2019 NRMP Match Marks Decade of Growth for Family Medicine
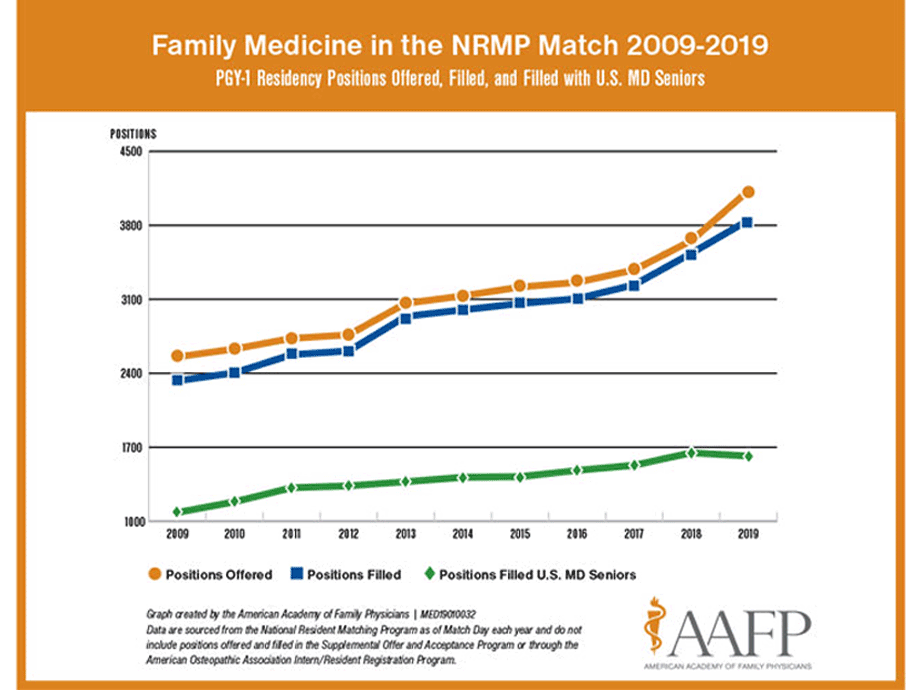
March 15, 2019 03:05 pm Sheri Porter – There's some big news following the release today of results from 2019 the National Resident Matching Program Main Residency Match (NRMP Match). Shout this from the rooftops: 2019 marks a full decade of year-over-year growth for family medicine.
This year also marks seven years running that the specialty is able to brag about a new all-time record for the number of medical students matching into family medicine in the NRMP Match.
Count it out: 3,848 medical students and graduates just matched into family medicine -- 313 more than matched to family medicine residency programs in 2018.
Overall, combining totals from the NRMP Match and the February American Osteopathic Association Intern/Resident Registration Program (AOA Match), family medicine filled 112 more positions than in 2018 (4,152 versus 4,040).
Add to that figures from December's Military Match, which brought another 132 students into the family medicine column. Of those, 52 positions were gained in the Air Force, 41 in the Navy and 39 in the Army.
AAFP President John Cullen, M.D., of Valdez, Alaska, extended his congratulations to all of the new recruits.
"I'd like to personally welcome our new family medicine colleagues. We're proud to have you join our ranks. Know that you are an important part of our team now and in the future."

Andrea Pittman and Garrett Dunn attend Match Day festivities at the University of Alabama School of Medicine in Birmingham, where they hold a carefully customized sign proclaiming "'We' matched in family medicine." The engaged couple will attend Texas A&M Family Medicine Residency in Bryan, Texas.
In an interview with AAFP News, Cullen said, "These students who have chosen family medicine get it -- they understand that family medicine is the hardest, yet most rewarding, specialty in all of medicine.
"Given family medicine's broad scope of practice, these soon-to-be residents can forge their own paths in a field overflowing with opportunity."
Readers should know that AAFP Match calculations include students matching into traditional family medicine residency programs, as well as programs that combine family medicine education with other specialty training. Those additional programs are family medicine/emergency medicine, family medicine/preventive medicine, family medicine/psychiatry, and family medicine osteopathic neuro-musculoskeletal medicine.
