Inside Look at Using Telemedicine During COVID-19 Pandemic
Family Physicians Describe Their Experiences
March 23, 2020 08:00 am Chris Crawford – As the number of cases of confirmed COVID-19 -- the disease caused by the novel coronavirus SARS-CoV-2 -- skyrockets in the United States, family physicians are consumed with trying to best care for their patients while protecting themselves and their staff.

That's why telehealth has become such a useful tool for providing care for these patients.
And right on cue, the AAFP recently updated its guidance on using telehealth to specifically address caring for patients during the COVID-19 pandemic.
Tips included in that guidance address how to quickly implement telemedicine in a practice, how to get reimbursed for virtual visits and what codes to use for COVID-19. Additionally, there is specific guidance on Medicare payment requirements for these telehealth sessions.
Another great resource that allows family physicians to share their experiences using telemedicine during the pandemic is the COVID-19 Rapid Response Member Exchange, a newly created online community that includes various threads about virtual visits and related issues.
Notes About CMS Reimbursement
In one such thread about CMS reimbursement for telehealth, Steven Waldren, M.D., vice president and chief medical informatics officer for the AAFP, said documentation requirements for any form of virtual care ("telehealth service" or non-telehealth digital online service) are the same as those for documenting in-person care.
"If a code is time-based, evidence of time must be documented," he said. "If exchanged asynchronously, videos, images and communications must be stored, for billing purposes, and retained for a duration pursuant to state regulation. Real-time (synchronous) videos, such as during a video visit, or video phone call (temporarily permissible for billing purposes) are not required to be stored."
STORY HIGHLIGHTS
To bill for an office visit with place of service code 02, Waldren said there must be a real-time video component of the visit, a requirement that he said the AAFP is working to get waived.
To accomplish a video visit, he said there already are some telemedicine products on the market that practices can use. Several examples are included on the Academy's telehealth page.
Additionally, FaceTime or Skype can now be leveraged to perform video visits with patients. Patient-informed consent was required before HHS' Office for Civil Rights announced it would use its discretion authority to not enforce some HIPAA requirements during the pandemic, although care providers are still encouraged to notify patients that these third-party applications potentially introduce privacy risks, and they should enable all available encryption and privacy modes when using such applications.
Waldren said additional details are available in an FPM Getting Paid blog post covering telehealth rules and procedure codes for testing COVID-19 that was updated March 17 to include additional context and updates.
Family Physicians on the Frontlines
Gina Tobalina, M.D., of El Dorado Hills, Calif., told AAFP News her practice closed its doors to in-person visits this week, converting fully to video visits.
"Our volume is down, as we rescheduled all physicals and wellness visits out until June," she said. "All acute care and routine follow-up visits will be done by 100% video visit."
The practice's staff includes Tobalina and four part-time advanced-level practitioners who use EpicCare Ambulatory EMR software and have offered video visits since May 2019.
"I would describe the difficulty level of converting to full video visits as moderate," she said. "The obstacles have been patients who need help using their smartphones and navigating the steps to use an app and connect to a video visit. This is more noticeable in our over-65 population."
Patience is a virtue in this situation, and Tobalina said for the patients who cannot get connected, the visit is converted to a telephone call.
The practice has used the updated CMS billing codes for COVID-19 but hasn't received any feedback one way or another yet.
As for the response from patients so far, Tobalina said they love their video visits.
"They are relieved to be able to connect with us and to see our faces," she said. "It offers a lot of reassurance to them. They are worried about us, too, and they are glad to hear that we are OK and up and running. There are no apologies needed as they are so thankful to be able to see and hear us."
