Am Fam Physician. 2021;103(7):393-394
Author disclosure: No relevant financial affiliations.
To the Editor: A 17-year-old patient presented with a solitary lump over the right chest wall of three years' duration. The patient reported that the lump was causing discomfort during contact sports and had an unattractive appearance. Clinical examination revealed a nontender, firm, and side-to-side mobile subcutaneous lump obliquely overlying the right anterolateral chest wall (Figure 1). Ultrasonography revealed a nonspecific solid heterogeneous mass measuring 76 mm × 26 mm × 18 mm. A punch biopsy result was inconclusive. Chest radiography and computed tomography were not considered practical imaging tools for this patient, and magnetic resonance imaging was not readily accessible. The patient was scheduled for an incisional biopsy under local anesthesia, with the option of excising the whole lump to avoid multiple procedures.

During the procedure, the mass was found to be protruding through the intercostal muscles and partially attached to the fascia. However, the distal part of the mass could be lifted, allowing the mass to be removed entirely following ligation of its proximal attachment to prevent arterial bleeding from the neurovascular bundle. The tumor was boat- or banana-shaped with a smooth, light-yellow surface (Figure 2). Closure of the surgical incision was uncomplicated (Figure 3). A histopathology analysis revealed a schwannoma. The patient had no postsurgical sequelae or recurrences during one year of follow-up.
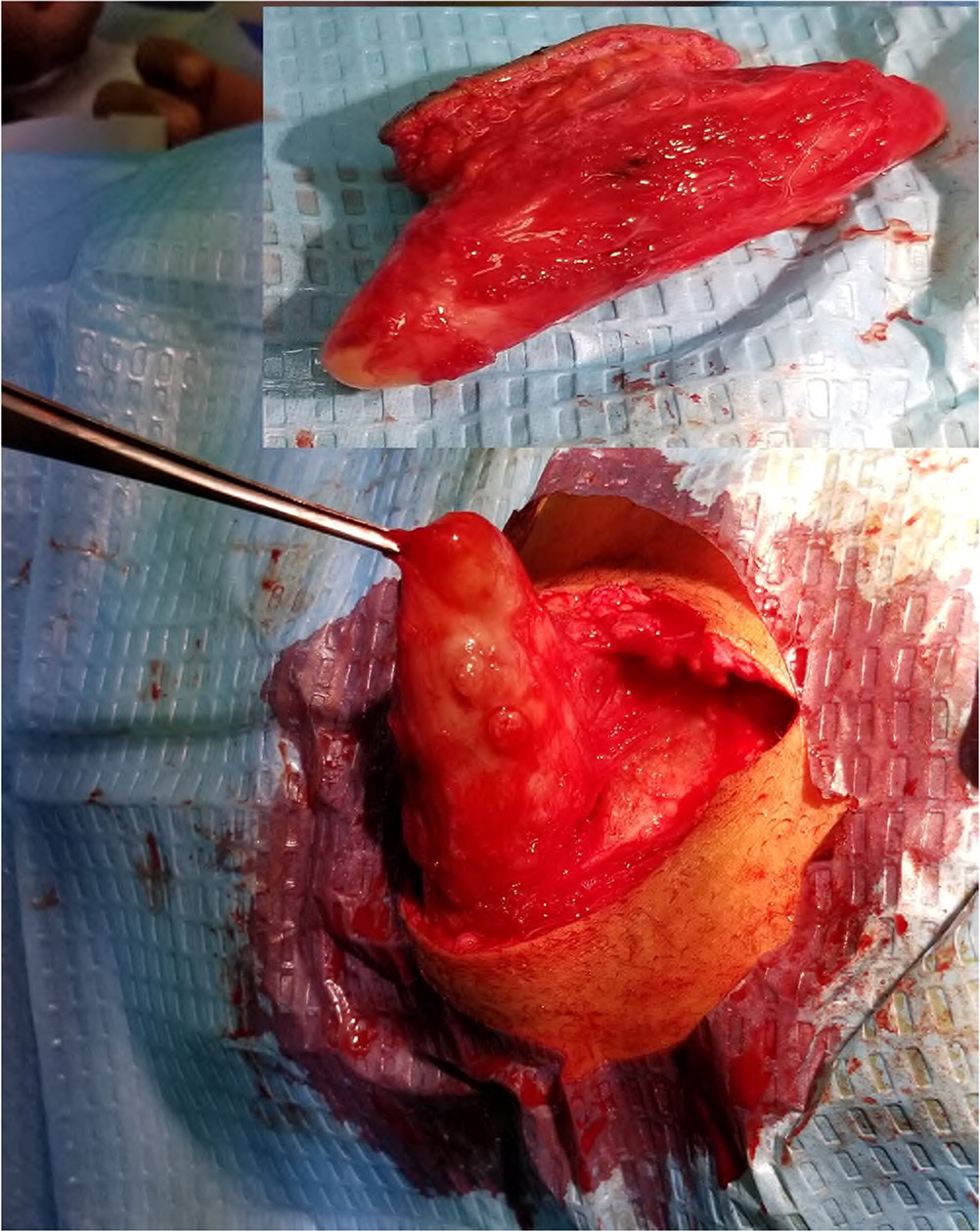

Schwannomas (i.e., neuromas) are sporadically encountered benign tumors that originate from the sheath of peripheral nerves. They can manifest as lumps in the skin and body cavity.1 Schwannomas commonly occur between 40 and 60 years of age.2,3 This patient, who first noticed the tumor at 14 years of age, might be the youngest reported case.
Ultrasonography is a useful tool for evaluating the size, attachment, and vascularity of soft tissue lumps and confirming the more common diagnoses of lipoma or cyst. However, a punch biopsy is not a practical approach for the diagnosis of subcutaneous lumps. If magnetic resonance imaging is unavailable, core, incisional, or full excisional biopsies may be performed for tissue diagnosis. Surgical excision is a definitive treatment if a patient wants a large schwannoma removed.