
When an infectious disease outbreak strikes, an outdoor clinic can reduce the risk of transmission and conserve personal protective equipment.
Fam Pract Manag. 2020;27(5):14-19
Author disclosures: no relevant financial affiliations disclosed.

When the COVID-19 outbreak in the United States was declared a national emergency on March 1, family medicine practices had to quickly adapt their workflows to continue providing essential care while limiting the spread of infection. Our clinic, Eglin Family Medicine Residency Clinic (FMRC), responded to the pandemic's challenges in a way that is instructive for the current crisis and future infectious disease outbreaks: by establishing a drive-in outdoor clinic for testing and treating suspected infections.
Eglin FMRC is a 36-resident program with 12 core faculty members, nestled in a small military community hospital in northwest Florida. Our primary goal as a health system during the pandemic was to decrease patient flow through our main building, while preparing for an expected inpatient surge and continuing to meet outpatient needs. We decided early on to create an outdoor urgent care unit to evaluate potentially infectious patients.
Other clinics have published information about performing outdoor care pre-COVID-19, but few have published detailed instructions on how to set up an outdoor clinic.1 A systematic review of 13 articles identified effective practices and recommendations for drive-through clinics to dispense mass prophylaxis during public health emergencies, but these articles were mainly based on simulations.2 This article documents some practical processes, policies, and workflows implemented during a real-life emergency, which other institutions may find useful when the next infectious outbreak occurs.
KEY POINTS
A drive-in clinic allows physicians to evaluate patients with symptoms of an infectious disease without exposing other patients or staff. It also reduces the need for surface cleaning between visits.
Separating the outdoor clinic into “cold,” “warm,” and “hot” zones using hazardous materials protocols helps preserve personal protective equipment while reducing transmission risk.
Climate and staffing are factors that could limit the ability to establish a full outdoor clinic, but even small practices may be able to adapt some of the principles for occasional outdoor patient visits.
SETTING UP THE CLINIC
Our hospital leadership designated some parts of the hospital “noninfectious” and others “infectious.” Patients who screened positive for any COVID-19 symptoms would be seen in the infectious areas, which included the FMRC, emergency department (ED), and inpatient wards. Personnel in these areas needed to prepare to maintain a high degree of capability despite expected staff absences. To that end, FMRC devised a drive-in clinic to efficiently utilize limited staff, personal protective equipment (PPE), and facilities while delivering face-to-face care to patients suspected of being infectious. This drive-in, appointment-based, urgent care clinic relieved significant stress on the ED, permitting ED staff to focus on higher-acuity patients.
