Ultrasound has head-to-toe applications for primary care, and the newest machines are portable and affordable enough to fit into almost any practice.
Fam Pract Manag. 2020;27(6):33-40
Author disclosures: Dr. Deutchman is on the medical advisory board of EchoNous, a point-of-care ultrasound device manufacturer. It is an unpaid position. He also owns stock in the company. No other relevant financial affiliations disclosed.
Related article from American Family Physician: "Point-of-Care Ultrasonography."
Family physicians can order a wide range of imaging services for patients. But barriers such as time, money, and physical distance sometimes prevent patients from accessing those services, causing gaps in care. Incorporating point-of-care ultrasound (POCUS) into clinical practice is one way to bridge those gaps.
Technological advancements have allowed more physicians to bring ultrasound services to the office visit or bedside, and to make POCUS an integral part of practice. I [Dr. Deutchman] was an early adopter, adding ultrasound to my rural practice in 1980 after delivering a surprise set of twins in the wee hours of the morning. I have never since been surprised by twins, nor missed an ectopic pregnancy. In addition, I [Dr. Shen-Wagner] first used POCUS during residency in 2011, after a patient complained that it felt like her intrauterine device (IUD) had moved. Everything looked normal on the pelvic exam, but a hand-me-down ultrasound machine from the clinic's obstetrics department revealed the unmistakable flutter of a tiny heartbeat. The patient was pregnant, despite having an IUD for three years.
These are just two examples of the many ways POCUS can benefit doctors and patients. There is robust evidence that POCUS improves care in critically ill patients and improves the efficiency and safety of many invasive ambulatory surgeries that are otherwise performed blindly or by anatomic landmarks.1 There is also preliminary but growing evidence that POCUS can improve diagnostic capabilities, expedite patient care, and inform bedside treatment and management.2,3 Most recently, POCUS has proven to be a valuable tool for confirming COVID-19 diagnoses, as well as monitoring some symptoms of the disease.4
The hands-on, “showing while telling” nature of POCUS advances physical diagnosis skills, fosters doctor-patient communication, and increases patient satisfaction.5 This article outlines some common uses for POCUS and explains how to add it to a practice.
KEY POINTS
Advances in technology have made ultrasound machines more portable and affordable, increasing their accessibility for primary care clinicians.
Point-of-care ultrasound beginners should start with impactful procedures that are easy to perform, simple to interpret, and relatively low liability for both patient and physician. Move on to more complex uses only after those are learned.
Pocket-sized ultrasound machines cost $2,000 to $10,000, plus the costs of gel, probe covers, and cleaning supplies. But several high-yield ultrasound codes can help recoup those expenses.
WHAT IS POCUS AND WHAT IS IT GOOD FOR?
POCUS is a quick, abbreviated study performed and interpreted immediately by the evaluating and treating clinician to help answer clinically impactful questions.
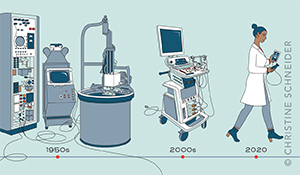
Ultrasound uses have evolved with the technology. The first widely used diagnostic ultrasounds were large, stationary machines that produced grainy still images in the 1960s. Ultrasound in that era was a snapshot in time, performed by a sonographer and interpreted by a radiologist with limited context.
Through decades of advancements those ponderous machines have become pocket-sized devices, capable of pairing with tablets and smartphones to create high-resolution, real-time images, which allows for innovative primary care applications.6 In the hands of a family physician who is familiar with the patient, these applications can expand beyond diagnostics to procedures like endometrial biopsy or IUD placement, among others. POCUS is now being investigated for home visits to extend services beyond the clinic walls.7
For physical exams, POCUS supplements palpation, providing greater sensitivity and specificity.8 It can help identify the best place to insert a needle, especially when traditional landmarks are unreliable because of obesity, or if safety is a concern (e.g., amniocentesis, central line, and paracentesis). For complex questions about a patient's hemodynamics, POCUS can provide multi-organ views pieced together to form an assessment, whereas traditional approaches might require a combination of different types of imaging (e.g., echocardiogram, X-ray, and computerized tomography scan) to arrive at a similar conclusion. (See “Point-of-care ultrasound uses.”)
