
Am Fam Physician. 1998;57(8):1778-1783
to the editor: Herpes simplex virus is a common oral pathogen in immunocompetent patients. Herpes esophagitis, however, is usually an opportunistic infection but can also occur in immunocompetent hosts.
A 27-year-old female presented with complaints of fever, myalgia, sore throat and lingual swelling; she was given a prescription for erythromycin. Two days later, she complained of pleuritic chest pain and severe odynophagia. The patient had no history of oral contraceptive use or pregnancy, no recent antibiotic or corticosteroid use and no risk factors for human immunodeficiency virus (HIV) infection. Pill esophagitis was suspected, and azithromycin (Zithromax) was substituted for erythromycin. Four days later, the patient was prescribed nizatidine (Axid) for “esophagitis” and was referred to the author for GI evaluation.
On physical examination, the patient was afebrile. Examinations of the oropharynx, heart and lungs were normal.
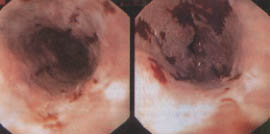
Esophagogastroduodenoscopy (EGD) showed a diffusely inflamed esophagus with hemorrhage and ulceration in the mid-esophagus (see figure). Histology showed severe ulcerative esophagitis without evidence of Candida organisms or viral infection.
The patient's clinical syndrome had nearly resolved when a viral culture, obtained at EGD, demonstrated herpes simplex virus infection. No antiviral therapy was prescribed.
The patient lives with her mother, who is immunosuppressed. Three days prior to the onset of the patient's symptoms, her mother had begun taking acyclovir (Zovirax) for culture-proven oral herpes simplex virus infection.
The true incidence of herpes esophagitis in immunocompetent hosts is underestimated. First, herpes esophagitis is not suspected in normal hosts, particularly in the absence of odynophagia or oropharyngeal lesions. Indeed, there have been reports of herpes esophagitis without oral involvement in normal hosts who have not suffered chest pain or odynophagia.1 Additionally, patients with severe herpes gingivostomatitis may have unrecognized herpes esophagitis if they are not questioned about esophageal symptoms or have only subtle dysphagia because of limited oral intake. Since herpes esophagitis in immunocompetent hosts is self-limited, these patients may be misdiagnosed when they “respond” to gastric antisecretory treatment or other empiric measures.
Esophageal histology in immunocompetent patients with herpes esophagitis usually demonstrates intranuclear inclusions and giant cell formation, unlike in our case.2,3 When these hallmarks of viral infection are absent—and viral infection is not clinically suspected—diagnostic confusion can result.4 Viral culture has greater diagnostic sensitivity than histology or cytology.1,5 If our patient had not received a viral culture, her illness might have been erroneously attributed to severe gastroesophageal reflux disease.
Immunocompetent patients with herpes esophagitis do not require antiviral therapy; spontaneous recovery is expected.6 Our patient was most likely infected by her mother, although both women may have contracted herpes simplex virus infection from another source. Another report of a patient with herpes esophagitis presumes the virus was contracted from the patient's spouse, who had a prior “fever blister.”7
Herpes esophagitis should be included in the differential diagnosis of patients with acute esophageal complaints. This diagnosis may spare the patient unnecessary therapies such as those our patient received. In addition, these patients can be cautioned against exposing themselves to individuals who are susceptible to opportunistic infections. Finally, immunocompetent patients with herpes esophagitis can be reassured that their acute and frightening symptoms will rapidly subside.