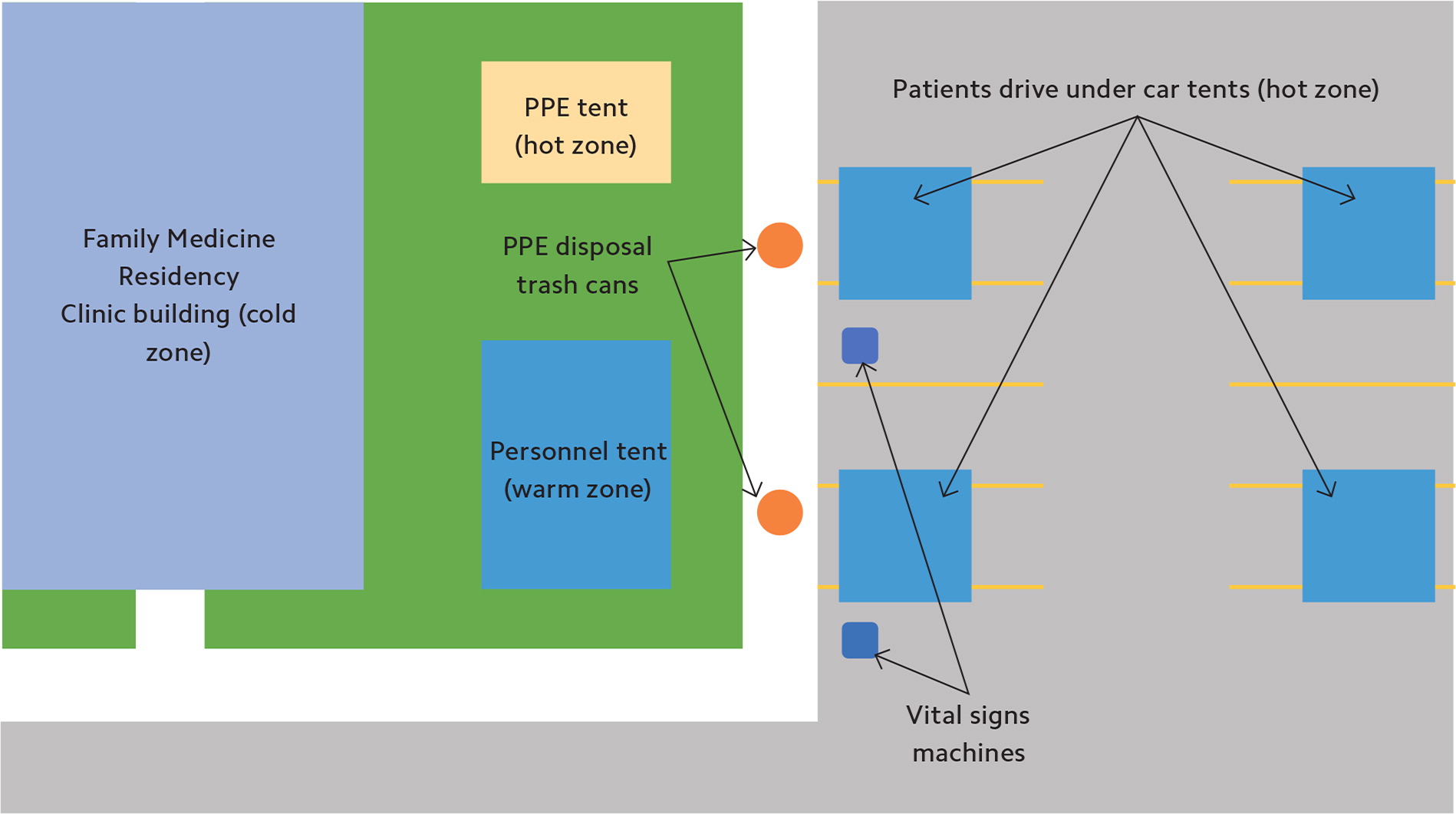
The drive-in clinic was constructed adjacent to the FMRC building in an L-shaped parking lot with easy access to main roads. Cones were set up to identify four patient parking spots, which were strategically distanced to reduce infection risk and maximize patient privacy. Staff used two battery-powered vitals machines to record temperature, blood pressure, heart rate, and critical pulse oximetry data. The clinic sheltered the patient parking spots from the weather with outdoor canopy tents that had no sidewalls (see Photo 1).

We designed the physical layout of the outdoor clinic to avoid mixing potentially infectious equipment and PPE with unused equipment. Using hazardous materials protocols, FMRC staff designated several different zones to mitigate the risk of contamination outside the patients' cars.3 We established a “hot,” or contaminated, zone in the tent where PPE was stored, donned, and discarded. New PPE was kept in original containers, while used PPE was labeled with the name of the user and hung on the edges of the tent during breaks in shifts so it was available for reuse. Staff used trash cans nearby for PPE disposal at the end of their shifts. In the “warm” or support zone, the clinic placed a tent where staff members who weren't working directly with patients cleaned and disinfected equipment. Staff in this zone wore surgical masks and scrubs, and donned disposable gloves to wash equipment. They then left the equipment close to the patient parking spots — also designated hot zones — where it could be accessed for patient care by staff in full PPE, which included N95 masks and surgical gowns. Indoor residents and staff worked in the “cold” zone providing virtual support, without a need for PPE. Our staging scheme was a modified version of hot, warm, and cold staging areas often used for nuclear, chemical, or biological agent decontamination processes in which staff transition from different areas that each have their own PPE requirements. (See “Overhead view schematic.”)
Staff members were each issued one N95 and/or surgical mask and one PPE gown for use during each clinic day. PPE was tracked closely and labeled. Staff changed gloves between patient encounters. When staff members performed a COVID-19 nasal wash, they discarded PPE and put on new gear, as this was considered a high-risk aerosolization procedure. But the use of each mask and gown was otherwise extended. Outdoor clinic staff remained in their PPE until their shift concluded.
PATIENT CARE
To streamline care, when a patient called the clinic with a concern, a nurse first spoke with the patient using institution-approved triage protocols. If the patient had a clearly noninfectious concern, such as a sprained ankle or a medication refill, the nurse performed a COVID-19 symptom screening and if the screening was negative, triaged the patient into a virtual appointment or, if necessary, a face-to-face appointment in a clinic designated noninfectious (see “Patient triage flow”).
