
Am Fam Physician. 2021;104(5):461-470
Author disclosure: No relevant financial affiliations.
Potential precipitating factors for the recent onset of altered mental status (AMS) include primary central nervous system insults, systemic infections, metabolic disturbances, toxin exposure, medications, chronic systemic diseases, and psychiatric conditions. Delirium is also an important manifestation of AMS, especially in older people who are hospitalized. Clinicians should identify and treat reversible causes of the AMS, some of which require urgent intervention to minimize morbidity and mortality. A history and physical examination guide diagnostic testing. Laboratory testing, chest radiography, and electrocardiography help diagnose infections, metabolic disturbances, toxins, and systemic conditions. Neuroimaging with computed tomography or magnetic resonance imaging should be performed when the initial evaluation does not identify a cause or raises concern for intracranial pathology. Lumbar puncture and electroencephalography are also important diagnostic tests in the evaluation of AMS. Patients at increased risk of AMS benefit from preventive measures. The underlying etiology determines the definitive treatment. When intervention is needed to control patient behaviors that threaten themselves or others, nonpharmacologic interventions are preferred to medications. Physical restraints should rarely be used and only for the shortest time possible. Medications should be used only when nonpharmacologic treatments are ineffective.
Altered mental status (AMS) can present as changes in consciousness, appearance, behavior, mood, affect, motor activity, or cognitive function.1–3 Recent changes are the focus of this article and are approached differently than chronic changes. Recent changes occur within seconds to days and usually pose a more immediate threat to a patient's well-being than chronic changes.2–4
| Recommendation | Sponsoring organization |
|---|---|
| Do not assume a diagnosis of dementia in an older adult who presents with an altered mental status and/or symptoms of confusion without assessing for delirium or delirium superimposed on dementia using a brief, sensitive, validated assessment tool. | American Academy of Nursing |
| Do not use antipsychotics as the first choice to treat behavioral and psychological symptoms of dementia. | American Geriatrics Society |
| Do not use physical or chemical restraints, outside of emergency situations, when caring for long-term care residents with dementia who display behavioral and psychological symptoms of distress; instead, assess for unmet needs or environmental triggers and intervene using nonpharmacologic approaches initially whenever possible. | American Academy of Nursing |
| Setting | Rate |
|---|---|
| Incidence during hospital admission | |
| After hip fracture | 28% to 61% |
| After surgery | 15% to 53% |
| During hospitalization (medical inpatients) | 3% to 29% |
| Prevalence | |
| Intensive care unit | |
| With mechanical ventilation | 60% to 80% |
| Without mechanical ventilation | 20% to 50% |
| Hospice | 29% |
| Community (people 85 years or older) | 14% |
| At hospital admission | 10% to 31% |
| Long-term care facility and postacute care | 1% to 60% |
The differential diagnosis for AMS is broad. A history and physical examination are the cornerstones of diagnosis, and their findings guide diagnostic testing. Preventive measures can decrease incidence and are important to use in patients at high risk. The goal of treatment is to correct the precipitating cause of the AMS.2,3,9–11
Causes of Recent AMS
Causes of recent AMS include primary central nervous system insults, systemic infections, metabolic disturbances, toxin exposure, medications, chronic systemic diseases, and psychiatric conditions (Table 2).2–4,9,10 Although a single abnormality may cause the alteration in mental status (e.g., opiate overdose), often the cause is multifactorial (e.g., dehydration, constipation, high-risk medication use).2–4,9,10
