
Want to see change in your team, your organization, or beyond? Start by filling your own tank.
Fam Pract Manag. 2020;27(2):17-22
Author disclosure: no relevant financial affiliations disclosed.
“One A Day” is a multivitamin designed to promote good health. It also represents the approximate number of physicians who die by suicide daily in the United States.1 Even one preventable death is too many, and it is a tragedy that as health professionals we are often not able to care for ourselves as well as we care for our patients.
Many stressors contribute to the rising cycle of burnout, depression, and suicide among health professionals.1 Chronic stress that results from workload exceeding workforce, lack of time and control, and feelings of inadequacy and hopelessness are just a few of the causes. The stigma around mental health and self-care often limits professionals from seeking help or even acknowledging they need a break. Additionally, despite having the knowledge and skills to diagnose and treat others, physicians do not effectively recognize burnout in themselves.2
After delivering a workshop on physician wellness recently, I met a participant named Marta who slipped me her personal business card with a note scribbled on the back. It read, “I need help.” The conversation we had that afternoon echoed words I've heard in my own head and from colleagues across all fields and all types of medical practices: “I can't relax because there is so much to do, and it will never be done,” “I've slipped so far from what I envisioned myself doing as a doctor that I have lost my sense of purpose and belonging,” “I feel so isolated,” “I have no control,” “I'm too busy to even know what to change or do about it,” and “I feel guilty that I just don't care anymore.”
These words paint a vivid and distressing picture of burnout. Marta compared her work to the definition of insanity attributed to Albert Einstein — “doing the same thing over and over again and expecting different results.”
How can physicians break out of this cycle and achieve a state of peacefulness, integrity, belonging, accomplishment, autonomy, agency, and compassion?
For doctors in crisis, the National Suicide Prevention Lifeline (1-800-273-TALK) is critical, but for other physicians, self-care is a viable solution. This article will highlight a critical shift in thinking — one that prioritizes caring for oneself as an effective means of caring for others. The emphasis will be on role modeling self-care, including practicing mindfulness and improving physical health, because personal transformation is the cornerstone for leading change broadly.
KEY POINTS
A broken system is not an excuse to not care for ourselves. It is a call to action.
Physicians should consider a critical shift in thinking — one that prioritizes caring for oneself as an effective means of caring for others.
Two strategies for self-care include practicing mindfulness and improving physical health.
PERSONAL TRANSFORMATION OR SYSTEM CHANGE?
When I coach physicians about burnout and well-being, they often make the point that the system is the problem, not them, and they sometimes express anger and resentment when challenged to practice self-care.
It's true that our health care system is broken and not supportive of physicians, and our learning and practice environments are often toxic. We should assign blame where it is due — to the system rather than the individual. But who is the system, and can it fix itself?
The 2019 National Academy of Medicine 333-page consensus report, Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being, highlights the importance of system change, but it also calls on individuals who make up the system to lead the change.3 The alternative to leading the change ourselves is that nothing will change, or nonphysician administrators will change the system in ways we may not like.
A broken system is not an excuse to not care for ourselves. It is a call to action. We must rise above our toxic environments and find successful well-being strategies for personal transformation. The power to change the system comes from filling the tanks of all physicians — including those in training. We change our culture by caring for and changing ourselves. We are the system. We are the culture. We must save lives, including our own. We must lead the change.