| POCUS uses | Scope of use | Example questions |
|---|---|---|
| Physical exam extension | Focused | “Is this palpable mass a cystic or solid structure?” “Is the baby in the cephalic or breech presentation?” |
| Procedural | Focused | “Where is the best location to insert a needle?” “Where is the foreign body?” |
| Diagnostic | Focused | “Are there stones in the gallbladder?” “Is there a pregnancy in the uterus?” |
| Multi-organ scans | Extended | “Is the patient's hypotension due to sepsis, heart failure, or acute blood loss?” “What is causing the patient's dyspnea?” |
POCUS, in fact, has “head-to-toe” primary care applications, from ocular ultrasounds to assess elevated intracranial pressure to ultrasounds looking for gout in the big toe. It can examine a specific, limited structure like soft tissue to evaluate lumps and bumps, or provide multi-organ views for undifferentiated complaints such as dyspnea.9
With such a wide range of uses, it can be hard to know where to start. But we recommend beginners start with applications that are easy to perform, simple to interpret clinically, low liability to the physician and the patient, and still clinically useful. (See “POCUS for beginners.”) For example, physicians new to POCUS should not start by scanning for deep vein thrombosis (DVT). The technique is not easy (it requires multi-point compression in specific locations along the affected leg), the interpretation is not simple (it requires knowing anatomical variations and the patient's pretest probability and clinical context), and the liability is high (because there are grave consequences to missing a DVT). It should be left to an experienced ultrasound user.
| Tissue/system | Learn this first | Then proceed to | Transducer type |
|---|---|---|---|
| Skin and soft tissue | Cellulitis vs. abscess | Lumps and bumps | High frequency |
| Musculoskeletal | Knee effusions | Needle guidance | High frequency |
| Pelvis and obstetrics | Bladder obstruction | Intrauterine pregnancy labor and delivery | Low frequency |
| Abdomen | Abdominal ascites | Hydronephrosis | Low frequency |
| Chest | Pleural effusion | Pulmonary edema | Low frequency |
On the other hand, scanning to determine if cellulitic skin has formed an abscess is a great POCUS starting point. It is impactful (it informs the need for bedside incision and drainage), easy to perform (it only requires one or two views), simple to interpret (it involves simple anatomy and limited diagnostic endpoints — either there is a fluid pocket or there is no pocket), and low risk for harm (after learning basic rules to differentiate from a lymph node or vascular structure).
Physicians can then add more complex applications as they gain experience. (See “POCUS multi-organ scans.”)
| Name | Clinical use | Diagnostic targets |
|---|---|---|
| EFAST (Extended Focused Assessment with Sonography for Trauma)1 | Blunt trauma of the abdomen and chest | Free fluid in the abdomen and pelvis, pericardial fluid, and pneumothorax and pleural fluid |
| Labor and delivery2 | Late third trimester exams and labor and delivery | “5 Ps” of pregnancy:
|
| RUSH (Rapid Ultrasound for Shock and Hypotension)3 | Undifferentiated hypotension or signs of shock | Multi-organ protocol to assess for etiology of shock and hypotension |
| CLUE (Cardiopulmonary Limited Ultrasound Exam)4 | Cardiopulmonary dysfunction | Heart, inferior vena cava, and lung views to determine heart failure physiology |
| PEARLS (Parasternal, Epigastric, Anterior lung, Right upper quadrant, Left upper quadrant, and Suprapubic)5 | Core physical exam for generalist (routine inpatient or outpatient use) | A layered, window-based approach to teaching and learning core ultrasound exam |
COMPETENCY, CREDENTIALING AND CERTIFICATION
POCUS does not belong to any one specialty or field. The American Medical Association affirmed in 1999 — and reaffirmed in 2020 — that “ultrasound imaging is within the scope of practice of appropriately trained physicians.”10 The guidelines for determining whether physicians are “appropriately trained” generally fall under the “three Cs”: competency, credentialing, and certification.
