Risk-Stratified Care Management Algorithm and Rubric
Risk stratification is a systematic way to group patients by risk level so that physicians can make care decisions that improve health and reduce costs.
You can support your practice's population health management efforts with risk-stratification tools (tools that are completely free for AAFP members). Appropriately risk stratifying your patient population can help your care team identify who would benefit from reminders and follow-ups under a care management program.
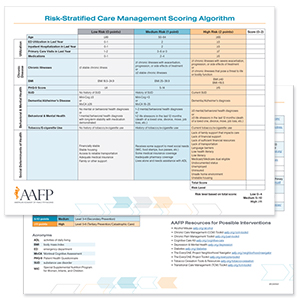
Risk-Stratification Algorithm
Stratify patients into three risk levels based on utilization, chronic disease, behavioral and mental health and social determinants of health with a streamlined algorithm.
How the algorithm works:
This tool enables practices to generate a score and associated risk level to identify patients who may benefit from longitudinal care management services.
While many practices have access to a registry or population health system, this tool can be helpful for implementing RSCM in practices that do not.
Once a patient’s score and risk level are determined, the care team can use the RSCM Rubric to identify care plan suggestions and opportunities for planned care, if appropriate.
Member: $0
Nonmember: $50
Getting started with value-based care? Find the education and tools that will help you make changes that count most for your patients.
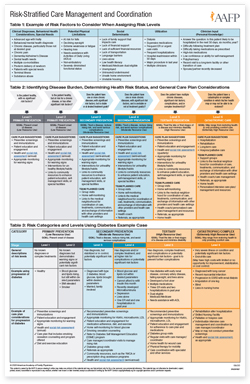
Risk-Stratification Rubric
Guide yourself and your care team through the process of stratifying patients into six risk based levels on health severity, social determinates and utilization of services.
The rubric includes:
- framework on how to identify and assign patient's health risk level
- care plan suggestions
- a diabetes example case illustrating different risk-levels and associated care plan suggestions
Member: $0
Nonmember: $50
"We got data back that one patient had been to the ER more than 40 times in the year before, and it was always on a weekend. My care manager started calling him every Friday morning to ask, ‘Do you need to be seen? Do you need any refills?’ And like that, the following year, he went to the ER maybe twice.”
Wondering if VBC is for you?