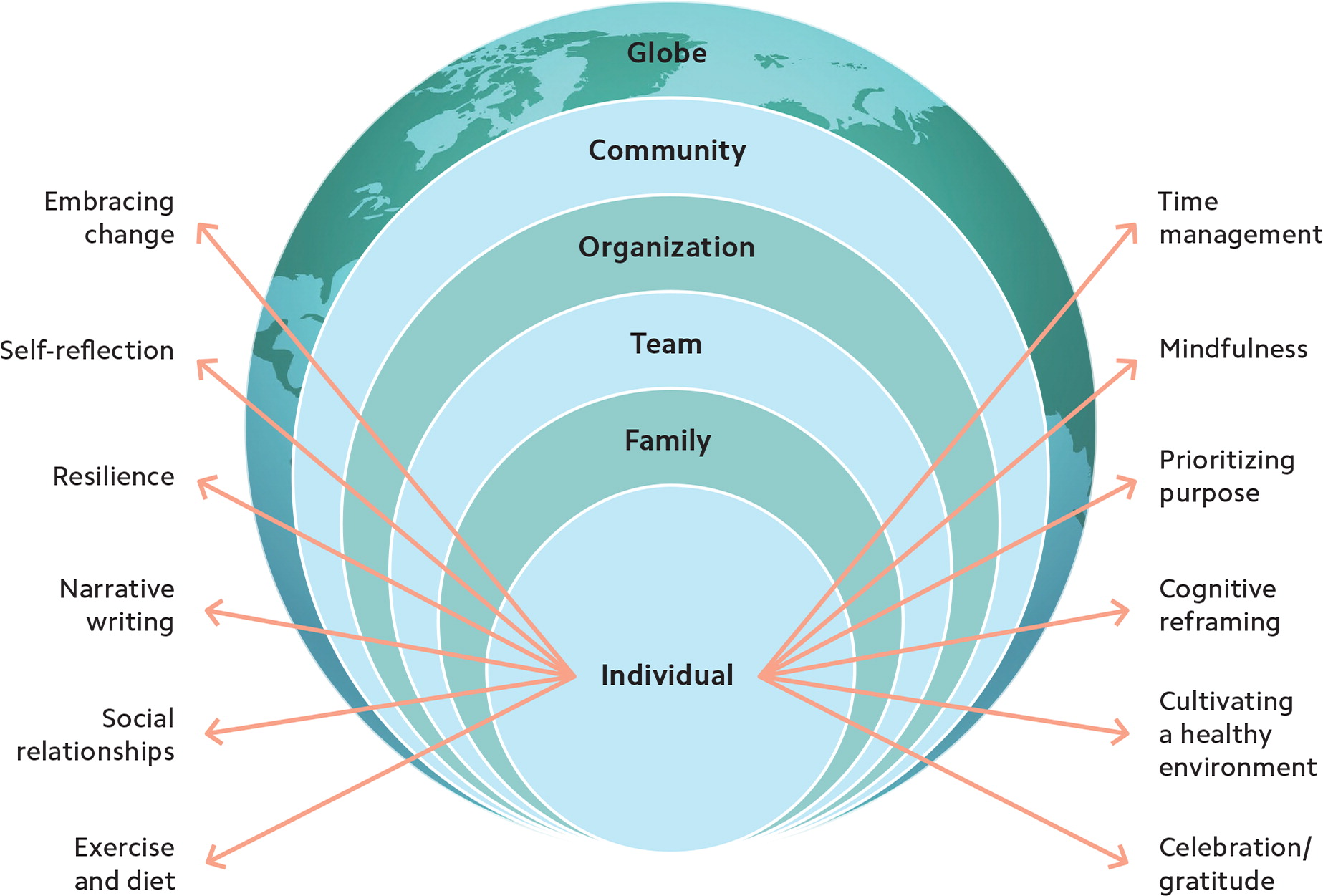
The social ecological model illustrates how change begins with each of us as individuals applying a variety of wellness strategies, and then it spreads outward to our families, teams, organizations, communities, and beyond.
All of us in family medicine will be needed to change our system. Empowered with the tools, strategies, and permission to care for ourselves, we can serve as crucial role models, even in difficult systems. We can give our colleagues permission to follow suit, stop the shaming around self-care, design healthy policies in our organizations, implement effective curriculum in our training institutions, construct healthier physical environments, hold our leadership accountable to meet authentic well-being metrics, and ultimately design supportive systems.