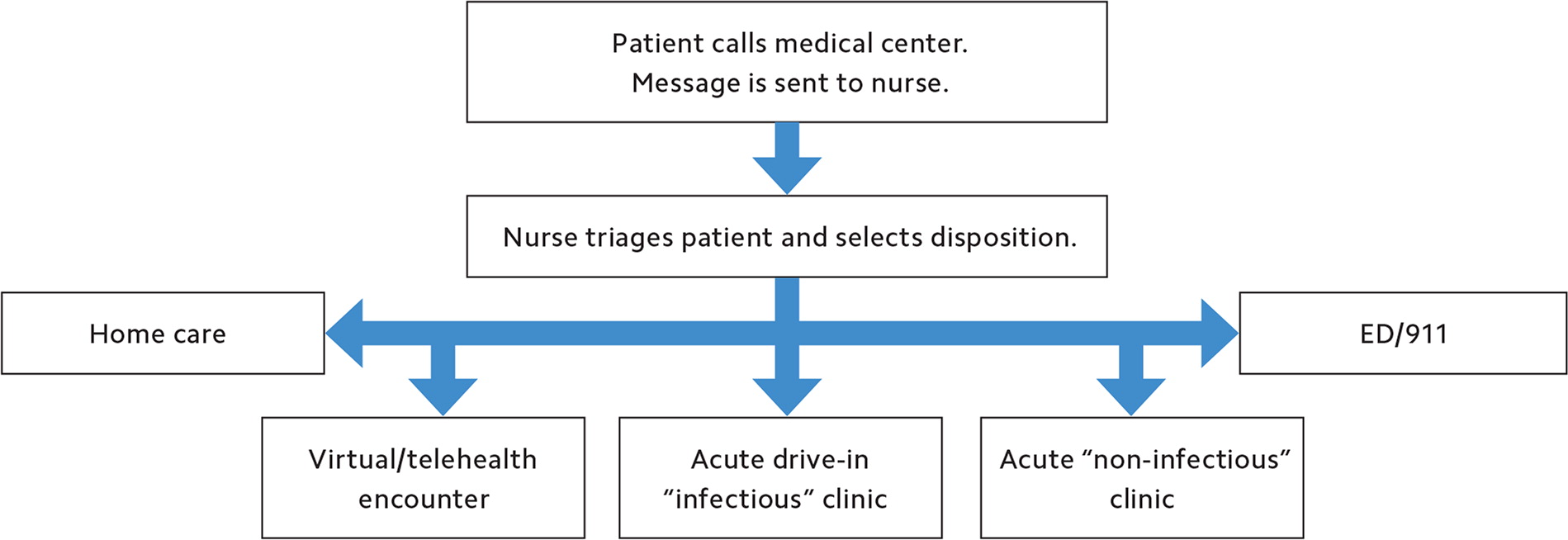
Using this method, most visits were conducted virtually, including chronic disease management. Only patients who required a physical exam for appropriate medical care were sent to face-to-face visits. If the patient was deemed an infection risk, either because of a positive COVID-19 risk factor screen or other infectious disease symptoms, the patient was booked into a face-to-face appointment at the outdoor FMRC drive-in clinic. Next, a resident physician took the patient's history over the phone to limit face-to-face interaction at the drive-in clinic and directed the patient to the outdoor clinic for physical examination and subsequent care.
After discussion with the indoor resident physician who conducted the virtual part of the encounter, another resident physician evaluated the patient in the vehicle, or occasionally outside the vehicle (see Photo 2).

A medical assistant wearing a surgical face mask stood more than six feet away and served as a scribe. After staffing the case with the outdoor attending faculty, the resident physician ordered the appropriate testing. The clinic offered streptococcal pharyngitis (rapid strep), polymerase chain reaction (PCR) influenza, respiratory panel, and novel coronavirus (COVID-19) testing. The clinic also offered amniotic fluid index measurements and nonstress fetal testing, as well as Rho(D) immune globulin (RhoGAM) and other injectables, to patients with concurrent infectious symptoms. If a patient needed additional diagnostics such as an electrocardiogram or X-ray, staff gave the patient a mask and then escorted the patient directly into an available exam room inside the FMRC. After concluding the face-to-face evaluation, the outdoor resident relayed physical exam findings and treatment information via cellphone or two-way radio to the resident working inside the office, who completed charting and wrote any necessary orders.
Disposition of patients ranged from no testing and no required follow-up to urgently directing them to the ED for evaluation and admission. Attending-to-attending physician consult occurred when ED evaluation was recommended. Our pharmacy issued ready-made “common cold” packs stocked with symptom treatment medications. When we dispensed these to patients, clerks recorded which medications in each pack were used and then communicated that to the pharmacy. Each day, the pharmacy would then document the dispensations in the electronic health record (EHR), which reduced charting burden. If a physician prescribed a medication that was not pre-dispensed, such as amoxicillin, the outdoor team dispatched a runner from the cold zone inside the clinic to pick up the activated medication at the on-site pharmacy. The medication was then handed off to the outdoor team in the warm zone tent (see Photo 3). This task allowed prescription medications to be readily dispensed at the drive-in clinic. Thus, patients did not enter the hospital unless absolutely necessary, which reduced institutional infection risk. Staff recorded patients who were tested for COVID-19 on a roster, and then clinic clerks booked them follow-up appointments via telehealth for three days later to discuss lab results and reevaluate symptoms.

