Discussing Medications for Patients With Cognitive Impairment
December 06, 2019 02:12 pm Michael Devitt – Although family physicians are known for their ability to manage care for patients of all ages, discussing medication use with older patients who have cognitive impairment can be challenging for even the most skilled FP.
And given the heightened burden of comorbidity these patients typically face -- and the attendant risks of polypharmacy -- the stakes are particularly high.
A recent study in the Journal of General Internal Medicine examined how FPs and other primary care clinicians discuss medication use with older adults who have cognitive impairment and their companions. The study's authors found that clinicians use a variety of approaches to ensure that patients understand and can participate in decisions about medication use, while also noting several challenges that could prevent clinicians from working with patients and companions effectively.
"Family physicians and their teams are uniquely positioned to assist patients with cognitive impairment, as well as their caregivers," Julie Wood, M.D., M.P.H., the Academy's senior vice president for health of the public, science and professional activities, told AAFP News. "This study affirms that using a whole-person approach while considering the patient's priorities and quality of life can be helpful with communication and shared decision-making about their medications and overall care and treatment."
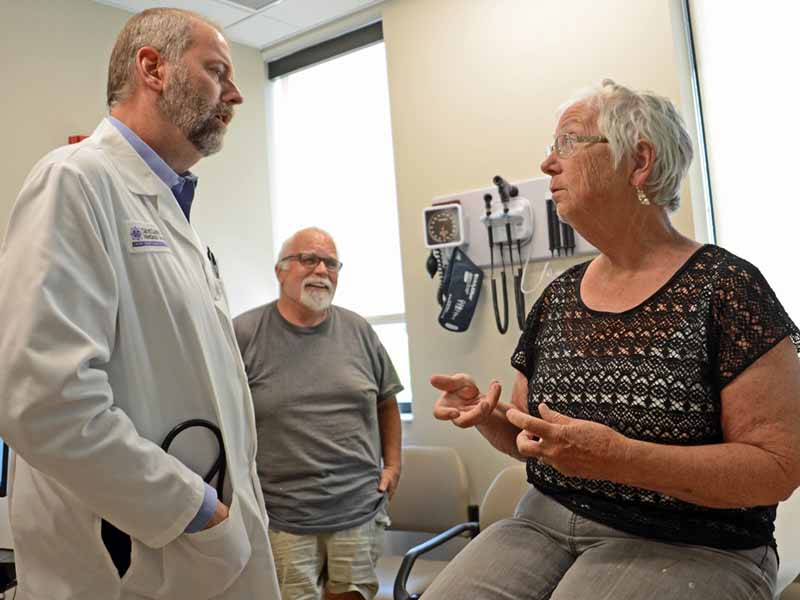
Former AAFP President Michael Munger, M.D., of Overland Park, Kan., understands that having another set of ears in the exam room can be helpful when it comes to discussing patient care plans and medications, sometimes even for patients without cognitive impairment, as in this visit.
Study Details
The researchers analyzed audio recordings and transcripts of primary care visits from the 2018 SAME Page trial, which involved 14 clinicians and 93 older adults with cognitive impairment and their companions. The trial was designed to examine the effects of a patient-family agenda-setting checklist on communication during visits. Six clinicians were family physicians, and six clinicians had additional specialty training in geriatrics.
Patient diagnoses and medication lists were obtained by reviewing patients' EHRs. At enrollment, all patients took the Mini-Mental State Examination. Two weeks later, patients and companions completed a questionnaire that asked about medication adherence and the quality of their communication with the clinician.
Patients averaged 79.9 years and had an average MMSE score of 21.6. Slightly less than half of enrolled patients had a diagnosis of dementia, cognitive impairment or symptoms of cognitive impairment in their EHR, and about one-fourth of patients were taking 10 or more prescription medications.
Findings
Three key themes emerged from the patient visits.
