
These practical strategies can help family physicians support patients with depression, anxiety, and other behavioral health issues.
Fam Pract Manag. 2017;24(2):30-35
Author disclosure: no relevant financial affiliations disclosed.

Consider this: About three-quarters of the patients on your schedule today likely have a clinical problem with a significant psychological or behavioral component.1 Most patients with psychological issues seek help from you, their primary care physician, not from a specialty mental health provider.2,3 Furthermore, caring for patients' emotional well-being plays an important part in preventing, diagnosing, and treating the top 15 causes of death in the United States.4
One of the most commonly used treatment approaches for psychosocial problems and emotional distress is psychiatric medication. Although practice guidelines support the use of antidepressants for severe depression in adults, greater controversy exists about their effectiveness, acceptability, potential risks, and safety in other groups (e.g., children or patients with mild or moderate depression). Further, some patients do not want medications for a variety of reasons such as stigma, cost, side effects, and drug interactions. As a result, family physicians often need additional tools for addressing patients' behavioral health needs.
In many practices, embedded behavioral health providers work alongside family physicians, helping patients with a broad range of issues including depression and anxiety, medication adherence, chronic pain, smoking cessation, weight loss, and chronic illness management. Although these integrated models are growing, it's imperative for family physicians to have a toolbox of skills for managing behavioral health issues independently, for several reasons. First, even in fully integrated clinics, behaviorists are not always available; limited funding may preclude sufficient staffing of positions, and behaviorists often have multiple demands on their time. Second, some patients are not willing to see a behavioral health provider, often due to the stigma surrounding mental illness. Third, family physicians who work in rural areas may lack adequate behavioral health referral sources or encounter the challenges associated with dual relationships in small towns. Finally, some insurance plans don't cover behavioral health services or have high deductibles and out-of-pocket costs for these services, making psychotherapy practically inaccessible.
This article shares six specific tools primary care physicians can use to help them care for patients with behavioral health care needs.
Six five-minute tools
Working with patients in severe emotional distress can be exhausting and overwhelming. Physicians may feel a responsibility to “fix” their patients' pain, but of course there are no quick solutions for life stressors and mental illness. Introducing one of the following behavioral health tools may seem like a small step, but it can plant a seed of hope for the patient and bolster the physician's sense of efficacy. None of these tools immediately ameliorates patient suffering and life stressors, but all of them can make a positive difference when provided in a caring environment (see “Being present with distressed patients”). Importantly, all of these skills can be taught to patients in less than five minutes, and you can select the tool that is most appropriate for the particular patient.
BEING PRESENT WITH DISTRESSED PATIENTS
Sometimes, the most important skills to use with your distressed patients are not diagnostic, technical skills but your emotional availability and compassion:
Be present and allow yourself to be emotionally available,
Use appropriate physical touch and open body language (turning away from the computer, for example),
Listen without interruption and judgment, and employ active listening skills such as paraphrasing and reflecting patients' feelings,
Instill hope and empower the patient by eliciting how he or she successfully coped with similar challenges in the past,
Express empathy in a genuine, natural manner, thereby fostering a stronger patient-provider relationship.
1. Encourage the patient to draw on social supports. An initial approach to many patients' behavioral health concerns may be to draw on existing social supports. Ask the patient, “Who do you have in your life to support you in dealing with [fill in the clinical issue]?” Social supports may include family, friends, support groups, religious groups, and 12-step programs. Encouraging patients to draw on social supports may not be effective for very isolated patients. However, if the patient is interested in broadening his or her social network, consider searching online together during the visit so the patient can leave with contact numbers or websites for volunteer opportunities, social groups, community education classes, faith-based resources, or other local resources.
2. Increase the frequency of visits with you. For patients who are reluctant to see a therapist due to stigma, cost, or other concerns, increasing visit frequency with you, their family physician, can be a mechanism to offer support. Sometimes primary care physicians minimize the importance of their role and their ability to support patients with behavioral health concerns. However, you may be the only person with whom the patient can openly share his or her distress and experience supportive, nonjudgmental listening. More frequent contact can strengthen trust, respect, and comfort in the doctor-patient relationship, which may increase the patient's openness to more intensive intervention in the future, such as medication, therapy, or a specialty referral.
