Mentor Shares His Passion for Learning
January 11, 2021, 12:08 pm David Mitchell — After Emmanuel Kenta-Bibi, M.D., M.P.H., M.S.M.Ed., M.B.A., graduated from medical school in 1997, he worked as a general practitioner in his native Cameroon for three years. When he decided to immigrate to the United States seeking “greener pastures,” he knew it would mean giving up his practice and resuming his training.
“It’s different there,” he said. “You’re a GP when you graduate, and you go straight into the trenches, caring for patients, delivering babies and performing general surgery. It was extremely hard to start over, but once you’re determined to do something, you have to keep working at it and look at your ultimate goal. I knew learning more would benefit me in the future.”
Since arriving in the United States two decades ago, Kenta-Bibi has added three degrees and a physician executive certification to his curriculum vitae.
“My passion is learning and passing on that information,” said Kenta-Bibi, an assistant professor of family medicine at the University of Connecticut School of Medicine and faculty at the Middlesex Health Family Medicine Residency Program.
Before he could start his own residency training, Kenta-Bibi had to complete all the steps required of international medical graduates, including Step 1 and Step 2 of the United States Medical Licensing Examination. So, he worked in public health for two years as an emergency response coordinator for the health district that includes Bristol and Burlington before matching into the family medicine program at Middlesex Health.
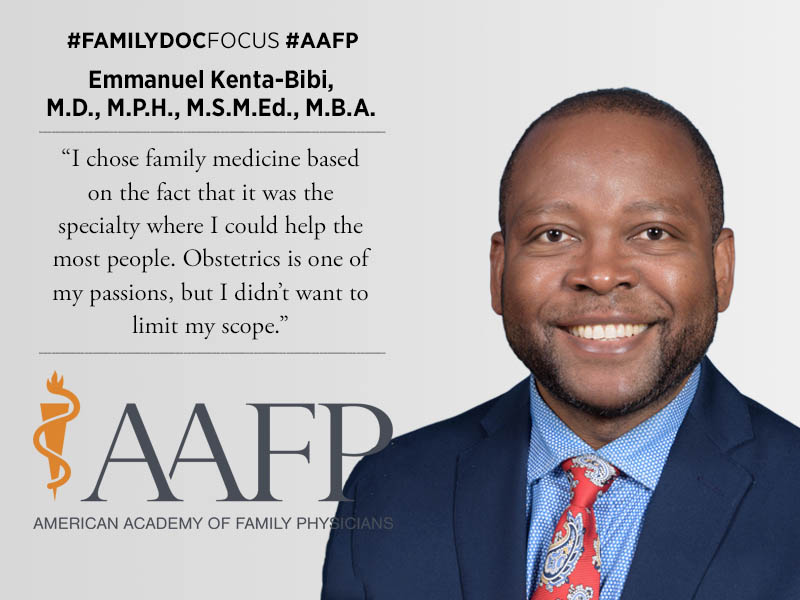
“I chose family medicine based on the fact that it was the specialty where I could help the most people,” said Kenta-Bibi, whose wife, Eucharia Kenta-Bibi, M.D., is also a family physician. “Obstetrics is one of my passions, but I didn’t want to limit my scope.”
During his training, Middlesex expanded from a three-year program to a four-year format. Although the new requirement didn’t apply to his class, Kenta-Bibi opted to stay an extra year.
By adding an extra year, Middlesex residents can focus on specific training tracks, including academic medicine and maternity care. Kenta-Bibi used the extra time to earn his master’s degree in medical education.
“It allows flexibility for residents to master these things,” said Kenta-Bibi, who continues to practice full-spectrum family medicine with obstetrics. “Our residents have more training, more experience and a higher number of patient visits.”
According to Middlesex, the program’s residents complete their training with 40% more clinical exposures than those in a traditional program.
Kenta-Bibi has taken on a number of leadership roles in his community. At Middlesex Hospital, he chairs the Patient Safety and Quality Committee and the Readmission Steering Committee.
Roughly 20% of all Medicare patients are readmitted within 30 days of discharge. The Medicare Payment Advisory Commission has estimated that 12% of readmissions could be avoided and that preventing 10% of such readmissions could save Medicare $1 billion a year. Since 2012, CMS has penalized hospitals with excess readmissions, and Kenta-Bibi said Middlesex Hospital has been able to greatly reduce these penalties.
“We have looked at the reasons why people come back and focused on transitions of care to avoid readmissions,” said Kenta-Bibi, who also is a medical advisor to the six-town Chatham Health District.
Kenta-Bibi’s leadership also extends to the state level. He has been on the Board of the Connecticut AFP since 2012 and is serving as the chapter’s president this year.
“Advocacy work is very important and necessary for family physicians,” he said. “Our role is not only treating individual patients. We go beyond that and look at our communities and address issues with health disparities.”