| Central nervous system insults | |
| Demyelinating conditions Direct brain trauma (concussion) Epidural hematoma Intraparenchymal hemorrhage Ischemic stroke Meningoencephalitis Neoplasm (primary or metastatic) Seizure (status epilepticus, nonconvulsive status epilepticus, or postictal state) Subarachnoid hemorrhage Subdural hematoma | |
| Commonly used medications | |
| Antibiotics (fluoroquinolones, cephalosporins) Antidepressants (tertiary amine tricyclics, monoamine oxidase inhibitors) Antipsychotics Benzodiazepines Beta blockers Bladder antispasmodics Dopamine agonists General anesthetics Opioid analgesics Sedatives or hypnotics Skeletal muscle relaxants Sympathomimetics | |
| Metabolic disturbances | |
| Hepatic failure Hypercalcemia Hypermagnesemia Hypoadrenalism/hyperadrenalism Hypoglycemia/hyperglycemia Hyponatremia/hypernatremia Hypophosphatemia Hypothyroidism/hyperthyroidism Renal failure Thiamine deficiency | |
| Systemic diseases or conditions | |
| Arrhythmia Autoimmune conditions Constipation Dehydration Heart failure Hypercapnia Hypertensive emergency Hypothermia Hypoxia Myocardial infarction Pain Pancreatitis Primary psychiatric conditions Sleep deprivation Urinary retention | |
| Systemic infections | |
| Acute viral (influenza, COVID-19, and others) Intra-abdominal Pneumonia Sepsis Urinary tract | |
| Toxins | |
| Alcohol (withdrawal or intoxication) Illicit substances (withdrawal or intoxication) |
Among the most common and important presentations of AMS is delirium, especially in older adults who are hospitalized.6,9 The hallmarks of delirium are acute, fluctuating changes in attention, awareness, and cognition that are not attributable to a neurocognitive disorder. Evidence of a secondary cause of AMS is often also present.6,9 Other features include sleep disturbances, hallucinations, delusions, inappropriate behavior, and emotional instability.11 Delirium was reviewed in a previous American Family Physician article.6
Evaluation
Changes in consciousness, appearance, behavior, mood, affect, or motor activity are usually apparent by general observation and interaction with the patient.
URGENT INTERVENTION
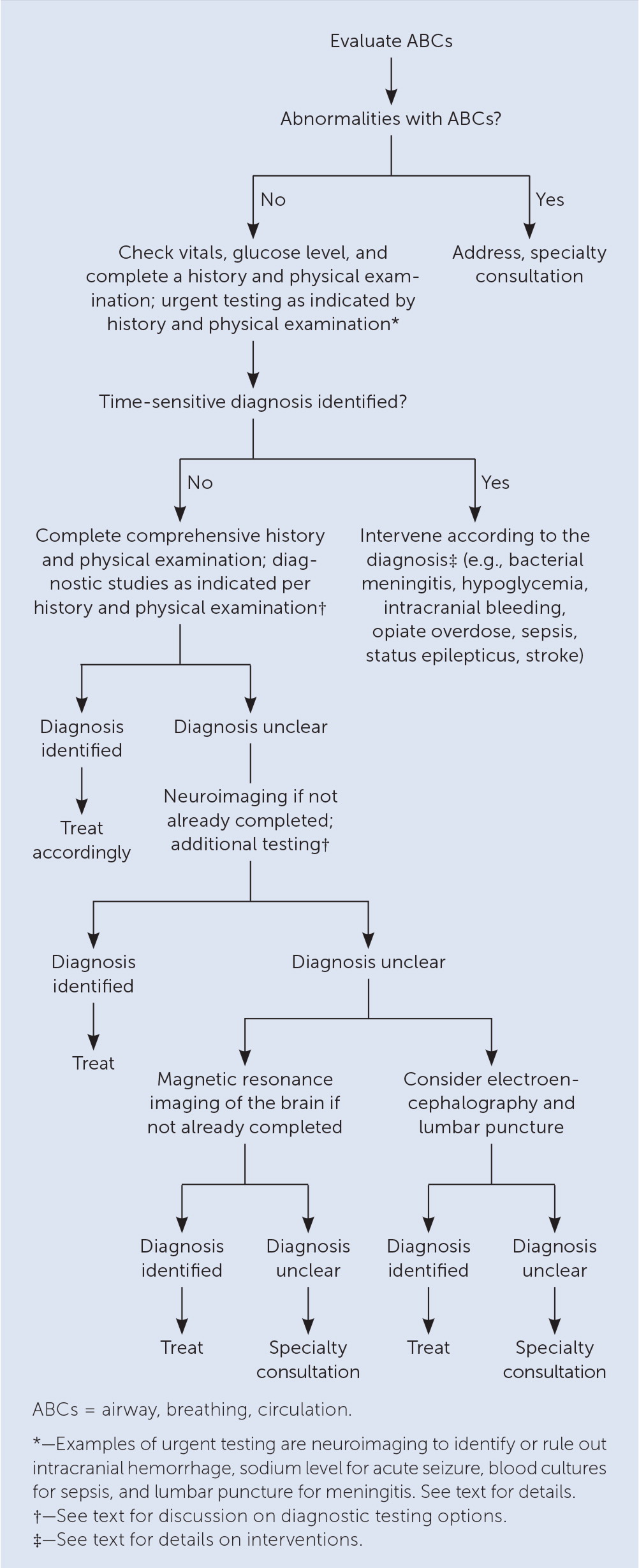
Once the ABCs have been stabilized, clinicians should evaluate for other conditions for which rapid intervention is needed to decrease the risk of morbidity and mortality. Abnormal vital signs may identify an obvious cause such as hypothermia, hypoxemia, or a hypertensive emergency, and such abnormalities should be addressed urgently.2,3,10
A point-of-care glucose level should be obtained, and if hypoglycemia is present, glucose should be administered immediately unless the patient is at risk of thiamine deficiency (e.g., alcoholism, gastric bypass surgery). Then thiamine must be administered before glucose to avoid Wernicke encephalopathy (i.e., AMS, oculomotor dysfunction, and ataxia due to thiamine deficiency).2,3,10
If concern exists for intracranial hemorrhage (e.g., anticoagulated state, head trauma) or ischemic stroke (e.g., focal abnormalities found during a neurologic examination), neuroimaging should be performed immediately to determine the next steps for care. Patients with a hemorrhage may require urgent surgery, and those with ischemic stroke can be triaged for reperfusion.2,3,10
Patients with status epilepticus need urgent anticonvulsive therapy and serum sodium testing. Patients with suspected sepsis require fluid resuscitation, urgent broad-spectrum antibiotics after cultures are obtained, and source control. Similarly, if meningitis is suspected, antibiotics at appropriate doses are urgently required following neuroimaging and lumbar puncture. If clinical suspicion is high and lumbar puncture will be delayed, antibiotics should be given empirically. When an opiate overdose is suspected, naloxone should be administered immediately.2,3,10
