RLS Speaker Played Key Role in New Program Requirements
Jan. 9, 2024, David Mitchell — The group visit concept was fairly new when Stacy Potts, M.D., M.Ed., FAAFP, was a medical student at the University of Vermont in the 1990s. But there was Potts, forming and leading group visits for patients with diabetes during her family medicine clerkship in a tiny ski village.
Potts and the practice’s nurse practitioner facilitated monthly meetings for roughly a dozen patients that covered topics like nutrition, eye health and foot care. The learning experience, she said, was unheard of for medical students at that time.
“It was incredible,” she said. “Regardless of what clerkship I was on, I would go back there for that once-a-month meeting with them for the rest of medical school. It was wonderful to keep going back to that community and caring for those same patients. The best thing was that the patients taught each other as much or more than I could as a medical student. Their lived experiences and work with each other was amazing.”
More than two decades later, Potts is still looking for novel approaches to education and health care. She’ll be a main stage speaker during the Residency Leadership Summit March 24-27 in Kansas City, Mo.
RLS drew record attendance last year when the conference was held a few months before new program requirements for family medicine took effect. Potts expects interest in that topic to remain high this spring.
“I definitely think there’s still a lot to learn,” said Potts, who served seven years on the Accreditation Council of Graduate Medical Education’s Review Committee for Family Medicine, including four years as chair. She also served two years as chair of the writing group that drafted the new requirements. “This will be the first year that people are trying to integrate the new requirements, so they have a lot to learn from each other.”
The new requirements, which allow residents more flexibility and elective time, were years in the making. The AAFP and six other family medicine organizations engaged thousands of students, residents and family physicians in focus groups and surveys leading up the fourth Starfield Summit in December 2020.
Potts said it was important for the specialty to “imagine what family medicine could contribute to the future of health care in the country” rather than “just tweaking” the existing requirements.
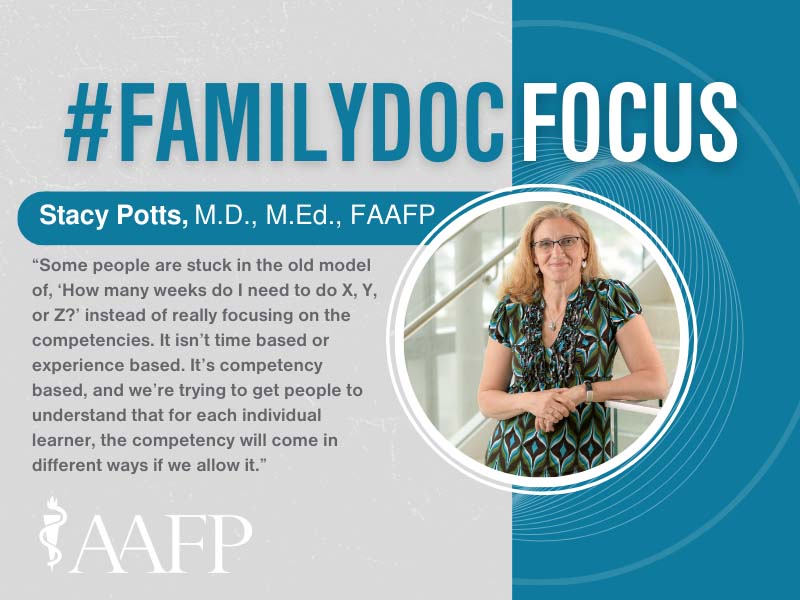
Her RLS presentation will focus on the competency-based approach to medical education and the individualized learning experiences for residents that are key components of the new requirements.
“Some people are stuck in the old model of, ‘How many weeks do I need to do X, Y, or Z?’ instead of really focusing on the competencies,” Potts said. “It isn’t time-based or experience-based. It’s competency based, and we’re trying to get people to understand that for each individual learner, the competency will come in different ways if we allow it.”
Potts’ influence extended beyond family medicine last summer when she became senior associate dean of graduate medical education and clinical affairs at the University of Massachusetts Chan Medical School in Worcester. In that role, she oversees 65 accredited GME programs and 22 non-standard programs that serve nearly 700 trainees.
“I really love this new role even more than I thought I would,” she said. “It’s a lot of fun to work with the different programs and program directors.”
Potts spent two decades in the Worcester Family Medicine Residency in assistant, associate and program director roles before becoming vice chair of education in the UMass Department of Family Medicine and Community Health in 2020. She later spent a year as the department’s executive vice chair. In those roles, she was involved in faculty development, undergraduate and medical education, as well as graduate medical education.
“It was hard to leave family medicine and to move into this other world,” she said, “but it gives me a lot of opportunities to support program directors and it’s a great new challenge to think about graduate medical education at the higher level. It also gives me an opportunity and a voice in the institution.”
Potts, who teaches residents as a professor in the Department of Family Medicine and Community Health, continues to serve family medicine in a variety of national leadership roles. She has been core faculty for the AAFP’s Chief Resident Leadership Development Program for more than a decade.
She said it’s a privilege to mentor the future leaders of the specialty.
“It’s a real investment in a residency program to have the chiefs participate in leadership development,” she said. “It empowers them to do more for their programs and to manage a lot of the day-to-day tasks. The leadership program helps them understand how to manage a crisis, but it also helps them be proactive about improving the program. It’s a great opportunity for all programs, but particularly programs that are starting out should consider getting their chiefs to this conference.”
Potts is in her second year as an Academic Council member for the Association of Family Medicine Residency Directors’ National Institute for Program Director Development fellowship, and she serves on multiple Family Medicine Education Consortium committees and work groups. She also is involved in multiple AAFP initiatives focused on growing the family medicine workforce, including serving as co-chair of the new Family Medicine Champions program.
She still devotes nearly one-third of her time to clinical care.
“At my core, I’m a full-spectrum family doc, and I care for a small town here in Massachusetts,” she said. “I still deliver babies, and now I’m delivering the babies of babies who I delivered, which is awesome. The real joy is taking care of people for decades, knowing my patients like I do and sharing that with learners and having them understand what it’s like to have that longitudinal relationship.”
Those relationships are what Potts envisioned years ago when she returned again and again to the Vermont practice of family physician Francis Cook, M.D.
“The thing I loved about that practice was that it was like home to everybody who worked there and everybody who came in,” Potts said. “They had an X-ray machine and did all kinds of procedures because it was the only health care facility in a big area. They dealt with urgent care for skiers and the tourists would pop in with their issues. One of the things I’ll never forget is Dr. Cook answering the phone himself sometimes. It seems like such a little thing, but I just remember seeing that and thinking, ‘That’s what I want, a small town practice where it’s like a family.'”