Story Highlights
Additional Match Highlights
Not all the news was good, however. The 2019 Match numbers revealed that 1,617 seniors graduating from U.S. M.D.-granting medical schools matched to family medicine compared with 1,648 seniors in 2018.
Yes, that number represents a decline, and it's the first year-over-year dip in the past decade.
However, it's important to note that family medicine added more positions in the 2019 Match -- 474, to be exact -- than in any year in recent history.
AAFP experts told AAFP News that although some of the increase in number of positions is due to the growth and expansion of residency programs, the vast majority likely is attributable to the transition to a single accreditation system.
That five-year process of shifting residency programs and students from the AOA Match to the NRMP Match is nearly complete. The final AOA Match occurred last month.
In an interview with AAFP News, AAFP Senior Vice President for Education Clif Knight, M.D., sorted out the situation in "perfect-storm" fashion.
"A slight decrease in the number of U.S. M.D. seniors matching to family medicine residencies, paired with the significant increase in the number of positions offered in family medicine -- plus the likely increase in osteopathic students matching into family medicine -- has resulted in a fill rate for U.S. M.D. seniors of 39.2 percent -- the lowest we've seen to date," said Knight.
He noted that figures showing the precise number of osteopathic students who matched to family medicine are not yet available from the NRMP.
The AAFP does know that 306 students matched to family medicine in the AOA Match and that family medicine numbers in that Match have cycled downward since 2016 as those students transitioned to the NRMP Match.
Staff experts noted that family medicine has historically been a top specialty choice for students graduating from D.O.-granting medical schools and hope to see that positive trend continue in this year's NRMP Match and beyond.
Deeper Dive
Knight, a former residency program director, cautioned that the dip in U.S. senior numbers is a red flag signaling that the U.S. health care system does not credit family medicine with the value the specialty brings to patients and to the country as a whole.
"Medical students sense that lack of value and can see, in policy and payment strategies at state and local levels, the hesitancy to fully invest in primary care," he said. "And in many medical schools, students face an academic culture and curriculum that de-emphasize primary care and especially family medicine.
"For far too many students, these intuitive insights and unfortunate realities lead them to make alternative specialty choices," Knight added.
He pointed out that some medical schools are doing a good job of producing family physicians and lauded the efforts of those institutions.
Ranjani Natarajan is all smiles as she shows off her 2019 Match letter that confirms she's headed to Pennsylvania to attend the University of Pittsburg Medical Center combined Family Medicine and Psychiatry Residency program. Natarajan will graduate from Albany Medical College in New York.
"The AAFP applauds the family medicine faculty and family medicine advocates at these institutions where people have worked together to create solutions that often run against the grain of the systems in which they work."
Readers can see for themselves; review two lists of medical schools that contribute the most to the U.S. family medicine workforce that are published, along with relevant research findings, in the March 2019 issue of Family Medicine.
Knight also reflected on the infusion of D.O.-trained physicians into the family medicine family.
"It's wonderful to see osteopathic students contributing in a significant way to the growing number of U.S. students entering family medicine residencies," he said. In fact, in 2018, the ratio of D.O.-to-M.D. matches was seven osteopathic students for every 10 allopathic students.
Those numbers are encouraging, as is an upward tick in the number of new osteopathic medical schools, as well as more seats in those medical school classes.
Moving Forward
What lies ahead for family medicine? Lots of hard work, Knight acknowledged.
He noted that nearly a decade ago, in December 2010, the Council on Graduate Medical Education issued its 20th report, titled Advancing Primary Care, which called for a number of changes to spur the growth of primary care in the United States.
"The system still has not achieved most of the changes called for in that report," said Knight.
Among those recommendations were calls to
- increase the percentage of primary care physicians in the workforce to 40 percent;
- add to the number of primary care residency positions;
- up the output of primary care physicians by U.S. medical schools;
- adjust the disproportionate pay between primary care and subspecialty care;
- reward and incentivize practice models that improve patient care and health outcomes, and decrease costs;
- increase incentives for physicians to practice primary care and other critical specialties in physician shortage areas;
- reform medical education to promote the choice of careers in primary care; and
- recruit and train underrepresented students and faculty, including those from racial and ethnic minority groups, as well as students from rural backgrounds and those with disadvantaged socioeconomic backgrounds.