IDENTIFYING THE CAUSE OF AMS
Baseline cognitive function should be clarified. The timing of the onset of mental status changes is also important because abrupt and severe changes indicate a more serious pathology. The results of numerous observational assessments and answers to questions asked directly to the patient (when possible) can often suggest a cause1–3,10 (Table 31).
| Component | Definition/content | What to assess | Sample questions/tests | Potential diagnoses if abnormal |
|---|---|---|---|---|
| General observations | ||||
| Appearance and behavior | Body habitus, eye contact, interpersonal style, style of dress | Appearance: attention to detail, attire, distinguishing features (e.g., scars, tattoos), grooming, hygiene Behavior: candid, congenial, cooperative, defensive, engaging, guarded, hostile, irritable, open, relaxed, resistant, shy, withdrawn Eye contact: fleeting, good, none, sporadic | NA | Disheveled: depression, schizophrenia/psychotic disorder, substance use Irritable: anxiety Paranoid: psychotic disorder Poor eye contact: depression, psychotic disorder Provocative: personality disorder or trait |
| Mood and affect | Mood: subjective report of emotional state by patient Affect: objective observation of patient's emotional state by physician | Body movements/making contact with others, facial expressions (tearfulness, smiles, frowns) | How is your mood? Have you felt sad/discouraged lately? Have you felt energized/out of control lately? | Mood disorder, schizophrenia, substance use |
| Motor activity | Facial expressions, movements, posture | Akathisia: excessive motor activity (e.g., pacing, wringing of hands, inability to sit still) Bradykinesia: psychomotor retardation (e.g., slowing of physical and emotional reactions) Catatonia: immobility with muscular rigidity or inflexibility | NA | Akathisia: anxiety, drug overdose or withdrawal, medication effect, mood disorder, posttraumatic stress disorder, schizophrenia Bradykinesia: depression, medication effect, schizophrenia Catatonia: schizophrenia/psychotic disorder, severe depression |
| Cognitive functioning | ||||
| Attention | Ability to focus based on internal or external priorities | — | Count by sevens or fives Spell a word backward | Attention-deficit/hyperactivity disorder, delirium, mood disorder, psychotic disorder |
| Executive functioning | Ordering and implementation of cognitive functions necessary to engage in appropriate behaviors | Testing each cognitive function involved in completing a task | Oral Trail-Making Test: ask patient to alternate numbers with letters in ascending order (e.g., A1, B2, C3) | Delirium, mood disorder, psychotic disorder, stroke |
| Gnosia | Ability to name objects and their function | — | Show patient a common object (e.g., pen, watch, mobile phone) and ask if they can identify it and describe how it is used | Stroke |
| Language | Verbal or written communication | Appropriateness of conversation, rate of speech (> 100 words per minute is normal; < 50 words per minute is abnormal), reading and writing appropriate to education level | NA | Rapid or pressured speech: mania Slow or impoverished speech: delirium, depression, schizophrenia Inappropriate conversation: personality disorder, schizophrenia Limited literacy skills: depression |
| Memory | Recall of past events | Declarative: recall of recent and past events Procedural: ability to complete learned tasks without conscious thought | When is your birthday? What are your parents' names? Where were you born? Where were you on September 11, 2001? Ask patient to repeat three words immediately and again in five minutes Ask patient to sign their name while answering unrelated questions (each test must be tailored to the individual patient) | Short-term deficit: amotivation, attention-deficit/hyperactivity disorder, inattention, substance use Long-term deficit: amnesia, dissociative disorder |
