
The difference between one level and the next may be no more than a word or two.
Fam Pract Manag. 2010;17(2):22-27
Kent Moore is the AAFP's manager for health care financing and delivery systems and is a contributing editor to FPM. Author disclosure: nothing to disclose.

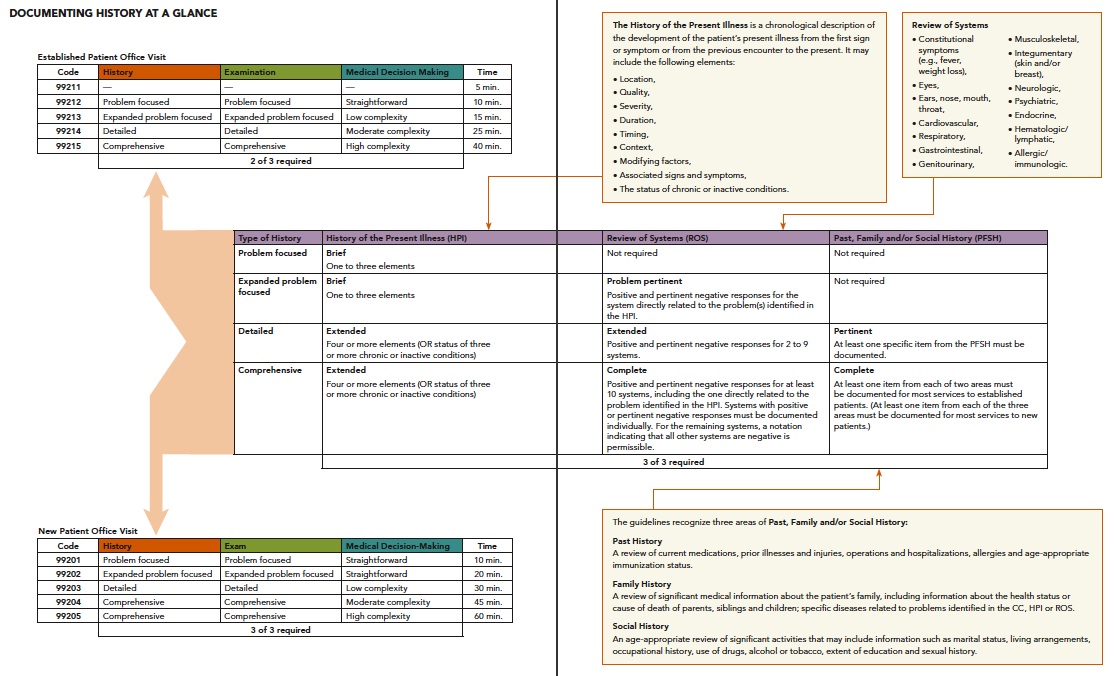
Sixteen years have passed since the Health Care Financing Administration (HCFA) first put physicians on notice about the kind of medical records they would be asked to produce to back up claims considered questionable by Medicare carriers. The “Documentation Guidelines for Evaluation and Management Services,” which HCFA (now the Centers for Medicare & Medicaid Services, or CMS) developed with input from the American Medical Association and medical specialty societies, establish parameters for the history, exam and medical decision making documentation required to justify billing each level of E/M service. This article, the first in a three-part series on the documentation guidelines, reviews the guidelines for history and describes how to use them to your advantage.
You don't have to do it all yourself
Oddly enough, the guidelines for history begin by explaining what physicians aren't required to do. For example, one of the most useful things the guidelines make explicit is the extent to which you can delegate the task of gathering history to ancillary staff and to patients themselves. One guideline puts it this way:
The Review of Systems and the Past, Family and/or Social History may be recorded by ancillary staff or on a form completed by the patient. To document that the physician reviewed the information, the physician must add a notation supplementing or confirming the information recorded by others.
The omission of the History of the Present Illness (HPI) here seems to imply that it may not be similarly delegated. Some Medicare carriers have established their own policies requiring physicians to perform the work of the HPI, although interpretations of these policies may differ.
