How Family Physicians Can Privately Seek Treatment for Depression
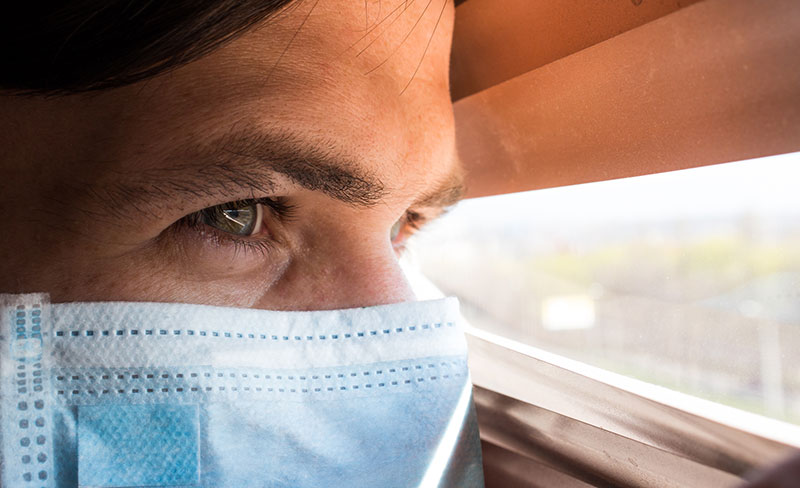
As family physicians, we thrive on the hustle and bustle of our profession. The fast pace of practice and variety of cases presented each day are just some of the reasons we decided to go into family medicine. The rewards are often tremendous. However, maintaining a hectic pace may, at times, lead to lows that test our perseverance. Additionally, the COVID-19 pandemic has presented a multitude of new challenges for family physicians, including rapidly changing patient care protocols and the loss of patients, colleagues, friends, and family to the virus. You may now find your lows are more consistent. You may even find yourself sliding into depression.
We know depression is a mental health disease. It’s common. It’s serious. It can affect anyone, even family physicians. Between 15% and 18% of physicians report being depressed in the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
As a physician, you may realize it’s time to seek professional treatment for your own depression but there may be professional consequences holding you back, such as the stigma felt from colleagues, the lack of confidential resources, and the viability of obtaining future practice insurance if you do so. Additionally, mental health treatment may impinge on the ability to obtain a future medical license as many states inquire about mental health treatments on licensing applications. Many of us believe these questions are out of compliance with the Americans with Disabilities Act (ADA) and its protection from employment discrimination for individuals who have or who have had a history of mental illness. Fortunately, some associations are leading the charge to advocate for physician well-being and change these tactics. So, I encourage you, now more than ever, to put aside your concerns and seek the help that’s available to treat your disease.
Addressing family physician depression at the state level
Professional medical associations, including the American Medical Association (AMA), are supporting family physicians and their rights to seek mental health treatment, without fear. In 2018, the AMA adopted a policy focused on providing physicians easier access to mental health care. The policy’s aim is to create an environment where treatment doesn’t carry the stigma nor negatively impact licensure or professional advancement of physicians. Additionally, the AMA is working with state medical licensing boards to encourage them to revise questions presented on state licensing applications to only require disclosure about current or currently untreated mental health conditions. Likewise, the association also is encouraging state boards to remove application questions that deal with past mental health illness. Some states are responding to this call and are working to make positive changes.
While these are steps in the right direction, it’s a slow process. Thankfully, there are other treatment options available today.
Treating family physician depression through an EAP
Help may be as close as your practice group if it offers an Employee Assistance Program (EAP). One of the reasons EAPs exist is to provide treatment and resources for mental health conditions before they negatively impact your work. When you contact your EAP, you’ll be connected with a counselor who will help guide you through the process. Additionally, strict state and federal regulations require confidentiality within EAPs; so, you can be open and honest with your counselor without fear of your employer finding out what’s discussed or that you’ve even contacted the service.
If you’re looking for additional privacy, ask if your EAP offers a telemedicine option. If so, you could speak with your counselor from your choice of discreet locations.
Note, however, if you’re referred to an EAP by your employer, your employer will be entitled to the details of your counseling sessions. Please be proactive and contact the EAP on your own before your employer notices adverse changes in your work.
Treating family physician depression through pharmacotherapy
If you suffer from moderate to severe depression, you may find that pharmacotherapy provides the relief you need. Seek care from a mental health professional who can properly evaluate you to see if medication is right for your treatment plan.
Treating physician depression through a PHP
Another way you can find help is through a Physician Health Program (PHP). Most states offer PHPs, and a list of programs can be found on the Federation of State Physician Health Programs (FSPHP) website. Unaffiliated with hospitals or medical groups, many of these programs are supported through legislative action and are exempt from required reporting. This affords them the biggest luxury — the ability to offer confidentiality.
One of the principles of the FSPHP states that the “privacy and confidentiality of a physician’s health and treatment history must be paramount in the relationships between PHPs and ill physicians … to allow those in need of help to come forward without fear of punishment, disciplinary action, embarrassment, or professional isolation. Confidentiality enhances the opportunity for recovery, and incentive to participate in early intervention.” That speaks volumes.
When you contact a PHP, you’ll be evaluated and presented with treatment options right away. But it’s not just a quick fix. PHPs are in it for the long haul with you through follow up and regular monitoring.
Treating family physician depression through medical colleagues
As your physician colleagues, we understand your stress more than anybody else. Reach out to one of us — for advice, resources, or just to talk. You may find you’re not alone. If you would rather speak with a peer you don’t know, call the Physician Support Line at 888-409-0141. It’s a free and confidential resource that is staffed by volunteer psychiatrists who specialize in mental health wellness. The service is available from 8 a.m.-1 p.m. (EST) daily. Additionally, its website offers resources you can use on your own.
If you’re feeling depressed right now and considering suicide, reach out for help immediately. Contact the National Suicide Prevention Lifeline at 800-273-8255 (TALK).
Resources are available to help you get back to a successful and healthy—and hopefully not as stressful—professional life.
Resources
- American Medical Association – Physician Health
- Federation of State Physician Health Programs – State Programs
- American Academy of Family Physicians: Physician Health First
- Physician Support Line
- National Suicide Prevention Lifeline