MINDFULNESS: A TOOL TO REDUCE STRESS AND REPLENISH ENERGY
Mindfulness, in its most basic form, is self-awareness. It is the practice of watching, observing, reflecting, and listening so that you see the present — yourself and the world around you — more clearly and without judgment. For physicians, the benefits of mindfulness extend beyond personal stress reduction, improved health conditions, and increased job satisfaction; mindfulness can also improve the patient experience.4,5
Mindfulness can be difficult for those of us who are master multitaskers, lack the word “no” in our vocabularies, have FOMO (fear of missing out), or would rather do just about anything than do “nothing.” It takes practice to appreciate the calmness, creativity, and peace that come in moments of mindfulness.
If you're new to mindfulness, you might start with a simple self-assessment. The Mindful Attention Awareness Scale (MAAS) is a validated tool that measures our ability to focus attention and awareness in daily life.6 It assigns individuals a mindfulness score based on how frequently they experience 15 scenarios, such as “I find myself doing things without paying attention,” “I forget a person's name almost as soon as I've been told it for the first time,” and “I find myself preoccupied with the future or the past.” (You can find the MAAS tool through various sources online, such as http://www.mindfulness-extended.nl/content3/wp-content/uploads/2013/07/MAAS-EN.pdf.) Consider taking the MAAS or at least observing your mental habits for a day. Pay attention to the conversations you're having in your mind, reflect on your reactions and your day-to-day activities, and consider how they interrelate. For example, if you've been responding tersely to your staff all day, take a moment to think about why and what activity might be triggering that response. Don't judge yourself. Just pay attention to what's going on and be honest about how you feel.
There are many ways to begin a mindfulness practice. I recommend starting with as little as 10 minutes a day of mindful meditation, mindful walking, or focused breathing. (For guidance on these activities, see “Resources.” For a sample mindfulness goal, see “Sample goals to help you get started.”)
Saying “no” to others' requests on our time and energy can also be an act of mindfulness. Instead of mindlessly saying “yes” to every request, try saying “no” at least once each day — “no” to another committee, another title, more meetings, or more stuff. This can lead to JOMO (joy of missing out), the alternative of FOMO. Your colleagues, friends, and family might even respect and appreciate you for setting limits, as opposed to saying “sure” but being stressed or not delivering.
SAMPLE GOALS TO HELP YOU GET STARTED
| To increase your likelihood of success in the area of personal transformation, focus on just one change at a time. For a tem- plate that walks you through the process of setting “SMART” goals, which includes addressing barriers and setting measures for success, download the Personal Health Improvement Plan or use the online version (www.MyPHIT.org) to get daily reminders. | |
| Mindfulness goal | Sleep goal |
| Specific – Practice mindful meditation for 10 minutes every morning. | Specific – Get at least seven hours of sleep every night. |
| Measurable – Process: Did I meditate today (yes or no)? Outcome: On a scale of 1 to 5, how stressed did I feel today? | Measurable – Process: Did I complete the goal today (yes or no)? Outcome: On a scale of 1 to 5, how rested did I feel today? |
| Achievable – How confident am I that I can achieve this goal (scale of 1 to 10, with 6 or greater required)? | Achievable – How confident am I that I can achieve this goal (scale of 1 to 10, with 6 or greater required)? |
| Relevant – How important is it for me to achieve this goal (scale of 1 to 10, with 6 or greater required)? | Relevant – How important is it for me to achieve this goal (scale of 1 to 10, with 6 or greater required)? |
| Timely – Begin today, and continue for 21 days. | Timely – Begin today, and continue 30 days. |
| Healthy eating goal | Exercise goal |
| Specific – Consume at least seven fruits or vegetables daily. | Specific – Run five times per week for 30 minutes. |
| Measurable – Process: Did I complete the goal today (yes or no)? Outcome: On a scale of 1 to 5, how energized did I feel today? | Measurable – Process: Did I complete the goal today (yes or no)? Outcome: On a scale of 1 to 5, how energized did I feel today? |
| Achievable – How confident am I that I can achieve this goal (scale of 1 to 10, with 6 or greater required)? | Achievable – How confident am I that I can achieve this goal (scale of 1 to 10, with 6 or greater required)? |
| Relevant – How important is it for me to achieve this goal (scale of 1 to 10, with 6 or greater required)? | Relevant – How important is it for me to achieve this goal (scale of 1 to 10, with 6 or greater required)? |
| Timely – Begin today, and continue for 30 days. | Timely – Begin today, and continue for one month. |
BACK TO THE BASICS: HEALTHY EATING, SLEEP, AND EXERCISE
As I've coached physicians over the years, I have noticed that they often pride themselves on their “superhuman” status — able to work all day without the need to eat, sleep, or exercise. Denying physical needs is like a badge of honor in medicine, but it also contributes to an empty tank and negatively affects our ability to care for others. Evidence-based strategies that promote our physical health include healthy eating, sleeping, and exercise habits, yet we often neglect these basic means of replenishing ourselves. Perhaps we should consider the same advice we give our patients and ask ourselves the following:
Do I eat five or more fruits or vegetables daily?