Another helpful guideline stipulates that, once you've gathered the information, you do not have to repeat the entire Review of Systems (ROS) and Past, Family and/or Social History (PFSH) at each subsequent visit:
An ROS and/or a PFSH obtained during an earlier encounter does not need to be rerecorded if there is evidence that the physician reviewed and updated the previous information. This may occur when a physician updates his or her own record or in an institutional setting or group practice where many physicians use a common record. The review and update may be documented by:
describing any new ROS and/or PFSH information or noting there has been no change in the information; and
noting the date and location of the earlier ROS and/or PFSH.
Now, turn to the overview of the history guidelines. These tables provide detailed descriptions of the elements that, according to the most recent (1997) version of the guidelines, should be comprised by the HPI, ROS and PFSH. See “The guidelines in context” to learn how the guidelines have evolved since the first (1995) version was released.
The HPI
The 1995 guidelines specify only eight elements of the HPI (location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms), all of which pertain largely to acute problems. They define an extended HPI as having four or more of these elements and a brief HPI as having one to three of them.
This definition tends to undervalue the HPI for follow-up visits with patients who have multiple chronic problems. If the problems are well-controlled – enough for the patient to be asymptomatic – even the most careful and thorough HPI might not be able to turn up four or more of the specified elements. (How do you give the duration of a symptom that isn't there?) As a result, this definition of the HPI tends to put a ceiling on the level of the visit: A brief HPI limits the level of history to problem focused or expanded problem focused, and that limits the level of a follow-up visit to 99213 unless both the exam and the medical decision making are involved enough to justify a higher level without reference to the history.
To address this concern, the 1997 version of the guidelines redefined the extended HPI as four or more elements of the HPI or the status of three or more chronic or inactive conditions.
Because of this addition, some physicians might be tempted to combine the 1997 guidelines for history and medical decision making with the 1995 guidelines for exam, which some say are easier to use than their expanded 1997 counterpart. It's important to note, however, that CMS has permitted the use of either set of guidelines, but not a combination of the two.
Dancing on the threshold
As you may have noticed on the overview chart, the thresholds dividing the different types of history are quite explicit. And each threshold is defined in terms of the number of items listed in the documentation. For instance, in terms of documentation, the only difference between a problem-focused history and an expanded problem-focused history is a problem-pertinent ROS: the documented review of one system. Other such thresholds (the differences between expanded problem-focused and detailed histories, and between detailed and comprehensive histories) involve documentation of additional items in two or three of the components of the history.
Study of the chart will help make the distinctions clear in your mind: what makes the difference between one level of HPI, ROS or PFSH and another – and when that difference makes a difference in the overall type of history.
In the HPI and PFSH, the difference between one level and the next may be no more than a word or two. For instance, the guidelines define a brief HPI as including documentation of one to three elements (location, quality, severity, etc.) of the present illness. Add a fourth element, and you have an extended HPI. Clearly, it does not take much to differentiate a brief HPI from an extended one. Here's an example of a brief HPI: “Patient has an intense [ severity], throbbing [ quality] pain in the neck [ location].” Add duration to the mix, and you now have an extended HPI: “Patient has had an intense, throbbing pain in the neck since yesterday.”
The guidelines indicate a similarly small difference between a problem-pertinent ROS and an extended ROS. For a problem-pertinent ROS, you need only document a review of the system directly related to the problem or problems identified in the HPI. By comparison, the correct documentation of an extended ROS demonstrates inquiry about two to nine systems, one of which is the system directly related to the problem identified in the HPI. For example, let's say the problem identified in the HPI is a common cold, and you document review of the ears, nose, mouth and throat. At this point, you have documented a problem-pertinent ROS. Note, however, that if you also document that you reviewed the respiratory system, you have documented an extended ROS.
A related point: To correctly document a complete ROS, you must show that you have reviewed at least 10 organ systems, one of which is the system directly related to the problem identified in the HPI. However, you do not have to individually document all the systems reviewed; you only have to document those with a positive or pertinent negative response if you document a review of the remaining systems with a notation like “all others negative.”
