Durable medical equipment helps patients live healthier, more independent lives. Here's how to minimize the hassles of getting it to them.
Fam Pract Manag. 2021;28(2):15-20
Related AFP article: Mobility Assistive Device Use in Older Adults
Author disclosures: no relevant financial affiliations disclosed.

Patients depend on durable medical equipment (DME) to function independently in their homes and communities. But fulfilling DME requests for patients can be time-consuming and burdensome for physicians. Getting the equipment often requires collaboration between multiple parties: the primary care physician and staff, the patient and family, the insurance company, and the equipment supplier. Common hurdles in the DME process include the complexity of the equipment, lack of standardized workflows, and variable insurance coverage requirements. In many practices, there may also be a lack of clarity surrounding the workflow. This can cause delays in patients receiving their DME and may even prevent some patients from ever receiving it. That increases risks to patient health, decreases patient satisfaction, and spurs staff frustrations.
But there are ways for practices to streamline the process, once they better understand it. This article includes a brief overview of DME regulations, tips for navigating them more efficiently, and several templates we have found useful in our practice.
KEY POINTS
Patients often depend on durable medical equipment (DME) to function in their homes and communities.
Getting DME ordered, authorized, and delivered can be challenging for physicians and staff, leading to delays in patients receiving their DME.
DME delays can cause safety risks, decreased patient satisfaction, and increased staff frustrations.
Designating a staff DME expert and developing templates for DME documentation and orders streamlines the process so patients can obtain their equipment quickly.
RULES AND REGULATIONS
As with most aspects of medicine, the Centers for Medicare & Medicaid Services (CMS) has created rules and regulations for DME. First, the agency has guidelines for what qualifies as DME under Medicare. The equipment must be durable (can withstand repeated use and generally lasts at least three years), used for a medical reason, not typically useful to someone who is not sick or injured, and used in the home.1
DME that meets this definition and is medically necessary is covered under Medicare Part B. Medicare sets an approved price for each type of equipment. Patients have to pay 20% of that amount, and their Part B deductible applies as well. Coverage varies somewhat based on the type of DME (for example, patients may be eligible to have some items replaced sooner than others). Although private insurers tend to use Medicare as a guide, they may have their own rules about what is covered and what isn't. All of this has implications for patients' upfront and ongoing costs.
STREAMLINING THE PROCESS
Given the complex nature of DME, it is not unusual for care teams to struggle with the approval process. Certain strategies, however, can make it easier.
Apply Lean principles. A group at Cincinnati Children's Hospital Medical Center used Lean methodologies (a set of principles for achieving efficiency commonly used in the corporate world) to standardize and streamline its DME ordering process.2 By using value stream mapping, a time study, and flow diagrams, the team identified the parts of the process that needed improvement, including initial processing, obtaining signatures, returning forms, and uploading completed documents. After the implementation of standard practices, the group's median lead time for DME requests (the time between receiving and completing them) decreased from 50 days to three days. The median processing time (the time staff worked on each request) decreased from 14 minutes to nine minutes, leading to a cost savings of $11,000 a year.
Develop a staff expert. Some tasks within a medical practice need to be spread across a large number of staff or geographic regions. But ordering DME is one task that may be accomplished more efficiently when it's funneled through one or a few staff members who already have experience and expertise, or can quickly gain it. Given the complexity of regulations and variation between orders, having one or more people well-versed in DME will quickly pay dividends. Someone who knows all the rules can expedite the DME process and keep everyone from going down a path that leads nowhere. In our large academic family medicine practice, we designated management of our DME processes to a full-time registered nurse, with some support from medical assistants working under her guidance.
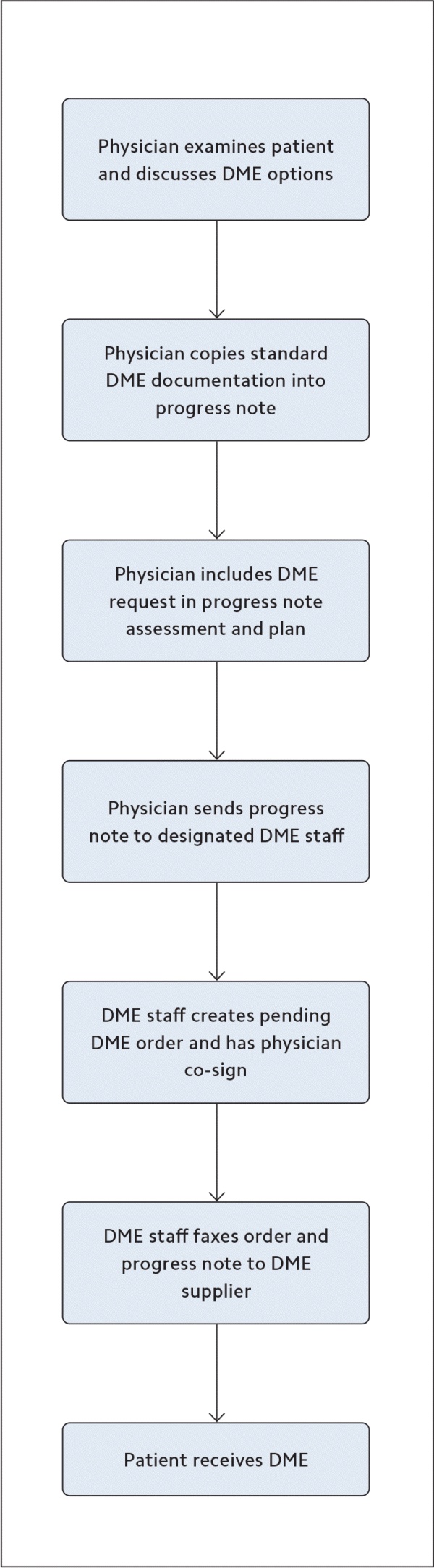
Reverse the process. Once you have your DME expert in place, consider reversing the typical ordering process. Instead of the physician (or qualified health care professional) readying the order and passing it off to staff for fulfillment, have staff ready the order based on the physician's documentation and then route it to the physician to co-sign before sending. (See “Ideal DME workflow.”)