Do I limit saturated fats and foods and beverages with added sugar?
Do I drink alcohol in moderation?
Do I get 30 minutes of cardiovascular exercise most days and muscle-strengthening at least twice a week?
Do I get the recommended seven or more hours of sleep each night?
If your answer to all the above is “yes,” congratulations! You are in the minority. Reflect on how you manage these habits so well. Journal your routines so that if in the future anything changes, you can return to your healthy habits.
If your answer to any of the above is “no,” consider why you do not practice healthy habits. Is it because you feel you have no time, no energy (you're too tired), it's not your priority right now, you've failed too many times so it's not worth trying again, or another reason? Explore your barriers and brainstorm solutions using the Personal Health Improvement Plan template.
Often the problem is that as physicians we feel that we have to do everything, do it all perfectly, and do it all now. We deny ourselves permission to ever be “done” (with email, charting, projects, etc.), to replenish, or to enjoy anything. But to be most effective in our work life or personal life, we have to take care of ourselves. Give yourself permission to stop trying to do it all and start focusing on your own well-ness. Pick just one goal that you will focus on for the next 30 days to improve your physical health. (See “Sample goals to help you get started.”)
RESOURCES
Mindfulness
Mindfulness video by Jon Kabat-Zinn
Headspace, a guided meditation and mindfulness app (free limited session options)
InsightTimer, a free app for guided meditations, music tracks, talks, and courses
AllTrails, an app to find a hike wherever you are to practice walking meditation
Healthy eating and exercise
MyFitnessPal, an app for tracking calories, macronutrients, exercise, goals, etc.
Cronometer, an app for logging your diet, exercise, biometrics, and notes
BodySpace, an app that offers free weight training workouts and programs designed by elite trainers and fitness pros as well as tips, visual guidance, and access to a supportive online fitness community
Seconds Pro, an app that offers a free interval timer for high-intensity interval training (HIIT), Tabata, and circuit training workouts and allows you to build custom workouts
Yummly, a recipe resource that allows you to filter for specific dietary needs (gluten-free, dairy-free, vegan, paleo, etc.)
IT STARTS WITH US
Changing ourselves can be the most challenging yet most rewarding work we will ever do. We will need to walk the walk every day, learn from those around us, and learn from our own successes and struggles. Prioritizing our own well-being has the power to change not only us but also the culture of medicine.
SERIES OVERVIEW

In this or previous issues:
Creating your personal wellness plan (January/February 2020).
Self-care through mindfulness and strategies for promoting physical health (March/April 2020).
In upcoming issues:
Family well-being through social connectivity and time management.
Team well-being through conflict resolution and promotion of gratitude in the workplace.
Organizational well-being through prioritizing purpose and creating resilient leaders.
Community well-being through cognitive reframing and building emotional intelligence.