3. Assist the patient in focusing on gratitude. Focusing on positive life events (big or small) is a tool you and the patient can employ easily in a primary care setting, and it is especially effective for patients with depression and anxiety symptoms. Some experts recommend daily gratitude journaling, while others indicate that documenting sources of gratitude even once per week can boost mood. Regardless of the frequency, writing or recording these thoughts in some way appears to be beneficial, perhaps because it creates some accountability and room for reflection. Reflecting on even small positive events, such as a smile from a stranger, the laughter of a child, or a good meal can be easy places to start. Reviewing this journal with the patient periodically may help you identify his or her values and goals, which you can then use in motivational interviewing to elicit other behavior change.
4. Teach breathing and mindfulness exercises. Simple breathing exercises can be useful for many patients in managing anxiety, depression, and generalized life stress. For example, physicians can teach a four-count breathing technique, wherein patients breathe in for four counts, hold their breath for four counts, blow out gently for four counts, and then hold the empty breath for four counts. Physicians can quickly model this technique in the clinic visit and encourage regular practice. Patients will find the skill more useful if they have rehearsed it during calm, non-crisis times. Use of this technique at bedtime can also help with insomnia.
Mindfulness, prayer, and meditation can also be helpful for some patients. Physicians can guide patients through a simple mindfulness exercise, such as the following: “Close your eyes. Take four deep breaths. Focus on the sound of your breath. Imagine that you are in a place where you feel calm and safe. Connect to the emotions that you are experiencing.”
Breathing and mindfulness exercises are easy to learn and can be very effective, but be sure to check in with the patient at each clinic visit to reinforce their use.
5. Prescribe physical exercise. The physical and mental benefits of regular physical exercise are well documented, and physicians can play a pivotal role in helping patients select and engage in appropriate physical activity. Some patients burdened by illness, chronic pain, and hopelessness experience a multitude of barriers to regular physical exercise. Physicians can openly talk with patients about these concerns and work with them to set realistic, appropriate, and attainable physical activity goals. It is important to suggest activities that the patient could pursue easily; for example, a gym membership can be expensive, so explore options such as walking, biking, stationary