toward the pubic tubercle. The finger follows adjacent to the spermatic cord, and the fingertip will be just within the external ring. The patient should then be asked to strain or cough as the physician palpates for a soft impulse, which is suggestive of herniation.13
In women, groin hernias often do not present with a visible bulge. However, a bulge can sometimes be detected on direct palpation with the Valsalva maneuver.14
Imaging
Diagnosis in men usually does not require imaging.15 However, imaging is often required in women and may be helpful when a recurrent hernia, surgical complication after repair, or other cause of groin pain (e.g., groin mass, hydrocele) is suspected. Ultrasonography, which is the first-line imaging modality, has a sensitivity of 33% to 86% and specificity of 77% to 90% for occult hernias and can be used to diagnose suspected groin hernias not evident on clinical examination.16,17
Magnetic resonance imaging (MRI) with Valsalva maneuver may be considered if the clinical suspicion of a groin hernia is high despite negative ultrasound findings. MRI has a sensitivity of 91%, specificity of 92%, positive predictive value of 95%, and negative predictive value of 85% for occult hernias. MRI is superior to ultrasonography and computed tomography in diagnosing inguinal hernias, particularly occult hernias.12 Herniography, which involves injecting contrast media into the hernial sac, has a sensitivity of 91% and specificity of 83% for detecting occult hernias. It is superior to ultrasonography and computed tomography (sensitivity = 80%; specificity = 65%) and may be useful in selected patients.17
Management
In 2018, various international societies (the HerniaSurge group) reviewed the literature and created guidelines for the management of groin hernias. The group received direct financial support from hernia mesh manufacturers Bard and Johnson & Johnson. The HerniaSurge group classifies management into two major categories: conservative and surgical.18,19
CONSERVATIVE MANAGEMENT
Watchful waiting is a reasonable and safe option in men if the patient's usual activities are not limited by pain and discomfort and there is no difficulty reducing the hernia.20 Surgical intervention should be initiated if pain develops. Watchful waiting is not recommended in nonpregnant women because of the higher likelihood of femoral hernias, which are associated with a higher risk of strangulation.21 Watchful waiting is also not recommended for symptomatic hernias because of a higher risk of incarceration.19
Abdominal contents becoming trapped within the hernial sac, leading to incarceration, is a risk of watchful waiting. Over time, this can impede the blood flow in the incarcerated hernial contents (i.e., strangulation). Richter hernia, a rare complication with a high mortality rate, occurs when part of the intestinal circumference is entrapped and strangulated in the hernial sac.22 The HerniaSurge guideline recommends that physicians counsel patients with asymptomatic or minimally symptomatic inguinal hernias about the expected natural course of the condition and the risks of emergency surgery.19
Family physicians may choose to refer patients to or work closely with a surgeon during the conservative management timeframe, which includes regular follow-up to monitor for development of symptoms and to continue surveillance for underlying diagnoses that may have contributed to the hernia. The best interval for follow-up during watchful waiting is unclear.
Watchful waiting is also commonly used in pregnant patients because groin swelling can be caused by self-limited round ligament varicosities.23 Color flow Doppler imaging can be used to distinguish between a true hernia and round ligament varicosities. In a 2017 cohort study of 20,714 pregnant patients, only 25 had inguinal hernias and none underwent elective or emergency hernia repair during pregnancy. In 10 patients, the groin bulge disappeared spontaneously after delivery.24 For reducible inguinal hernias in pregnant patients, it seems safe and cost-effective to wait until after delivery to attempt repair.
SURGICAL MANAGEMENT
The choice of surgical technique for repairing an inguinal hernia depends on factors such as anesthesia accessibility, the surgeon's preference and training, patient preference, cost, availability of mesh, and other logistics. Becoming familiar with the common types of surgical interventions can help family physicians facilitate postoperative care and assess for complications, including recurrence. Surgical interventions can be categorized as open anterior repair, open posterior repair, tension-free mesh repair, and laparoscopic repair.
Although nonmesh techniques have fallen out of favor in the United States, they are still acceptable internationally. Mesh techniques are strongly recommended because of lower recurrence rates compared with nonmesh techniques.19 If mesh is unavailable, a 2009 European guideline suggests that an open anterior nonmesh technique is most favorable.19,25
The use of laparoscopic techniques has been shown to be superior to tension-free mesh repair for postoperative pain outcomes.19 Common laparoscopic techniques include the total extraperitoneal approach and transabdominal preperitoneal approach. In both of these approaches, mesh is placed in the preperitoneal space, but access starts at different anatomic points.
Laparoscopic repair of groin hernias is preferred over open repair because of better recovery outcomes.26–29 Guidelines specifically recommend laparoscopic approaches in women to decrease the risk of chronic pain and avoid missing femoral hernias. Laparoscopic approaches can also be used in patients with previous hernias that were repaired with an open approach to avoid significant scar tissue.19 A Cochrane review comparing open and laparoscopic repair found that laparoscopic repair took longer and was associated with a higher rate of vascular, colonic, or bladder injury; however, overall, laparoscopic surgery was associated with shorter recovery, earlier resumption of activities of daily living, less pain, and lower recurrence rates.29
Postoperative Care
Historically, surgeons have recommended four to six weeks of inactivity after groin hernia repair, which was based on expert opinion.30 However, there is no evidence that early physical activity increases the risk of recurrence, regardless of surgical approach.31 Most patients undergoing laparoscopic hernia repair should be encouraged to resume physical activity three to five days after the procedure.32 Extended periods of analgesic treatment and extended sick leave are not supported by evidence.32
This article updates previous articles on this topic by LeBlanc, et al.,10 and Bax, et al.1
Data Sources: A PubMed search was completed using the key phrases (“hernia, inguinal”[mesh] and “hernia”[mesh]) and (“hernia, inguinal/classification”[mesh] or “hernia, inguinal/diagnosis”[mesh] or “hernia, inguinal/diagnostic imaging”[mesh] or “hernia, inguinal/prevention and control”[mesh] or “hernia, inguinal/rehabilitation”[mesh] or “hernia, inguinal/surgery”[mesh]). Search dates: December 6, 2019, and January 18, 2020.