For example, if you see an elderly patient with severe chronic obstructive pulmonary disease, congestive heart failure and hypertension, you do not need to individually document all the systems reviewed. Instead, you could document the positive or pertinent negative responses for the relevant systems and then simply note, “all others negative,” if appropriate, to cover the other systems reviewed.
Finally, as you document HPI, ROS and PFSH, you should keep medical necessity in mind, as it is the “overarching criterion for payment in addition to the individual requirements of a CPT code,” according to CMS.1
THE GUIDELINES IN CONTEXT
In 1992, when the Health Care Financing Administration (HCFA) replaced the old customary and reasonable fee methodology with the new Medicare Fee Schedule incorporating the resource-based relative-value scale (RBRVS), the AMA CPT Editorial Panel created new E/M codes in an attempt to better standardize physician coding for these services. Because of the enormity of the task of implementing an entirely new payment schedule for every physician in the country, HCFA elected not to simultaneously develop and promulgate guidelines for documenting the new codes.
It quickly became apparent, however, that although physician coding for E/M services was growing more consistent under the new system, some physicians tended not to use the full range of the new E/M codes. Physicians' uncertainty about the documentation required to support various levels of service and E/M codes, and carriers' desire for a yardstick for reviewing claims, led HCFA to begin developing documentation guidelines for E/M services.
The “Documentation Guidelines for Evaluation and Management Services” caused a minor stir when they were implemented in 1995. When revised guidelines were released in 1997, widespread concern about their complexity led HCFA to grant a request from the AMA to extend the grace period for implementation by six months, to June 30, 1998. Ultimately, the revised guidelines were implemented without changes, but as an alternative to, rather than as a replacement for, the 1995 version, which remains in force.
The documentation guidelines also have relevance outside of Medicare. Most payers tend to follow Medicare's example.
Putting it all together
Let's take one established patient – an adult male with the chief complaint (CC) of cough with green sputum for seven days – to illustrate the differences in documentation required for history at three different levels of service. To begin with, suppose the documentation of history for this visit read as follows:
The first sentence gives the chief complaint and four elements of the HPI (quality, severity, associated signs and symptoms, and duration). The rest of the paragraph documents the ROS for three systems (constitutional symptoms; ears, nose, mouth and throat; and respiratory). The second paragraph documents elements from two areas of the PFSH. As you can see from the summary table, this constitutes a detailed history, which would support a 99214 code assuming the documentation also included a detailed exam or moderate complexity decision making, since two of the three key components determine the overall level of service.
What if the documentation had been less complete? If the second paragraph had been omitted entirely, leaving no PFSH, the type of history documented would have been reduced to expanded problem-focused. (Note, however, that including either of the points made in this paragraph would be enough to raise the type of history to detailed.)
Similarly, if less of the HPI had been included – even a couple of words less – the type of history would have decreased. If both paragraphs had been included, but the first sentence had read, “CC: cough; patient has had a cough with green sputum for seven days,” the HPI would have dropped from extended (four elements) to brief (one to three elements), and the type of history would have dropped with it. Despite the lower level of history, if the exam and medical decision making were detailed and moderate complexity, respectively, it would still be possible to code 99214. Otherwise, the level of service would drop to 99213.
What if the history portion of the note had read simply, “CC: cough; patient has had a cough for seven days”? While not including enough detail to characterize the patient's situation clearly, it does include the chief complaint and one HPI element, and would therefore qualify as a problem-focused history, which would be consonant with a 99212, assuming at least a problem-focused exam or straightforward decision making.
For new patients, the documentation thresholds are particularly important to keep in mind because all three key components – history, exam and decision making – determine the overall level of service. The difference between a three- and a four-element HPI could mean the difference between an expanded problem-focused history and a detailed history – and between billing a 99202 and a 99203.
One final note about documenting history: The guidelines refrain from defining how a note should be organized. Our sample note, with the history components lumped together, might well give a chart reviewer pause, but there's no harm in that. Here's what the guideline says: The CC, ROS and PFSH may be listed as separate elements of history, or they may be included in the description of the HPI.