| Orientation | Ability of patient to recognize their place in time and space | Time, space, person | What year/month/day/time is it? What city/building/floor/room are you in? What is your name? When were you born? | Amnesia, delirium, mania, severe depression |
| Praxis | Ability to carry out intentional motor acts | Apraxia: inability to carry out motor acts; deficits may exist in motor or sensory systems, comprehension, or cooperation | Could you show me how to use this hairbrush/hammer/pencil? | Delirium, intoxication, stroke |
| Prosody | Ability to recognize the emotional aspects of language | — | Repeat “Why are you here?” with multiple inflections (e.g., happy, surprised, excited, angry, sad) and ask patient to identify the emotion Ask the patient to say the same sentence with each of the above emotional inflections | Mood disorder, schizophrenia |
| Thought content | What the patient is thinking | Delusions, hallucinations, homicidality, obsessions, phobias, suicidality | Do you have thoughts or images in your head that you cannot get out? Do you have any irrational or excessive fears? Do you think people are trying to hurt you in some way? Are people talking behind your back? Do you think people are stealing from you? Do you feel life is not worth living? Do you see things that upset you? Do you ever see/hear/smell/taste/feel things that are not really there? Have you ever heard or seen something other people have not? Have you ever thought about hurting others or getting even with someone who wronged you? Have you ever thought about hurting yourself? If so, how would you do it? Have you ever thought the world would be better off without you? | Delusions: fixed delusions, mania, psychotic disorder/psychotic depression Hallucinations: delirium, mania, schizophrenia, severe depression, substance use Homicidality: mood disorder, personality disorder, psychotic disorder Obsessions: obsessive-compulsive disorder, posttraumatic stress disorder, psychotic disorder Phobias: anxiety disorder, posttraumatic stress disorder Suicidality: depression, posttraumatic stress disorder, substance use |
| Thought processes | Organization of thoughts in a goal-oriented pattern | Circumferential: patient goes through multiple related thoughts before arriving at the answer to a question Disorganized thoughts: patient moves from one topic to another without organization or coherence Tangential: patient listens to question and begins discussing related thoughts, but never arrives at the answer | Generally apparent throughout the encounter | Anxiety, delirium, depression, schizophrenia, substance use |
| Visuospatial proficiency | Ability to perceive and manipulate objects and shapes in space | — | Ask patient to copy intersecting pentagons or a three-dimensional cube on paper Draw a triangle and ask patient to draw the same shape upside down | Delirium, stroke |
Delirium is common but frequently overlooked, and is associated with serious medical conditions; therefore, assessment for delirium should always be considered in patients with acute AMS, especially in those at high risk(Table 4).6,9,11 The Confusion Assessment Method is a widely used, validated tool to identify delirium with a high sensitivity (94% to 100%) and specificity (90% to 95%)11 (Table 56). The 4 A's test is also a reliable screening tool (sensitivity of 89.7% and specificity of 84.1%) and is available at https://www.mdcalc.com/4-test-delirium-screening.11 The ultra-brief test requires only two questions—What is the day of the week? and Name the months of the year backwards—and has a sensitivity of 93% and specificity of 64%. The high sensitivity makes it useful to rule out delirium when both questions are answered correctly, but a positive test (i.e., incorrect answers) requires confirmation with a tool such as the Confusion Assessment Method.11,19
