
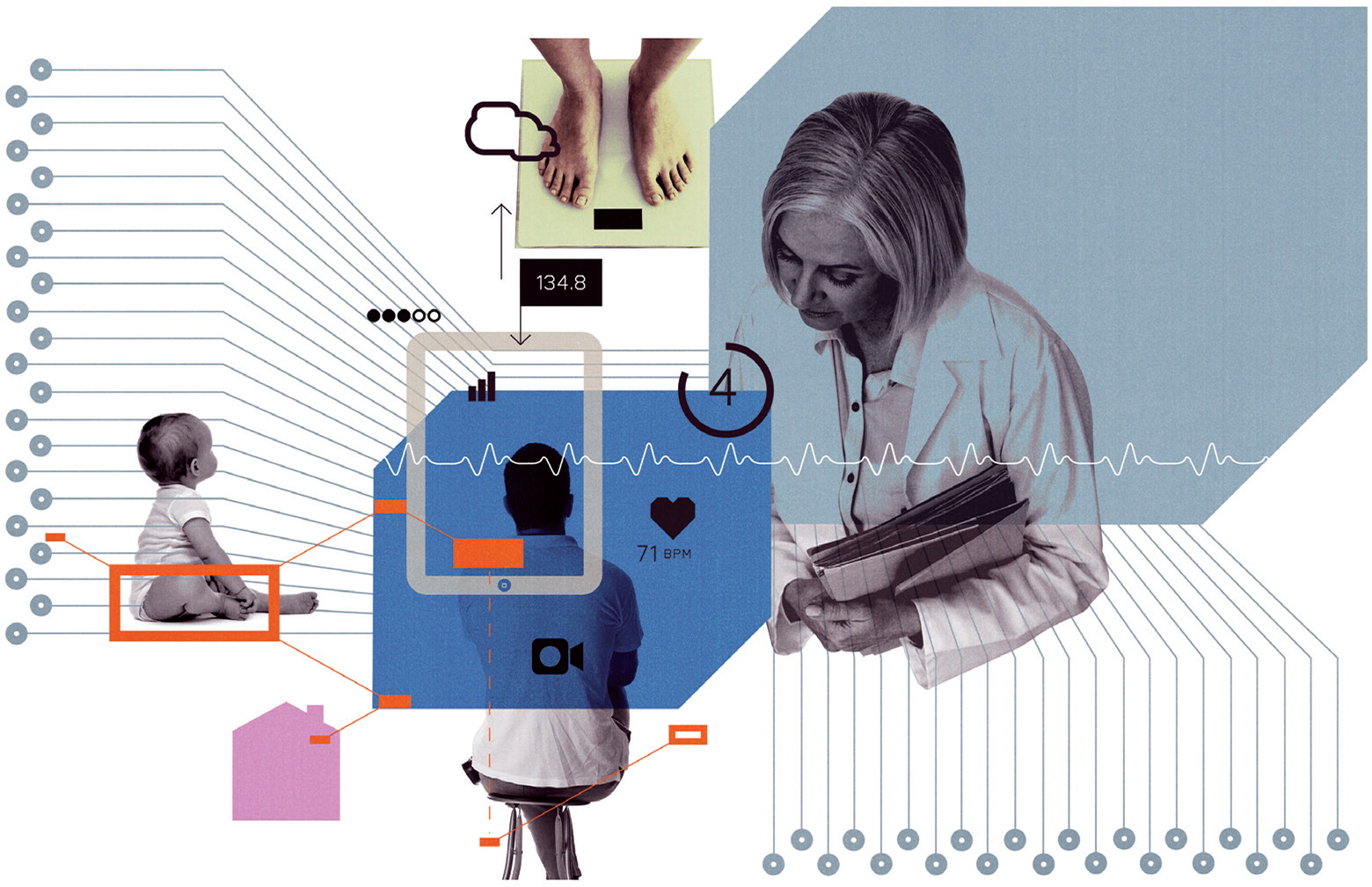
From remote monitoring of chronic diseases to virtual assistants in the exam room, technology will improve practice.
Fam Pract Manag. 2017;24(5):28-32
Author disclosures: no relevant financial affiliations disclosed.
For many physicians, health information technology (IT) begins and ends with their electronic health record (EHR) system, a product that may not generate much satisfaction for them. The rocky road to EHR implementation may have colored some physicians' perceptions of health IT, but electronic tools are getting more intuitive and useful by the day. Encouraging developments in many sectors of health IT have the potential to expand the reach and capabilities of family physicians immediately and in the near future. This article highlights some health IT trends that promise to improve patient care now and in the near future.