exercises at home, or exercise and yoga DVDs (many of which are free online or at the library). Writing out an actual prescription for this mutually agreed upon plan can be useful and highlight its importance. Encourage patients to keep a physical activity diary to be reviewed at each visit. At follow-up visits, you can also celebrate successes, re-address barriers, and help the patient overcome any obstacles that may have arisen.
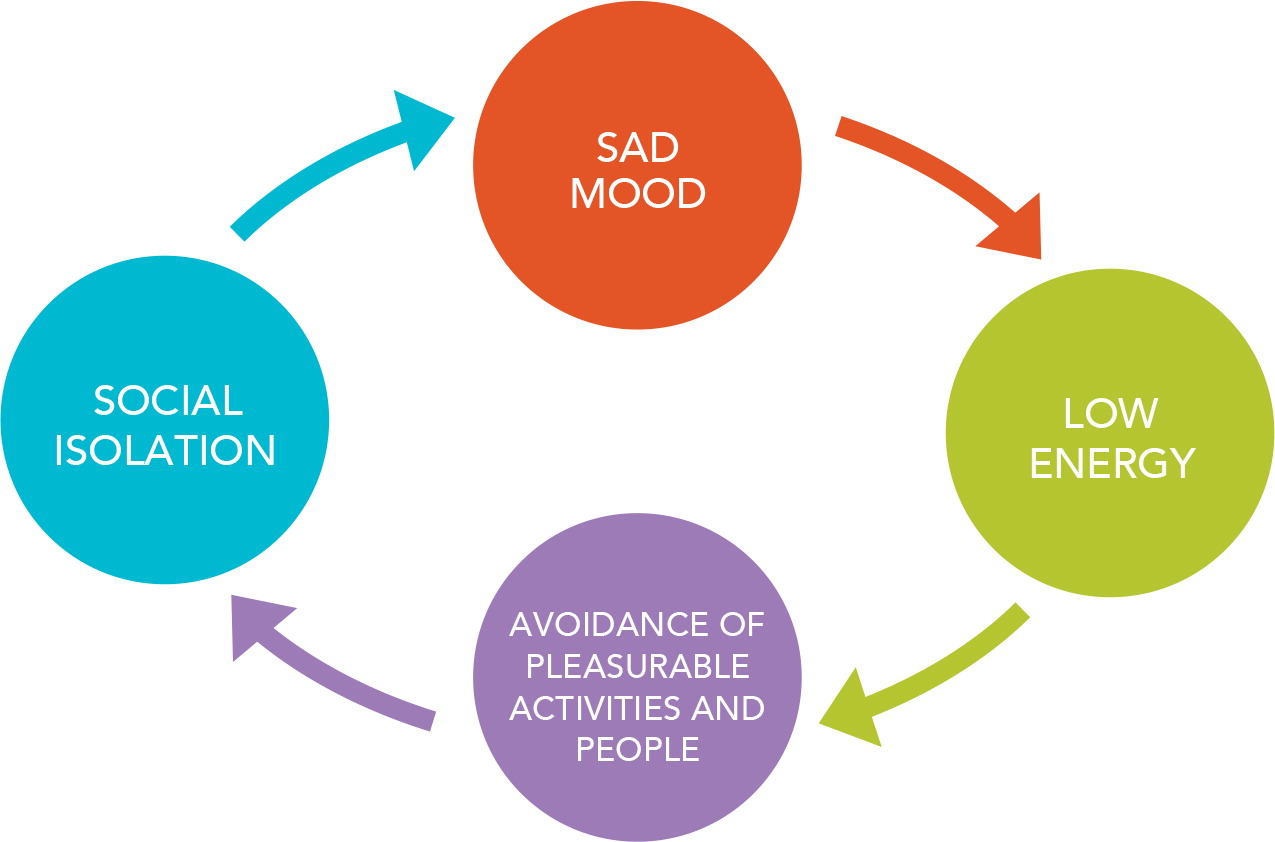
6. Encourage behavioral activation by helping the patient create a routine or schedule. Depression often involves a vicious cycle of sad mood, low energy, avoidance of pleasurable activities and people, and social isolation – all of which then exacerbate the depression. Behavioral activation is an approach to addressing depression that focuses on decreasing avoidance and isolation and increasing engagement in pleasant activities. Recent research has found that behavioral activation is as effective as cognitive-behavioral therapy and can be provided by professionals without formal training in psychotherapy.5
Physicians can empower patients to break the cycle of depression by explaining this cycle, noting the consequences of continued avoidance and isolation, and urging patients to engage in some type of pleasurable behavior (even if the patient doesn't feel like doing so). Drawing a picture of the depression cycle on paper and planning the behaviors in advance can be helpful for patients. Asking patients to track their moods before and after the planned behaviors can yield persuasive data to encourage continued activity. Patients cannot wait until they “feel like” doing something; behavioral activation requires patients to engage in activity regardless of their mood or energy level.
THE DEPRESSION CYCLE
Depression often involves a vicious cycle of sad mood, low energy, avoidance of pleasurable activities and people, and social isolation – all of which then exacerbate the depression.
Making patients aware of this cycle and encouraging them to participate in pleasant activities even when they don't feel like it can help them break the cycle.
Patients struggling with depression and anxiety also benefit from creating routines or schedules. For patients with physical or psychological limitations who cannot regularly participate in school or work, creating a regular routine can provide structure, promote social connections, and highlight a reason to get out of bed in the morning. Ask the patient to commit to specific activities each day and note them on a paper or smart-phone calendar. Patients often realize that their mood improves when they are busier, thereby creating a more positive cycle of enjoyable activities, social connections, and better overall quality of life.