- Principles of optimal drug prescribing. Clinicians used a variety of approaches to introduce patients and companions to some of the basic tenets of prescribing medications. For example, they
o talked about scaling back the number and intensity of medications as a routine part of care to reduce treatment burden and improve quality of life;
o explained how the balance of benefits and harms of medication use can change over time;
o tried to prioritize patient function and quality of life over treating the disease;
o outlined the concept of diminishing returns in this context;
o explained that medications cannot always fix a patient's symptoms and sometimes carry significant risks; and
o acknowledged the sensitive nature of making decisions about medications in older adults with cognitive impairment and comorbid conditions. - Working with patients and companions as partners. Clinicians frequently asked patients and companions for their perspective to get them involved in the conversation. They reassured patients that stopping a prescription was not the same as withdrawing appropriate care and emphasized that they would continue to closely monitor patients after stopping a medication to check for symptoms.
- Circumventing barriers. Clinicians had to work around various challenges to optimal prescribing, including behavioral and psychological symptoms associated with dementia; patients' or companions' expectation that medication would be prescribed; clashes between clinician recommendations and patient or companion preferences; three-way conversations, especially when the patient and companion were at odds; and trying to balance disease-based guidelines against medication side effects, patient quality of life and treatment burden.
Overall, a majority of patients (52.4%) and companions (62.6%) who responded to the question about the quality of the medical communication with the clinician rated it as excellent. Older patients and those with lower average MMSE scores were more likely to rate the medical communication as poor, fair or good.
Takeaways
"Cognitive impairment is one of the most challenging illnesses that primary care clinicians address because of the behavioral and psychological complications and because of structural barriers," the authors wrote.
"Even if a clinician recognizes a medication as potentially inappropriate or a candidate for withdrawal, talking about deprescribing is difficult, especially in the context of cognitive impairment, with its prolonged and uncertain trajectory," they continued.
The authors suggested that future efforts center on providing clinicians with resources to make it easier for all stakeholders to share in decision-making about medication use.
They also called for more research on how patients and companions interpret and respond to these conversations, as well as for strategies to help clinicians overcome technical and logistical barriers that draw time away from discussing appropriate medication use.
FP Perspective
Sarah Coles, M.D., of Phoenix, a member of the AAFP's Commission on Health of the Public and Science and chair of an Academy panel charged with developing a dementia guideline, acknowledged that addressing medication use in older adults with cognitive impairment can be challenging and stressed the importance of FPs knowing and implementing strategies to improve the experience for both physicians and patients.
"This includes keeping the patient front and center in the conversation, focusing on quality of life, and reducing risks of unnecessary medications," Coles said. "We must emphasize that this does not mean that we are 'giving up' on treating the patient or that they are not 'worth' the medication, but that we will remain with them and partner together to make sure our medical care is meeting their needs, values and goals."
Coles called out the important role companions and caregivers play, explaining that some patients may not fully understand their symptoms or may feel uncomfortable discussing personal difficulties. Companions can fill in those gaps by offering information on a patient's history or identifying issues that have not been addressed, in addition to providing patient care.
"Caregivers also are at high risk of burnout and stress," she noted. "As family physicians, we should routinely address the well-being of the caregiver,"
Finally, Coles shared some best practices derived from personal experience.
"When seeing patients with cognitive impairment, I try to include the patient and caregivers for all discussions and treatment planning," she said. "This should start with clarifying what the patient's concerns might be, what are that person's goals and values, and what concerns the caregiver may have.
"The visit should include a thorough medication reconciliation to identify any polypharmacy and consideration of which medications could be removed to simplify the regimen, reduce risks of medication use, and improve quality of life," Coles continued. "I emphasize that this is a partnership, and the patient is the most important member of our team."
To assist in these discussions, Coles recommended that FPs use resources such as the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults from the American Geriatrics Society. She also recommended a recent American Family Physician article, "Polypharmacy: Evaluating Risks and Deprescribing," which contains helpful tips and suggestions for FPs.
Related AAFP News Coverage
FPM Showcases Tools Available to Improve Dementia Care
(4/17/2019)
More From AAFP
AAFP Cognitive Care Kit
American Family Physician: AFP By Topic: Geriatric Care
Additional Resource
The Conversation Project