Patient portals and patient-generated health data
Medicare's meaningful use program and the new Quality Payment Program have helped drive the adoption of patient portals, but most practices are still learning how to optimize them. When fully implemented as part of everyday workflows, patient portals can help practices serve and communicate with patients at any time, even outside regular office hours. Making information readily available through a portal or secure messaging for patients and their families can promote adherence to treatment regimens and care planning.1 These capabilities can also help you keep revenue within your practice by avoiding penalties and earning incentives under Medicare and other value-based or direct primary care payment models. Portals also help motivated patients be more engaged in their care, which can give them more control over their medical conditions and reduce their long-term out-of-pocket costs.2,3 Most data currently flows from the practice to the patient portal, but as patients generate more of their own health data through such things as wearable devices or remote patient monitoring (more on these trends later), we expect to see them submitting that data to portals more often.
Telemedicine and telehealth
Although telemedicine in its traditional form still exists, the acceptance and prevalence of virtual visits and e-consults are redefining the term and changing the face of the technology, which typically includes webcams (for synchronous visits), telehealth software, and sufficient Internet speeds. Outside of rural and undeveloped areas, virtual visits once were conducted solely between direct-to-consumer national telehealth service organizations dealing with conditions typically seen in an urgent care setting. That phase could be labeled “telehealth 1.0.”4 Today, “telehealth 2.0” is well underway, with the volume of reported virtual visits increasing exponentially as greater numbers of payers and employers agree to cover telehealth services, diagnostic peripheral devices allow virtual physical exams for a wider number of presenting conditions, and more medical practices adopt telemedicine.5,6,7
Traditional practices are embracing telemedicine for a number of reasons, including the growth of value-based payment models that incentivize physicians to provide greater access to care and increasingly hold them accountable for cost and resource use. Practices that use the direct primary care model also see telemedicine as a way to improve patient outcomes while containing costs for both patients and themselves. Plus, giving patients the option of a virtual visit with their trusted family physician helps prevent them from turning to direct-to-consumer telehealth services, which can result in fractured care and lost revenue. Finally, telemedicine lets physicians make care more convenient for themselves and their patients.
Remote monitoring and patient-contributed data
Technology is making it easier for physicians and other clinicians to monitor patients in their homes for a number of chronic diseases in a more routine and automated way. For example, practices can use remote monitoring to track patient weight for congestive heart failure, fasting glucose for diabetes, blood pressure for hypertension, and oxygen saturation for chronic obstructive pulmonary disease (COPD). Data can be incorporated directly into the patient portal and EHR so that it is available for use during patient self-management, care management planning, or at the point of care. Converging and overlapping technologies are assisting this automation, such as the increased use of smartphones by patients. A recent Pew Research Center report indicated that nearly 75 percent of Americans own a smartphone, including more than 40 percent of those over the age of 64.8
Many smartphones can use software applications and Bluetooth or other wireless connections to automatically upload and securely store data from commercial grade medical devices including scales, glucometers, blood pressure cuffs, heart rate monitors, pulse oximeters, and others. For example, the Propeller is a sensor that attaches to an inhaler to electronically record and, through a mobile app, send the physician data that can help treatment for asthma and COPD. AliveCor makes a fingertip sensor strip that patients can use to record an EKG and deliver results to their smartphone and their physician via a mobile app.
In the clinical setting, many commonly used EHRs and their connected patient portals can securely import these data from a smartphone or tablet, making them available to clinicians at any point in the process of care, such as for tracking the weights of a recently discharged patient with congestive heart failure or the fasting glucose levels of a patient with diabetes who is taking a new medication.9
Long an obstacle for this type of technology, the user interfaces for these devices are getting better and more patient-friendly. Some commercial products can now display normal, abnormal, and critical results along with recommended actions, such as glucometers that advise patients when to contact a physician in response to consistently low glucose readings. EHR vendors continue to upgrade their products to facilitate better data integration and display for physicians. EHRs are increasingly able to display large quantities of patient-generated data as graphics that highlight trends and out-of-range data in ways that are easy to understand and interpret. These systems also enable clinical decision support by filtering these data and alerting clinicians only when there are worrisome abnormal variations, which can reduce the clinical workload and let providers focus on the most important issues.
Secure messaging
Direct exchange is a way of sending secure email using HIPAA-compliant standards that are now part of certified EHR technology (CEHRT). In fact, you likely already have this capability in your EHR. It functions like regular email but is more secure and is recognizable by “@Direct” in the email address. It has become very popular in recent years with more than 1.4 million Direct exchange email addresses and users sending millions of messages each month.10 Direct exchange makes it easy for physicians to send messages securely to colleagues, health care organizations, and to patients. It also supports the sharing of patient data between EHR systems as well as health information exchanges, which ultimately improves the delivery of coordinated, collaborative care.