| Age older than 65 years Anesthesia Baseline cognitive impairment Baseline poor functional status Change in environment Constipation and/or urinary retention Dehydration Depression History of alcohol misuse History of delirium Intensive care unit stay Malnutrition Medical illnesses (e.g., heart, lung, liver, kidney) Polypharmacy Sleep deprivation Social isolation Surgery Tethers (e.g., urinary catheter, intravenous tubing) Visual or hearing impairment |
| (1) Acute onset and fluctuating course Is there evidence of an acute change in mental status from the patient's baseline? Did this behavior fluctuate during the past day (that is, did it tend to come and go or increase and decrease in severity)? (2) Inattention Does the patient have difficulty focusing attention; for example, being easily distracted or having difficulty keeping track of what was being said? (3) Disorganized thinking Is the patient's speech disorganized or incoherent; for example, rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject? (4) Altered level of consciousness Overall, how would you rate this patient's level of consciousness: alert (normal); vigilant (hyperalert); lethargic (drowsy, easily aroused); stupor (difficult to arouse); coma (unarousable)? |
A thorough medication history, including new or recent changes in prescription medications, over-the-counter medications, herbal products, and nutritional supplements, is essential. Consulting the patient's pharmacy may help with this task. Comorbid medical conditions, recent surgeries or procedures, and the use of alcohol and recreational drugs can increase the risk of or cause AMS and should be identified.2,3,9,10
Other aspects of the history should focus on associated symptoms or events of infection, trauma, neurologic changes, and headaches, any of which might identify a precipitating cause. A complete review of systems may uncover additional factors (e.g., constipation, urinary retention) contributing to AMS.2,3,9,10
PHYSICAL EXAMINATION
The neurologic examination is important to identify AMS and determine the cause. In addition to the mental status examination, cranial nerves, motor function, reflexes, sensation, and coordination should be evaluated. Focal abnormalities can suggest intracranial pathology such as stroke, neoplasm, or demyelinating conditions. If a patient is exhibiting asterixis, it suggests metabolic encephalopathy.1–3,10,12
Attention to eye and vision abnormalities can also provide important diagnostic clues. Visual field defects can indicate a stroke. Pupillary abnormalities may be present with substance abuse, stroke, or pending cerebral herniation. The ability to perform extraocular movements may differentiate a suspected comatose patient from one with a locked-in syndrome. Ophthalmoplegia is an important finding of Wernicke encephalopathy, and nystagmus can identify drug intoxication or stroke. Papilledema suggests increased intracranial pressure.2,3,10
Examination of the head, ears, nose, and throat should focus on signs of trauma and infection. When examining the neck, thyroid abnormalities and meningismus are important findings that suggest thyroid disorders and nervous system infections, respectively. Examination of the heart, lungs, and abdomen can indicate important systemic causes of AMS, such as heart failure, pneumonia, and decompensated hepatic disease.2,3,10
Examination of the skin can show signs of chronic systemic disease (e.g., jaundice), systemic infection (e.g., petechiae), or local infection with cellulitis or abscess, or locate medication patches. A musculoskeletal examination may identify inflamed joints indicating infection or an autoimmune condition.2,3,10
TESTING
The history and physical examination guide diagnostic testing; however, the following initial tests can be considered for all patients with AMS when the diagnosis is not clear: complete blood count, electrolytes, liver function tests, serum ammonia, blood urea nitrogen, creatinine, phosphorus, magnesium, blood gas analysis, thyroid testing, blood culture, urinalysis, viral antigen or polymerase chain reaction tests when community prevalence is high, toxicology screening, chest radiography, and electrocardiography. 2,3,10
