Lifting up and representing minority voices through family medicine
Sept. 17, 2025, David Mitchell — Melissa Campos, MD, FAAFP, noticed a glaring disconnect between patients and health care professionals during the two years she volunteered in a New Haven, Connecticut, emergency department.
Although a significant percentage of the patients spoke Spanish, few of the hospital’s staff had the same ability.
“I was just astonished,” said Campos, who earned her undergraduate biology degree at Yale University. “There’s a large community that speaks Spanish, but a majority of the physicians and nurses did not speak the language. Patients were confused, scared and nervous. I was just a little volunteer, but I helped translate for the doctors. The patients were more comfortable, having felt understood and being able to understand what was happening to them.”
A few years earlier, Campos had been left to wonder if her own grandfather, an immigrant who developed cirrhosis from alcoholism, might have had a different outcome if he had been able to better communicate with his physicians.
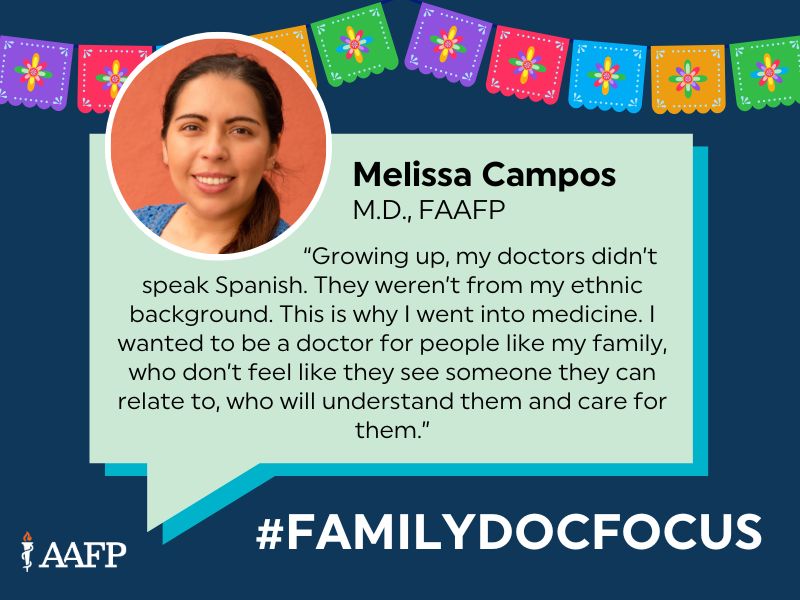
“If someone had spoken his language, maybe they could have made a difference and given him a little more time with our family instead of the quick ending that he had,” she said. “There are wonderful doctors everywhere, but I think it’s important to have a doctor who looks like you and who understands where you’re coming from. Growing up, my doctors didn’t speak Spanish. They weren’t from my ethnic background. This is why I went into medicine. I wanted to be a doctor for people like my family, who don’t feel like they see someone they can relate to, who will understand them and care for them.”
During the AAFP’s National Conference of Constituency Leaders, which met April 24-26 in Kansas City, Missouri, Campos was elected co-convener of the BIPOC (Black, indigenous, people of color) constituency. She also will be a member constituency alternate delegate when the Academy’s Congress of Delegates meets Oct. 4-6 in Anaheim, Calif.
“That was a really cool experience and just really awesome to see how across the United States, a lot of these family docs are thinking about the same issues,” said Campos, a past president of the San Diego AFP. “There are variations, depending on state issues, but overall, we care about the same things. It was really wonderful to connect on a national level. I’m interested in being more involved in CAFP, leadership and working on improving diversity representation within family medicine.”
Campos is doing her part to bolster the workforce as faculty and assistant program director of the Scripps Chula Vista Family Medicine Residency in Chula Vista, California, where the population is 61% Hispanic.
“Our program attracts a lot of Latino residents,” said Campos, who is a graduate of the residency program. “The community is predominantly Latino underserved. A lot of the residents either come from that type of community or want to work with that community.”
Campos serves on a California AFP committee focused on diversity issues, and she serves on the board of Latinas in Medicine, a local organization that provides mentoring, workshops and scholarships for high school, college and pre-med students interested in health care careers.
“I want to pay it back and help others who may not have the support network or resources to get there,” she said. “If you have a passion for this, there really shouldn’t be barriers.”
After graduating from Yale, Campos spent two years working at the Scripps Research Institute in La Jolla to earn money for medical school. Her work was focused on studying cocaine addiction in rats.
“They were cute and cuddly, and the work that the lab was doing was really important to help with substance use disorder,” she said, “but it was not something that I had my heart in. I really missed human connection. I was more interested in working with actual people and trying to make a more immediate impact.”
Campos entered Tufts University School of Medicine in Boston with an interest in emergency medicine, but her rotations led her to family medicine.
“I found that family medicine was where I can have the most impact, trying to prevent illness and coordinating care,” she said. “That’s also how I discovered that I liked doing a little bit of everything.”
Campos had worked as a tutor from high school through medical school and got a chance to teach as a resident when she participated in the AAFP Foundation’s Emerging Leader Institute. Her project focused on teaching public health to high school students.
“I got to do that during second year of residency, and I had a lot of support for my program and co-residents,” she said. “We expanded that in my third year of residency to include fun, hands-on workshops for topics like suturing.”
Campos stayed at Chula Vista for a fourth year as chief resident.
“I got to keep doing a lot of the youth pipeline pathway programming,” she said. “I love doing that, but I also got to empower the residents as a chief and work with them on didactics, supervising them on inpatient, on OB, on nursing home rounds. I stayed on and kept doing it, and I’m still here as faculty.”