Anticipate and roll with resistance
Expect that many patients will be hesitant and dubious about the helpfulness of these tools, at least initially. This reaction can be part of their negative thinking, a cornerstone of depression. You might hear from patients, “Nothing is fun anymore,” “I can't exercise like I used to because of my pain,” “I can barely afford money for the bus much less a gym membership,” “No one wants to spend time with me anymore,” or “It's hopeless. My life will never get better.” For the majority of physicians (and people in general), the automatic reaction is to try to convince patients that things will get better and to try to fix the situation. However, it is important to anticipate, honor, and explore ambivalence and barriers, especially in the early stages of behavior change. Motivational interviewing offers several ways to gauge patients' readiness for change and to address ambivalence. Asking open-ended questions, uncovering the patient's motivations for change, highlighting discrepancies between the patient's values and behaviors, and supporting self-efficacy can all strengthen the patient's ability to change.
Motivational interviewing tools can also help patients reflect on their readiness for behavior change and the progress they have already made. One such tool is the confidence ruler: “On a scale from 1 to 10, with 10 being most confident, how confident do you feel in being able to make this change?” After hearing the patient's number, the physician can ask questions such as “Why did you choose that number instead of the bottom of the scale?” and “What would it take to move one step higher on the scale?” People have a tendency to resist change when they are feeling ambivalent or pressured, so this approach reduces potential resistance by increasing patients' sense of control and confidence. The focus in behavior change is taking small steps and recognizing change is a long-term process – a marathon, not a sprint.
(For more information on motivational interviewing, see “Encouraging Patients to Change Unhealthy Behaviors With Motivational Interviewing,” FPM, May/June 2011.)
Preparing the way for more intensive treatment
Many patients benefit enough from these six skills that they do not need specialized behavioral health care. However, patients with severe psychological distress, an extensive trauma history, comorbid substance abuse problems, personality disorders, and serious family challenges (e.g., family violence) usually need more intensive, specialized behavioral health services. As noted earlier, some patients have considerable reservations about seeing a behavioral health care provider. It can be helpful for physicians to think broadly about treatment and referral options for a particular patient, considering not only individual therapy models but also peer support, 12-step programs, couples/family therapy, online classes, mental health apps, etc.
How physicians talk about behavioral health issues can shape the patient's decisions and feelings about seeking more intensive treatment. The following five tips (and sample scripts) can be useful.
Focus on the specific issue you're observing, but avoid labels and psychiatric diagnoses. “I know you've lost your appetite and have not been sleeping well since you lost your job” (noting two specific symptoms of depression rather than focusing on the label of depression).
Normalize the emotional response and express empathy/concern. “It's common to feel a lot of strong feelings after a parent dies – being angry at the world, confused, sad, and lost. I know how close you were to your mom, and I can tell you're really sad and hurting. I feel sad seeing you in such pain today.”
Note how mental health is related to physical health concerns. “I wonder if your stress [or sadness, anxiety, etc.] is making your headaches [or nausea, back pain, etc.] worse. I'm curious what connection you see between the two.”
Emphasize the power of your relationship and the team approach. “You don't have to go through this alone. I'm here, and I want to support you in this difficult time” or “We believe so strongly in addressing emotional issues as part of your overall wellness that we have behavioral health care providers here in the clinic. Dr. X has helped a lot of my patients, and I think she could help you too. Would you have a few minutes to meet Dr. X now?”
Instill hope by noting that additional treatment can help. “I have observed that others in your situation have found that talking to a counselor can be really helpful. How would you feel about that?”
The case for brief behavioral interventions in primary care
The majority of patients seen in primary care will experience one or more psychological or behavioral health problems during their lifetime. Although some patients need specialized care, primary care physicians should not discount the potential impact of taking time during clinic visits to employ brief behavioral interventions with patients who struggle emotionally or face life crises. Simple actions such as demonstrating emotional openness, instilling hope, and using active listening can be powerful. With practice, physicians will feel more confident and effective using the six tools described in this article. When referrals are necessary, physicians can greatly influence patients' willingness to follow through by highlighting the potential benefits of behavioral health services and explicitly addressing patients' ambivalence and concerns.