Opening up the EHR
A key weakness of EHRs is that most are closed systems without the ability to readily exchange data or integrate with other external software. But this is changing. Pressured by requirements of the Centers for Medicare & Medicaid Services' CEHRT program and newly authorized financial penalties against information blocking under the 21st Century Cures Act, vendors are being forced to make their products more open. Additionally, market forces are pushing vendors toward interoperability to compete against larger EHR competitors. As a result, physicians will no longer be completely dependent on their EHR vendors to provide them with the functionality they want. One CEHRT requirement is that vendors must provide within the EHR an open application-programming interface (API), a piece of technology that is a cornerstone of the modern Internet. An API enables authorized third-party vendors to securely access the data within an EHR, which gives physicians the ability to connect external devices to their EHR, send data to applications that can apply evidence-based medicine, integrate population management software, and export data to another EHR. APIs also make it easier for physicians to receive patient-generated health data through apps like those discussed previously.
Machine learning
The health care industry has not kept up with the cutting edge of information technology, but exploring advancements outside our industry does allow us to see the potential of these innovations for family medicine and primary care. If you have ever used Google or Facebook, then you have taken advantage of machine learning. In essence, machine learning is programming that lets the computer learn how to do something rather than simply follow a series of programmed commands to do something. This innovation has profound promise for health care given its complexity and scale. It is not feasible for programmers to code all of the requisite complexity of health care into the computer. Even if it were, they would have to revise the code every time we learned something new. With machine learning, a single computer, working with thousands of other computers in the online “cloud,” can continually review new data and adjust its understanding. We are seeing machine learning provide significant advancements in how computers recognize and understand human speech. This could potentially reduce the amount of data entry physicians must perform and help sift through voluminous amounts of patient data and evidence to quickly find information. There are some specific subdomains of machine learning:
Computer vision. Scientists and software engineers are working to train computers how to “see.”11,12 For example, they have created machine learning models that can “look” at a picture of a skin lesion and with a high degree of accuracy determine if the lesion is potentially malignant. There are also models that can interpret a retinal scan and identify diabetic retinopathy changes as accurately as an average ophthalmologist. The goal is for computers to be able to distinguish between normal and abnormal results in many arenas, which could potentially allow primary care physicians to perform a wider array of screening tests and do so at a lower cost.
Affective computing. One of the newest areas of machine learning, this involves developing models that allow a computer to recognize, interpret, and mimic human affect. The potential of affective computing for medicine is fascinating. Imagine if a computer playing an educational video to a patient could recognize when the patient became confused. It could then notify practice staff that the patient needed additional information around a specific topic or even offer its own alternative or additional education around that topic.
Virtual assistant. Technically this is not a subdomain of machine learning but rather an application of a number of machine learning models. You may have already interacted with a virtual assistant, such as Amazon's Alexa and Echo devices or the Google Assistant feature of Google Home. Imagine if you had such a device in the exam room linked to the EHR and a display screen on the wall. As you were conducting your office visit, you could ask the virtual assistant to display and trend the patient's latest hemoglobin A1C values. You would not have to redirect your attention from the patient to search for data in the chart. Just as Amazon's Alexa can order dog food from the grocery store, you could direct the virtual assistant to order a lab test or prescribe a new medication. The artificially intelligent virtual assistant could ease many administrative burdens faced today by physicians.
The “Internet of Things”
Computers are becoming ubiquitous. Even refrigerators have computers that can connect to the Internet. You can look into the refrigerator from your smartphone while at the grocery store to see if you need to buy milk. In health care, wearable devices like activity trackers have become mainstream. There are also instances of pill bottles that can track and report when the bottle was opened. All of these things are connected and communicating enormous amounts of data from their sensors. Computer applications can aggregate these data streams to extend the physician's reach beyond the walls of the clinic and provide a new set of capabilities to health IT. For example, physicians and nursing staff could use wearable devices that let the EHR know exactly where they are located. The EHR can then recognize when the nurse or physician enters an exam room and log them in. If the patient's smartphone is linked to the EHR, it could also know when the patient is in the room and open the chart. The EHR would also know how much time the physician or nurse spends with specific patients. These data can be used to personalize appointment lengths or support time-based billing.
The next big thing
This article only begins to consider the innovations in health IT, and the rate of innovation is continuing to accelerate. Although it is easy to see how current technologies can improve the lives of patients, physicians, and staff, the most exciting innovations have yet to see the light of day.