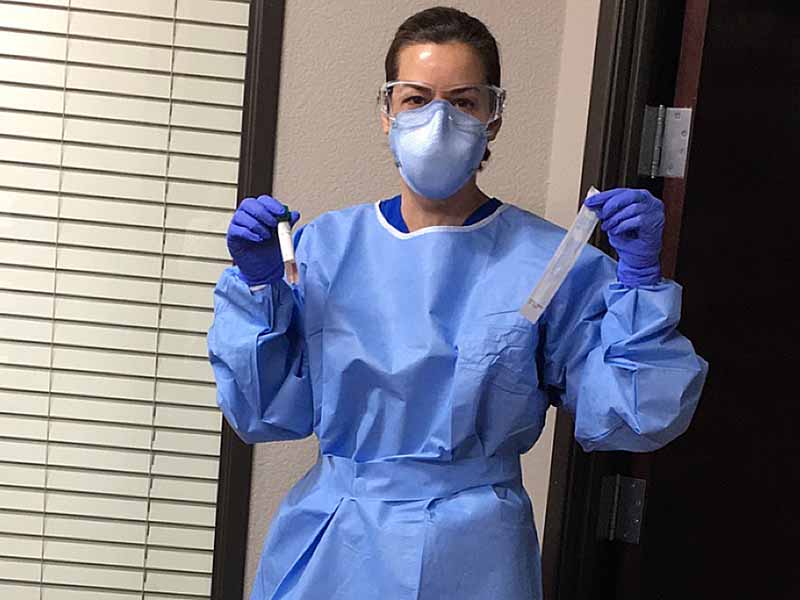
Converting to telemedicine also provides the benefit of not worrying about adequate test kits or N95 masks or other personal protective equipment. Before going virtual, Tobalina said she was testing for COVID-19 in-office while wearing PPE, and she will continue to drive into the office to test patients with suspected cases in the parking lot.
She said routine vaccines for children will continue to be given in the parking lot, as well, with the children in their parents' cars while the attending staff wear full PPE.
"I'd like to highlight the confidence and comfort it brings me to know that other doctors are doing this and doing it well," she said. "We need to rely on each other for support, both tactically and emotionally."

Sinclair McCracken, M.D., of Newport News, Va., told AAFP News that her office also is now 100% virtual, using the HIPPA-compliant platform Doxy.me, which they chose to use the same week they stopped in-person visits.
"It allows video to be seen while documenting in the EMR," she said. "We use Nextgen and have our staff using HIPPA-compliant laptops from home and office cellphones to call patients to instruct them how to do it."
This practice with one physician, one physician's assistant and six staff members doesn't have access to COVID-19 test kits or PPE, so it had to stop seeing sick patients last week.
"Now, we are able to 'see' patients, screen for the drive-through testing that is available at a local hospital, treat other acute illnesses and manage their chronic problems, and keep them clear of an urgent care or ER," McCracken said.
In addition, the practice changed its voicemail to offer numbers to call staff directly.
"From the least to the most tech-savvy patients, ranging in ages from 20 to 80, they agreed and adapted and were 'seen' successfully the next day," she said. "We were all logged into our electronic record remotely, working together during office hours. We were essentially '100% virtual' in 24 hours. My physician's assistant, office manager and staff really did a great job working together to make this work."
McCracken said the group reviewed the CMS coding recommendations and documentation requirements but said it would take a while to see how the codes they submitted are reimbursed.
Like many areas of the country, COVID-19 testing in Newport News has been very limited, she said.
"We are unable to test without kits and without PPE," McCracken said. "Our entire state had only 450 or so kits, as noted by Gov. (Ralph) Northam. Local hospitals procured tests and set up drive-through testing but have run out in two days. These limitations make it logistically impossible to care for our patients in an office setting due to risk of disease transmission."
Drive-through screening at the local hospital sites, she said, required meeting two of three criteria: fever of at least 100.4°F, cough and shortness of breath, and you've either traveled internationally or to an area with a known COVID-19 outbreak or been in close contact with someone with confirmed or suspected to have COVID-19.
"If you don't meet those criteria, the hospital encourages people to stay home, call their primary care physician, and continue to follow the CDC's recommended prevention methods," McCracken said.
As for family physicians still lacking adequate resources, McCracken recommended that members use the AAFP's Speak Out feature to reach out to their congressional representatives and request stronger support for COVID-19 coordination.
"I sent a letter March 17 from the AAFP email link suggesting all family physicians should have immediate access to telemedicine to ensure we can take care of our patients and do our part to mitigate the COVID-19 outbreak by doing what we do best: coordinating care, managing acute and chronic illnesses, and preventing unnecessary emergency room visits and hospitalizations," she said. "We know our patients well and are well-equipped with the strength of today's technological advances to make this happen."