Competency is physicians' ability based on their education and demonstrated experience, and is the key factor in determining if family physicians can perform point-of-care ultrasound. Physicians should only begin billing for POCUS after they achieve competency and establish billing and documentation infrastructure. The American Academy of Family Physicians (AAFP) has endorsed recommended POCUS curriculum guidelines for family medicine residents, and as more residency programs begin to incorporate POCUS in their curriculum, it may become a core competency like it is in emergency medicine residency.11 In the meantime, hands-on ultrasound training is increasingly available throughout the year, including sessions geared towards primary care physicians offered by the AAFP, American Institute of Ultrasound in Medicine (AIUM), and American College of Physicians (ACP). There are a handful of primary care ultrasound fellowships (and some emergency medicine fellowships that accept general medicine applicants) across the U.S. that can jumpstart training. There are also free online resources available to supplement hands-on education.
Learners should keep a log of completed scans, but requiring a specific number of scans for competency is controversial because the number varies by physician and by the complexity of the application.
Credentialing is determined by the credentialing body at the physician's local hospital and is often undefined for family physicians. If you are an early adopter at your institution, you may have to self-advocate and carve out a pathway. Reach out to your counterparts in emergency medicine, internal medicine, and critical care to network and support each other in credentialing.
Certification is offered by several national institutions and can streamline the credentialing process, depending on local politics. However, certification can be costly and time-consuming, and should not be viewed as an absolute requirement for using POCUS within family medicine.
| Name | Clinical use |
|---|---|
| American Academy of Family Physicians (AAFP) Procedure Tracker (AAFP members only) | A tool for tracking logged ultrasounds and other procedures |
| AAFP Point-of-Care Ultrasound Member Interest Group (AAFP members only) | A forum with library resources for family physician ultrasound enthusiasts |
| American Institute of Ultrasound in Medicine | A multidisciplinary ultrasound organization that offers procedure-specific practice parameters and YouTube tutorials |
| European Society of Musculoskeletal Radiology | Musculoskeletal ultrasound technical guidelines with images |
| Zedu | Free ultrasound training e-books from an Australian sonography group |
| The POCUS Atlas | A collaborative, evidence-based ultrasound education platform with images for download |
| SonoClipShare by Ben Smith | Software to edit, de-identify, and convert images to GIFs for HIPAA-compliant sharing |
| University of South Carolina Ultrasound Institute | A YouTube Channel with extensive scan video guides |
| Ultrasound Podcast | An emergency medicine ultrasound podcast |
PUTTING POCUS INTO PRACTICE
Placing the ultrasound probe on the patient and getting the image is fun and rewarding, which makes it tempting to skip the administrative tasks and jump right in. But long-term success requires a consistent billing and documentation routine. Ignoring ultrasound administrative tasks could mean lost revenue, lack of justification for new equipment, and legal vulnerability for missing documentation. Some ultrasound scans could be non-billable “quick looks,” such as scanning to monitor therapy, or educational scans by trainees. But most scans should aim to be billable, with documentation in the medical record, independent image reports, and archived representative images, depending on the CPT code. Establishing a good system is therefore key for sustainable scanning.
POCUS documentation. To meet billing requirements, an independent report needs to include these components: two patient identifiers or demographics (e.g., patient name, facility name, date and time of exam, etc.), indication for the ultrasound, adequacy of the scan, description of the findings, and interpretation.12 Documentation and reporting templates can be found in the American College of Emergency Physicians (ACEP) ultrasound standard reporting guidelines.13,14
Documentation should reflect the level of training or stage of ultrasound learning maturation. During the learner stage (whether you are a medical student or a seasoned clinician adopting ultrasound as a new skill), document that you performed an educational ultrasound with the patient's verbal consent and that the purpose of the imaging was strictly educational and not meant to replace clinical judgment or a formal study. If there was a clinical finding, document that you discussed the finding with the patient and document any additional steps taken or studies ordered.
Image archival. Billable scans require images that can be retrieved for audits, to substantiate insurance claims, or for comparison and review down the road. Medicare requires billers to retain images for at least five years, but states may have different rules.15 Though images have to be retrievable, they do not have to be stored within the EHR. There are three ways to store images, each with its own pros and cons.