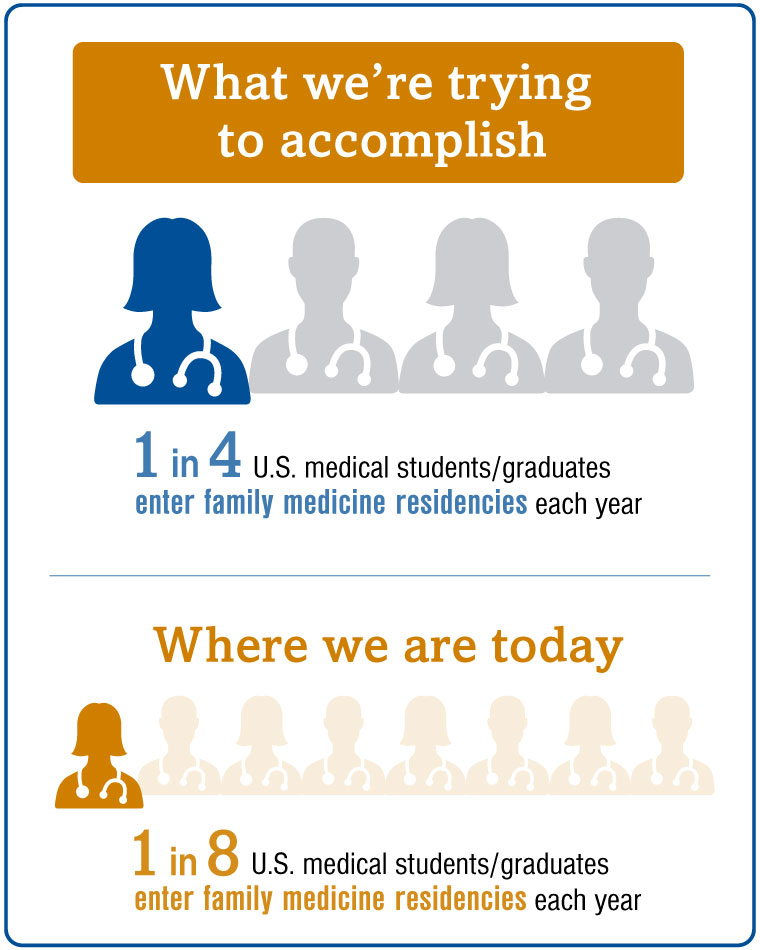
Knight also gave a shout out to an initiative the AAFP and seven other national family medicine organizations have taken on to increase the proportion of U.S. medical students who pursue family medicine residency training to 25 percent by the year 2030.
One focus of that initiative, the America Needs More Family Doctors: 25 x 2030 collaborative, aims to create a learning community to support U.S. medical schools as they strive to learn best practices from the schools that are achieving the best results in producing students who match into family medicine residencies.
The 25 x 2030 initiative also aims to increase interest in family medicine careers among students who are underrepresented in medicine and to do so early in the medical school pipeline.
Cullen included some action items of his own directed at family physicians in the field.
He challenged his family medicine colleagues to engage students and show them the possibilities available with a career in family medicine.
"No matter where you practice or the size of your practice -- you can show medical students what family medicine is all about. It doesn't matter if you practice in a clinic in an urban setting, suburban America, a small rural community or a remote frontier town in Alaska," said Cullen.
"Patients in all of these settings deserve a family physician."
He urged his colleagues in practice to do their part. "Invite students to spend some time in your clinic and absorb the atmosphere. Allow them to feel what's it like to be a family physician.
"Because seeing firsthand the difference we make in our communities and in our patients' lives can really make an impact on students as they consider their career choices."
Related AAFP News Coverage
Researchers Calculate Medical School Production of FPs
More Family Physicians Could Crush Primary Care Shortage
(3/15/2019)