Considering that the above tests are noninvasive and relatively inexpensive, they should be used liberally, especially when the etiology is not clear from the history and physical examination. Additional tests to consider when initial evaluation is not diagnostic are adrenal function, erythrocyte sedimentation rate, C-reactive protein, extended toxicology screening, and serologic testing for autoimmune disorders.2,3,10
NEUROIMAGING
Unless the etiology is clear and the risk of intracranial pathology is low, neuroimaging should be included in the initial assessment of recent AMS.12–14 Patients with trauma, anticoagulation, hypertension, hypertensive emergency, headache, nausea or vomiting, clinical concern for infection, new-onset seizure, neurologic findings on examination, history of cancer, older age, and a known intracranial process all require imaging. Neuroimaging should be performed in patients who did not previously receive imaging and in whom initial therapy has failed. In patients with new-onset delirium, imaging should be considered if there is no other obvious precipitating cause.13
Noncontrast computed tomography (CT) of the head is the initial study for most patients. Noncontrast CT is widely available, can be completed quickly, identifies most pathology requiring urgent intervention, and is better tolerated by patients than magnetic resonance imaging (MRI). If MRI is available and tolerated by the patient, it can also be the initial imaging study and is preferred to CT if the progression of an inflammatory process (e.g., multiple sclerosis) is suspected. Contrast is helpful when infection, tumor, inflammatory pathology, or vascular abnormalities are suspected.13–15
MRI should be considered when CT was the initial study but was not diagnostic; it can detect pathology not evident on CT such as acute, minor, or posterior circulation ischemia, encephalitis, subtle subarachnoid hemorrhages, and inflammatory conditions. MRI may also be indicated to better define pathology found on CT.13–15
LUMBAR PUNCTURE
Lumbar puncture can help identify several causes of AMS, including meningitis, encephalitis, subarachnoid hemorrhage, autoimmune conditions, and metastases to the subarachnoid space. When there is clinical suspicion for meningitis, a lumbar puncture is mandatory. Standard testing of cerebrospinal fluid includes a cell count with differential, protein, glucose, and culture. Obtaining additional fluid for freezing is prudent because other testing may be needed.2,3,20
ELECTROENCEPHALOGRAPHY
Electroencephalography is an important study to rule out nonconvulsive seizures, which may occur in 8% to 30% of patients with AMS without an obvious cause.16 It can also help diagnose metabolic encephalopathy and infectious encephalitis.17,18 A normal electroencephalogram may help exclude a suspected seizure disorder and support a primary psychiatric cause of AMS.
PATIENTS WITH UNDERLYING DEMENTIA
Patients with dementia have an increased risk of AMS.6,9,11 Clinicians are often challenged to determine if deficits are chronic or new, and substantial efforts should be made to identify the patient's baseline status. Clinicians should balance the risk of unnecessary testing and intervention for chronic situations the clinician may be unaware of vs. missing a new treatable condition causing AMS. Advance directives and input from the family can help guide evaluation and treatment decisions.
A common pitfall for patients with dementia who are in a care facility is inappropriately attributing AMS to a urinary tract infection. Many patients who are institutionalized have asymptomatic bacteriuria, and treatment is not indicated unless a urinary infection with symptoms is present.22 Management should focus on identifying other causes for the patient's AMS.