Device storage: This is a temporary stop for images and needs to be regularly reviewed, backed up, and cleared. This is the easiest option to achieve, but also the riskiest.
Hard drive storage: This is where images can be regularly saved. It needs to have encryption, be checked regularly and backed up, and be stored in a secure location. This is cost effective but labor intensive.
Cloud storage: Images are stored using “middleware” (software that acts as a bridge between a device and an operating system), and then uploaded securely to a server. It's the most secure, but most expensive option.
Image capturing requirements differ for each application. For example, billing for procedural guidance typically requires just one still image of the structure of interest (e.g., the effusion in a knee aspiration). CPT codes for limited scans are generally well-suited to POCUS because they are narrower in scope and require only a few representative images. Complete studies require more documentation. For example, an abdominal aortic aneurysm screening requires captured images and measurements of three segments of the aorta in two planes. Common requirements can be found in the ACEP reporting guidelines and AIUM practice parameters.12,13 Different insurance companies may have slight variations in requirements.
After performing an ultrasound, your first disinfection step should be wiping away any gel left on the ultrasound transducers with a soft clean cloth. Sterile ultrasound gel is recommended, but it can still harbor organisms and, if it is allowed to dry, can make disinfection less effective. Infection risk can be further mitigated with single-use probe covers, which should be discarded promptly after use.
The rest of the ultrasound cleaning and disinfection protocols fall into two categories: lower risk scans (or “non-critical” based on the Spaulding criteria for sterilization of medical devices), which require low-level disinfection (LLD), and higher risk scans (“semi-critical,” per Spaulding), which require high-level disinfection (HLD).
Ultrasound applications that involve scanning intact skin and no mucous membranes require only LLD. Multiple passes with a commercial disinfecting wipe readies the equipment for the next use. Commercial wipes and sprays have varying wet contact times to be effective, which should be listed on the packaging. Ultrasound manufacturers can recommend cleaning agents that won't corrode equipment. If disinfecting wipes are not available, soap and water is acceptable. The ultrasound can also be sufficiently cleaned in this manner after certain percutaneous procedures and needle guidance, if you use a disposable probe cover and sterile gel.
Ultrasound applications that include contact with mucous membranes (vaginal or rectal mucosa) or non-intact skin (such as burns or stasis ulcers) require HLD. In addition to using probe covers and an appropriate commercial disinfectant wipe, the user should also put the equipment through a series of chemical washes made specifically for medical products (e.g., Cidex or MetriCide) or in an aerosolized hydrogen peroxide misting machine (e.g., Nanosonics' trophon).
In the era of COVID-19, physicians should pay special attention to disinfection before and after scanning. Most commercial wipes are effective against the novel coronavirus, with variations in contact time that can be confirmed on the Environmental Protection Agency's website.18
ECONOMIC CONSIDERATIONS IN IMPLEMENTING POCUS
A variety of entry-level ultrasound units are now affordable for individual physicians, and some companies allow physicians to rent equipment as well as buy it. (See “Pocket-sized ultrasound models.”)