Standardize documentation. A key aspect of DME billing and approval is physician documentation of the medical need for the equipment. For some items, documenting that need is straightforward (such as a patient who needs a prosthetic limb due to a recent amputation). In other cases, it may not be. We've found that the DME items with the most complicated requirements are wheelchairs, hospital beds, gel overlays, and oxygen. So, for these items, we've developed templates of the information required in progress notes for face-to-face encounters. Power mobility devices like scooters can also be difficult to get approved because of the many regulations that govern them. Therefore, we've created a separate table with a brief summary of the Medicare requirements that guide patient eligibility, plus templates to aid in ordering mobility devices and documenting the need for them (see “Power mobility devices”).
DME DOCUMENTATION TEMPLATES
| Wheelchair | Hospital bed | Gel overlay | Oxygen |
|---|---|---|---|
|
AND MORE THAN ONE OF THE FOLLOWING:
|
AND MORE THAN ONE OF THE FOLLOWING:
|
OR:
|
| Power mobility devices | |||
|---|---|---|---|
| Guidance | Order template | History/physical exam template | Assessment/plan template |
For Medicare to reimburse for a power wheelchair (PWC) or power operated vehicle (POV) such as a scooter, several requirements must be met:
| – Order specifics – EQUIPMENT DESCRIPTION: Power mobility device. Dispense: 1 with 0 refills. Anticipated length of need: 99 DIAGNOSIS (and ICD-10 code): Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | HISTORY:
EXAM: Diagnosis of medical condition requiring power mobility device: [condition]
[Insert rest of exam.] | Ambulatory dysfunction due to: [diagnosis].
|
Standardize ordering. Given the amount of information required in many DME orders, it is helpful to have templates that prompt you to enter required elements for a given piece of equipment (we have included some of our own in this article). Some orders may need to include a patient's height and weight, for example, while others need to have the date of last office visit. Many EHRs can be set to alert you when a required piece of information is missing.
Based on CMS guidelines, discussions with DME companies, and expertise from DME clinical staff, we have compiled a list of 10 commonly required elements for Medicare coverage of DME.
TEN COMMONLY REQUIRED ELEMENTS FOR DME ORDERS
Equipment description
Dispense quantity and number of refills
Anticipated length of need (estimated in months, enter “99” if indefinite)
Diagnosis and ICD-10 code
Most recent height
Most recent weight (if > 300lbs, include “bariatric size” in equipment description)
Patient name and date of birth
Home address
Insurance company
Member ID
The five DME items most commonly ordered in our practice are rolling walkers, canes, incontinence supplies, nebulizers, and commodes. We've created templates for these orders that include many of the required elements. (See “DME ordering templates.”) We've also included templates for ordering wheelchairs and hospital beds — items that aren't as common for our practice but may be useful for practices with more elderly or frail patients — and a generic template for “other DME.”
| Cane | Rolling walker | Nebulizer | Incontinence items |
| – Order specifics – EQUIPMENT DESCRIPTION: Cane Dispense: 1 with 0 refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): Difficulty walking (R26.2) Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: Rolling walker Dispense: 1 with 0 refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): Difficulty walking (R26.2) Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: Nebulizer machine with neb kits, tubing, and filters Dispense: 1 machine and appropriate supplies Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): [diagnosis] FOR USE WITH: [medication type and dosage] Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: Incontinence suppliesDispense: [amount] with [number] refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): Mixed incontinence (N39.46) Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: |
| Commode | Wheelchair | Hospital bed | Miscellaneous |
| – Order specifics – EQUIPMENT DESCRIPTION: Commode Dispense: 1 with 0 refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): Gait and mobility abnormalities (R26.9) Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: 1 wheelchair and supporting equipment (light/standard weight wheelchair with anti-tippers, seatbelt, cushion, and elevating leg rests) Dispense: 1 with 0 refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): Difficulty walking (R26.2) Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: Hospital bed Dispense: 1 with 0 refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): [diagnosis] Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: | – Order specifics – EQUIPMENT DESCRIPTION: [description] Dispense: [amount] with [number] refills Anticipated length of need: 99 [or fewer months if temporary] DIAGNOSIS (and ICD-10 code): [diagnosis] Height: Weight: – Demographics – Patient name: DOB: Home address: Insurance info: Member ID: |
IN SUMMARY
Getting patients the DME they need can be an arduous process, but these items are often life-changing. Developing standard templates for common DME orders and designating a staff expert to shepherd those orders to quick fulfillment can increase your practice's efficiency in this area, cutting costs and improving quality of care.