Prevention
When patients are at risk of AMS, particularly for delirium, nonpharmacologic preventive measures can decrease incidence, especially in those who are hospitalized.6,9,11 The use of multiple measures through a multidisciplinary team approach is most effective. There is no convincing evidence to support the use of medications to prevent AMS or delirium.6,9,11
Treatment
Definitive therapy for AMS is treatment of the underlying causes or the removal of precipitating agents. However, when patients' behaviors threaten themselves or others before a reversible cause can be identified or fully treated, intervention is needed to avoid harm. In these situations, nonpharmacologic interventions are the treatment of choice.2,3,6,10,11
NONPHARMACOLOGIC TREATMENTS
Reassurance and use of de-escalation techniques by staff, family, or friends can be effective. Reducing artificial lighting and other environmental stimuli such as monitoring alarms can also help calm patients. A family member or assigned staff can stay at the patient's bedside to ensure that patients do not harm themselves. Additional measures include those used for AMS or delirium prevention (Table 66,9,11).
| Adequate hydration Adequate nutrition Adequate oxygenation Avoid constipation Avoid tethering (intravenous lines, monitors, Foley catheter) Cognitively stimulating activities Early mobilization Ensure patient has assistive devices (eyeglasses, hearing aids, mobility devices) Geriatric specialty consultation Infection prevention Limit psychoactive medications Pain management Presence of family and caretakers Orientation (accurate calendars and clocks, and appropriate lighting; reorientation by staff and family) Sleep enhancement measures (avoid nighttime disturbances, use appropriate lighting, reduce noise at night) |
MEDICATION
Medication to manage behaviors associated with AMS should be used only when nonpharmacologic measures are not effective, and then only when it is essential to control behavior. Studies evaluating the effectiveness of medications used for their sedative effects yield conflicting results and may cause harm due to adverse effects.11,23,24 Antipsychotics have historically been used off-label to treat delirium; however, a recent systematic review does not support the use of these agents in hospitalized adults with delirium.24 Anti-psychotics also carry a U.S. Food and Drug Administration boxed warning about an increased risk of death when used in older adults with dementia-related psychosis.
Benzodiazepines should generally be avoided unless they are being used to treat alcohol withdrawal or seizures because they may worsen delirium. For any agent, the lowest effective dose for the minimum time necessary should be used. Medications used when nonpharmacologic modalities fail are listed in eTable A.
| Drug | Dose* and route | Maximum daily dosage | Onset | Treatment considerations |
|---|---|---|---|---|
| Antipsychotics | FDA boxed warning: increased mortality in older patients with dementia-related psychosis Adverse effects: extrapyramidal symptoms, QTc prolongation, increased risk of falls, aspiration | |||
| Droperidol | 2.5 to 10 mg IV | 20 mg | 3 to 10 minutes | |
| 5 to 10 mg IM | 20 mg | 3 to 10 minutes | ||
| Haloperidol | 0.5 to 1 mg orally every four to six hours | 30 mg | 15 to 30 minutes | |
| 0.5 to 1 mg IM/IV every 30 to 60 minutes | 30 mg | 5 to 20 minutes | ||
| Olanzapine (Zyprexa) | 5 to 10 mg IM | 30 mg | 15 minutes | |
| 2.5 to 5 mg orally | 20 mg | 30 to 60 minutes | ||
| Quetiapine (Seroquel) | 12.5 to 25 mg orally | 150 mg | 15 to 45 minutes | |
| Ziprasidone (Geodon) | 5 to 10 mg IM | 40 mg | 15 minutes | |
| Benzodiazepines | May worsen delirium Generally reserved for alcohol withdrawal and seizures | |||
| Lorazepam (Ativan) | 0.5 to 2 mg IM/IV/orally | 10 mg | 3 to 5 minutes | |
| Midazolam | 2 to 5 mg IM/IV | 20 mg | 1 to 10 minutes | |
| Ketamine | 0.5 to 1 mg per kg IV | 200 mg | 0.5 minutes | Use caution in patients with cardiovascular disease; may increase blood pressure and heart rate |
| 4 to 5 mg per kg IM | 500 mg | 3 to 4 minutes |
Data Sources: PubMed (including use of the Clinical Queries feature), the Cochrane Database of Systematic Reviews, Essential Evidence Plus, and UpToDate were searched using the key terms altered mental status and encephalopathy. Also searched were specific etiologies of altered mental status. Search dates: January 19 to February 22, 2021, and August 20, 2021.