RESULTS
Our extended-PPE approach prepared us to balance staff protection with efficiency. We estimated that our staff would use a maximum of 24 gowns, six N95 masks, and 63 surgical masks per day if all 32 face-to-face appointments we offered were filled. Staff utilization numbers were driven by work-rest cycles. To staff this model, we employed eight medical assistants, one clerk, eight resident physicians, and two attending faculty each day. We had four medical assistants on for an hour and then off for an hour. This reduced fatigue in the hot Florida sun. By adding additional teams, we could sustain a surge of up to 64 appointments per day. Effectively, half of our workforce was resting while the other half was working. This limits the applicability of our approach to clinics of a certain size. However, smaller clinics could adapt the physical layout and potentially offer in-person visits for a half day and virtual visits the other half of the day to reduce staff utilization.
On average, patients utilized 16 outdoor clinic appointments per day. We had capacity for greater numbers of infectious patients, but as of June 1, we had not experienced the demand we anticipated. During the period from March 23 through May 1, our clinic conducted 212 clinically indicated COVID-19 tests and diagnosed COVID-19 in 26 patients. This has changed more recently with the surge in cases in Florida. By July 20, our suspected COVID-19 patient visits had roughly doubled, and we had to add additional appointment slots.
Prior to the pandemic, we offered 12% of our visits virtually. After our retooling, that number climbed to about 70%, including 95 virtual chronic care appointments. The virtual visits accounted for, on average, about 30 patients per day (in addition to the 16 outdoor face-to-face appointments). Simply put, we found that demand for routine primary care decreased tremendously. As expected, our billable diagnoses changed significantly over this time period. Our top four diagnoses pre-COVID were hypertension, low-back pain, annual physicals, and hyperlipidemia. During the initial six weeks of our outdoor urgent care clinic, the top four diagnoses were hypertension, acute respiratory infection, cough, and Type 2 diabetes. Our year-over-year revenues dropped 53% over this period, due largely to the reduction in annual preventive medicine visits to zero. The slippage would likely have been greater, if not for the face-to-face acute care visits the outdoor clinic allowed us to do, as well as the follow-up virtual visits three days later for all patients who had COVID-19 tests.
Other benefits of the outdoor clinic were clearer. Our approach decreased expected ED visits for non-severe infections by 50%. Our outdoor clinic also decreased the use of housekeeping, preserving those resources for the rest of the hospital, because few indoor clinic exam rooms needed to be turned over. Following our facility's COVID-19 protocols, exam rooms would be out of service for two hours after each use, meaning we likely would have run out of rooms if not for our outdoor clinic. Use of canopy tents, as opposed to more structured tents with pipe framing and thick plastic walls, also decreased the housekeeping burden and decreased carbon mon-oxide exposure, which was identified as a threat in the systematic review of drive-in clinic simulations mentioned earlier.2
LESSONS LEARNED
We learned several important lessons.
First, all staff should have a say in the workflow because no group has a monopoly on good ideas. Our group met twice a day initially, and then daily after about a week, to discuss iterative changes in the work-flow to improve efficiency and quality. Staff implemented changes the day after they were approved.
Second, by reducing strain on the ED and conserving PPE we further endeared ourselves to our colleagues in the wider Eglin health system. Protecting resources during a stressful time improved our relations with other departments, adding to institutional morale while providing a much-needed means to evaluate worried, potentially infectious patients who weren't ill enough to require emergency care.
Third, weather was a big factor in our success. Florida is known for rain, and the necessity of tents for all-weather operations cannot be overstated. Research suggests similar severe acute respiratory syndrome (SARS) coronavirus virions survive poorly at high ambient temperatures and elevated humidity.4 The logical implication is that this may decrease viable virus particles, which presumably decreases infection rates and transmissibility. The latest surge in cases across the South and Southwest casts doubt on this theory, but it's possible that moving staff outside in sunny, humid Florida reduced transmission risk, even if only slightly.
Finally, we learned that the staff enjoyed working outside tremendously. We actually had to remind our medical assistants not to congregate in the clinical area of the outdoor clinic while on breaks. This would not be the case in every climate, of course, which illustrates a key external limitation of our model.
Overall, our approach preserved resources and enabled effective care for low- to medium-acuity, potentially infectious patients at a small Florida community hospital with an embedded family medicine residency. We propose that other clinics with similar resources consider developing or implementing contingency urgent care outdoor clinics, if the climate in their region allows for it. Smaller clinics without similar resources may still be able to adapt some of our practices to their own particular settings.