| Model | Probes | Applications | Price | Comment |
|---|---|---|---|---|
| VScan Extend by GE (2009, 2014) | Dual probe, linear, and sector on each end | Musculoskeletal (MSK), abdomen, cardiac, and obstetrics (OB) | $2,995–4,995 per unit. No subscription fee. | Display unit included. Separate battery packs extend scanning time. Does not require internet updates. Projects to a TV screen using Anycast. Local device storage and exports to DICOM PACS. |
| IViz by Sonosite (2015) | Linear, curvilinear, and sector | MSK, abdomen, cardiac, and OB | >$10,000 per unit. No subscription fee. | Display unit included. Does not require internet updates. Includes access to Sonosite Institute. Local device storage and exports to DICOM PACS. |
| Lumify by Philips (2015) | Linear, curvilinear, and sector | MSK, abdomen, cardiac, OB, and biometrics | $3,995–6,000 per unit. No subscription fee. $199/month rental. | App-based, displays on a separate Android phone or tablet. Internet updates. Remote guidance with REACTs. Local device storage and exports to DICOM PACS. |
| Clarius by Clarius (2016, 2019) | Linear, curvilinear, and endocavitary | MSK, abdomen, OB (with transvaginal), and biometrics | $2,500–6,900 per unit. No subscription fee. | Cordless. App-based, displays on a separate iOS/Android phone or tablet. Internal battery. Local device and cloud storage and exports to DICOM PACS. |
| IQ by Butterfly (2017) | Single probe with high and low frequency | MSK, abdomen, cardiac, OB, and biometrics | $1,999 per unit plus subscription fee ($420–1,200 per year). | App-based, iOS- or Android-compatible, displays on a separate phone or tablet. Internet updates. Remote guidance with TeleGuidance.* Internal battery. Projects using Apple TV. Cloud storage and exports to DICOM PACS.† |
Make sure any device you purchase has Food and Drug Administration approval before using it on patients. If you are employed by a hospital system, your employer may require institutional approval before you can use ultrasound in patient care (outside of educational scans). Reimbursements are determined by the type of scan performed and the practice setting (e.g., hospital-employed physicians will need to use modifier -26 to bill only the professional component).
Entry-level ultrasound devices cost between $2,000 and $10,000. Some offer annual subscriptions for features like HIPAA-compliant cloud storage, tutorials, and advanced imaging presets. Those are the startup costs. There are also per-procedure costs. When bought in bulk, single-use packets of sterile gel generally cost $1–$2, and disposable probe covers cost about $0.25 each. LLD cleaning products are generally less than $0.25 per use, and HLD chemical washes cost about $50 per gallon.
Family physicians can perform a number of POCUS procedures that yield Medicare reimbursements of $50–$125 (see “POCUS coding”). These far outweigh the per-procedure costs, allowing physicians to recoup startup expenses within a reasonable timeframe, although a warranty to hedge against breakdowns of the ultrasound device may be considered, depending on the cost. That's just one of many things to consider when adding ultrasound to a practice. However, there have never been more free resources and hands-on CME workshops to help family physicians do it. Technological advancements have brought more user-friendly interfaces, increased portability, and lower costs. The latest POCUS models even include telemedicine capabilities to interact with experts remotely, and artificial intelligence to increase diagnostic support, making interpretation easier.19 With time, effort, and practice, any motivated physician can incorporate ultrasound into clinical practice.
| System | Applications | CPT code | Comment | Medicare reimbursement* |
|---|---|---|---|---|
| Musculoskeletal | Ultrasound-guided injection/aspirations of a major joint or bursa | 20611 | Combined code; do not bill separately for the injection | Non-facility $96.72 Facility $62.44 |
| Limited ultrasound exam of arm/leg joint, tendon, or muscle | 76882 | $58.10 | ||
| Ultrasound-guided needle placement for abscess aspiration | 76942 | Bill separately for the incision and drainage (10160) | $58.47 | |
| Limited soft tissue exam with ultrasound | Codes differ by body part. Examples: Upper back, 76604 Lower back, 76705 Extremity, 76882 | Varies by body part: 76604 $80.48 76705 $92.75 76882 $58.10 | ||
| OB/GYN | Limited pelvic exam for pregnant patient (transabdominal) | 76815 | $85.53 | |
| Limited pelvic exam for non-pregnant patient (transabdominal) | 76857 | $49.44 | ||
| First trimester pregnancy dating (transabdominal) | 76801 | <14 weeks pregnant, single fetus | $124.51 | |
| Transvaginal ultrasound | Pregnant, 76817 Non-pregnant, 76830 | No separate limited code. Use modifier -52 to indicate reduced services | 76817 $97.44 76830 $125.23 | |
| Abdomen | Limited abdominal exam (e.g., gallbladder, renal, bladder) | 76705 | $92.75 | |
| Abdominal aortic aneurysm screen | 76706 | Do not use G0389 (code deleted in 2017) | $115.85 | |
| Chest | Limited chest exam | 76604 | To identify pleural effusion and A-/B-line artifacts | $80.48 |
| Limited echocardiography | 93308 | $100.69 |