Direct primary care will continue to grow because it empowers price transparency, quality, and patient satisfaction.
Fam Pract Manag. 2016;23(5):12-14
Author disclosure: Dr. Eskew discloses that he has an ownership stake in DPC Frontier, a free DPC online resource; is an employee and officer of ProactiveMD, which offers DPC services to employers; and is on the speakers' bureau for Access Healthcare, where he occasionally speaks at CME events.
See the related editorial: “Is Direct Primary Care the Solution to Our Health Care Crisis?”
They charge a periodic (monthly or annual) fee for a defined set of primary care services,
They do not bill any third parties on a fee-for-service basis for the services covered by the periodic fee,
Their per-visit charges are less than the monthly equivalent of the periodic fee.
DPC practices differ considerably from concierge practices in both legal design and practice operation.2 Pure DPC practices do not bill any forms of traditional insurance, and this lowers practice overhead and allows these physicians to spend more time with the patient rather than wasting time on busy work requested by insurance companies. In contrast, concierge practices “double dip” by continuing to bill in a traditional fee-for-service fashion and by charging a membership fee. Overhead in a concierge practice is not reduced, and these physicians must be willing to spend less time with patients who decide not to pay their monthly fees, which are usually much higher than DPC monthly fees. Ignorance of the distinction between DPC and concierge models is often a source of attack against DPC,3 which I have addressed elsewhere.4
This article will address three common misconceptions about and criticisms of the DPC model.
1. Is direct primary care legal?
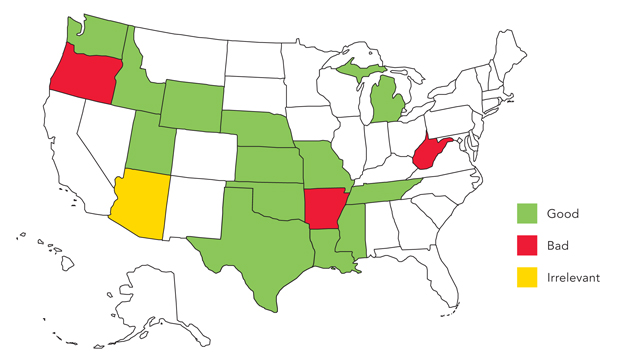
Yes, DPC is “not insurance” (since there is no risk transfer), and legal DPC contracts can be drafted in every state. As of Aug. 16, 2016, 17 states have passed laws related to direct primary care. (See “Direct primary care laws by state.”) Most of the state legislation is motivated by a desire to define DPC as “not insurance” so that the state insurance commissioner does not feel obligated to prohibit or regulate the practice model. DPC is arguably legal in every state without this legislation, but legislation is often helpful because it clears up legal gray areas and thus removes barriers to physician adoption of the model.
Each of the 17 state laws include a variety of patient protections. They generally require practices to state that the DPC agreement is “not insurance,” to permit patients to end the agreement at any time without owing additional fees, and to describe the scope of services offered so patients understand what is being purchased.
At the national level, the Affordable Care Act defines and encourages DPC as well. It allows insurance companies to develop “wrap around” insurance plans designed to be coupled with DPC and sold in a bundled fashion in state insurance exchanges so that they may be compared to traditional insurance plans in an “apples to apples” fashion.
The DPC model is easily understood and enjoyed by patients, and my research has not discovered a single malpractice claim from a DPC patient. For example, although the Washington State Insurance Commissioner was skeptical of the DPC model when it was established in the state in 2007, his office's “Direct Practice Annual Report to the Legislature” found no formal or informal patient complaints filed against the 33 practices serving 11,504 patients.5 Unlike traditional insurance, which can feel like an arranged marriage between the patient and physician, the DPC model involves mutual selection by the patient and physician, and the physician is not incentivized to limit care. If the patient perceives a lack of value, he or she may end the relationship at any time.
2. How does DPC affect the physician shortage?
This is the most common public policy criticism of DPC. If you consider that a DPC physician's panel size is anywhere from 400 to 1,200 patients, in my observation, and an average traditional panel size is 2,300 patients,6 the logical assumptions are that 1) less total care is delivered and 2) more primary care physicians are needed. The first assumption is false, as I will demonstrate, but I will admit that in the short term DPC may exacerbate the primary care physician shortage by increasing patient utilization of primary care services. However, this effective use of primary care decreases the burdens placed on the rest of the health care system and highlights the real problem: a physician maldistribution problem, with an overabundance of specialists.7 With the growth of DPC and a more effective use of primary care, the number of specialty referrals would fall and the gap between primary care and specialty physician compensation would eventually shrink, incentivizing more physicians to enter primary care.
What does it mean to offer more primary care? DPC physicians spend an average of 35 minutes with the patient at each visit and average around four visits per patient per year.2 Even if we ignore the countless touch points that occur between DPC physicians and patients via email, text, and phone, the amount of physician time spent with the patient in a DPC practice is higher than in the typical primary care fee-for-service practice, where the average visit is 20 minutes in duration8 and patients average 1.66 visits per year.9 DPC physicians have time to obtain a detailed history and then conduct medical research so that they may offer comprehensive primary care. Studies have shown that comprehensive primary care is associated with higher quality and lower costs by decreasing utilization throughout the remainder of the health care system.10 Studies have also shown that practices with panel sizes of 2,500 do not allow primary care physicians the time required to follow USPSTF preventive guidelines.11
Increasing use of the DPC model improves patient access to care because it offers more care. DPC physicians literally provide more care to the patient (an average of 140 minutes of care per year compared with 33 minutes per year in a traditional practice, according to the figures cited earlier). DPC also improves physician recruitment and retention. Medical students would notice that primary care can thrive, aging physicians could pursue DPC rather than retiring, and even specialists could be attracted to primary care.12 The only place I have seen dermatologists envious of family physicians was at a DPC conference.
3. How does DPC affect disparities in care and health system utilization?
DPC achieves price transparency, and price transparency increases access to care, decreases disparities in care, and decreases waste within the system. Price transparency starts with the DPC practice, where the patient fee is around $70 per month. Many established DPC physicians can direct patients to facilities that offer MRIs in the range of $400,13 discounted labs are the norm, and specialists are beginning to cater to DPC practice requests for transparent pricing as well. The Surgery Center of Oklahoma, for example, has listed all-inclusive prices for almost any outpatient surgical procedureon its website since 2009.
DPC patients visit emergency departments, urgent care clinics, and specialists less frequently than traditional patients and, therefore, are less of a burden on the rest of the health care system.14 While hospital systems form narrow networks that patients hate, DPC physicians form narrow networks that patients prefer. DPC physicians are in a position to know which other specialists in the community are worth seeing. They receive and have time to read the consult notes and can judge the outcome of each referral or requested procedure. Patients trust DPC physicians to send them to an effective specialist when needed.
A growing model
Although many obstacles remain, I anticipate continued adoption and expansion of DPC across the country. Evidence of this growth can be found in the DPC Mapper, where most practices are “pure” DPC practices, meaning the physicians see patients in the DPC setting only, rather than using a hybrid model,1 which many find to be unnecessary or unhelpful. DPC has received support from many organizations (for example, the American Academy of Family Physicians, the American College of Osteopathic Family Physicians, and the Family Medicine Education Consortium have hosted two DPC Summits, and two recent pieces of state DPC legislation passed without a single nay vote in Wyoming15 and Nebraska.16 The DPC model will continue to grow because it has the power to save our health care system. Why not give it a chance rather than watching from the sidelines?