
Am Fam Physician. 1998;57(8):1813-1822
Head and neck manifestations of acquired immunodeficiency syndrome (AIDS) are among the most common complications of this disease. Some of these manifestations are the initial signs of human immunodeficiency virus (HIV) infection, and others are associated with full-blown AIDS. Otologic manifestations include otitis externa, otitis media, Kaposi's sarcoma and sensorineural hearing loss. Nasal and oral manifestations of AIDS are more common than otologic manifestations and range from infections, caused by both opportunistic and nonopportunistic organisms, to malignancies. We address common manifestations and current treatment recommendations.
Human immunodeficiency virus (HIV) infection can be called the epidemic of the 20th century. It is estimated that by the end of the 1990s, 10 million people worldwide will be HIV-positive. By 1996, more than 581,400 cases of acquired immunodeficiency syndrome (AIDS) were reported in the United States, of which 357,598 were fatal.1 Although longer survival periods have been achieved, thanks to antiretroviral drugs and better treatment of complications, the mortality rate remains at almost 100 percent. In addition, it is estimated that there may be 10 times more HIV-infected persons as there are patients with AIDS.
It was reported initially that 41 percent of patients with AIDS had head and neck manifestations. As awareness has increased, however, recognition of these lesions has also increased, until it now seems that nearly 100 percent of patients with AIDS have head and neck manifestations.2 The primary care physician and the otolaryngologist play pivotal roles in both diagnosis and management of these conditions. It is of utmost importance that clinicians recognize these manifestations at an early stage, so that prompt treatment can be undertaken. The most common head and neck complications of AIDS are listed in Table 1.
| Otologic | |
| Otitis externa | |
| Serous otitis media | |
| Kaposi's sarcoma | |
| Eustachian tube dysfunction | |
| Sensorineural hearing loss | |
| Nasal and sinus | |
| Cutaneous | |
| Kaposi's sarcoma | |
| Herpes simplex ulcers | |
| Herpes zoster | |
| Noncutaneous | |
| Adenoid hypertrophy | |
| Eustachian tube obstruction | |
| Acute/chronic sinusitis | |
| Oral | |
| Recurrent aphthous ulcers | |
| Condyloma | |
| Candidiasis | |
| Hairy leukoplakia | |
| Herpes simplex | |
| Gingivitis | |
| Stomatitis | |
| Periodontitis | |
| Kaposi's sarcoma | |
| Non-Hodgkin's lymphoma | |
| Squamous cell carcinoma | |
| Neck | |
| Generalized lymphadenopathy | |
| Neck mass (due to infection with Mycobacterium tuberculosis, Mycobacterium avium complex, cryptococcosis, histoplasmosis or coccidioidomycosis) | |
| Parotid gland cyst | |
Ear Manifestations
In general, otologic manifestations are less common than other head and neck manifestations. Some of the more common complications include otitis externa, serous otitis media, Kaposi's sarcoma, eustachian tube obstruction secondary to nasopharyngeal mass, acoustic brainstem response abnormalities and sensorineural hearing loss secondary to central nervous system complications.2
External Ear
The incidence of otitis externa (Figure 1) is not increased in the AIDS population. Most infections of the cartilaginous external auditory canal in HIV-positive persons are caused by routine organisms and resolve with standard therapy. Otitis externa is typically caused by Pseudomonas aeruginosa and, less commonly, Proteus or Aspergillus species. Predisposing factors are excessive irritation or mechanical trauma.2 Patients usually complain of hearing loss and severe pain that increases with manipulation of the auricle. On examination, the ear canal may be edematous and erythematous, with purulent debris within it. Treatment requires suctioning the exudate and instilling topical antibiotic ear drops. Commonly used ear drops are otic suspensions combining antibiotics and a steroid.3 Otic wick placement may be required to help in delivery of antibiotic ear drops in patients with severely obstructing canal edema.

As well as diabetic or immunocompromised patients, persons with AIDS and otitis externa are predisposed to malignant otitis externa or osteomyelitis of the skull base. Clinical evidence suggesting malignant otitis externa includes severe, progressive pain, fever and granulation tissue within the ear canal. The causative agent is usually P. aeruginosa. The incidence of otitis externa evolving to bacterial or fungal malignant otitis externa, however, does not appear to be higher in the AIDS population than in other immunocompromised patients.2,4 Treatment requires combination intravenous antibiotics and, possibly, surgical debridement.
Kaposi's sarcoma is the most common malignant manifestation of AIDS (Figure 2). It is 20,000 times more common in the AIDS population than in the general population.5 Kaposi's sarcoma of the external ear most commonly occurs in patients with AIDS. Involvement of the ear, the ear canal, the tympanic membrane or the middle ear causes conductive hearing loss.

Treatment of Kaposi's sarcoma varies with the degree of symptomatology and the site of involvement. If the lesion is asymptomatic and the patient is not requesting removal of the lesion, it can be left untreated, with periodic follow-up examinations. Argon laser removal is the treatment of choice if Kaposi's sarcoma involves the tympanic membrane and/or the auricle. Carbon dioxide laser is preferred for the removal of Kaposi's sarcoma involving the external auditory canal. Radiation therapy to the external canal or intralesional chemotherapy can be used in patients with extensive localized lesions. Systemic chemotherapy is also an option in patients with extensive or disseminated Kaposi's sarcoma. Outcome of treatment varies with the activity of HIV disease and the extent of immunosuppression.3
Middle Ear
Serous otitis media, (i.e., middle ear effusion without inflammation) is more prevalent in the adult AIDS population than in the general population.2 It can result from a malfunctioning eustachian tube secondary to recurrent viral infections, adenoidal hypertrophy, nasopharyngeal tumors or allergies.6
Unilateral or recurrent serous otitis media warrants evaluation of the nasopharynx to rule out large benign or malignant nasopharyngeal tumors. These lesions present as nasal obstruction, hearing loss, otitis media and recurrent serous otitis media. The presence of large lymphoid proliferation of the adenoids (Figure 3) in a patient should prompt the physician to obtain a good history of risk factors and to perform serologic testing for HIV. Adenoidectomy is the treatment of choice, to relieve obstruction in the eustachian tube and obtain biopsy specimens to rule out lymphoma and Kaposi's sarcoma, both of which occur at higher frequency in HIV-infected patients.7–9 In patients with nasopharyngeal carcinoma, radiation therapy is the treatment of choice.

Acute otitis media is common in patients with AIDS. Symptoms, causative agents and treatment of acute otitis media are similar in patients with AIDS and in the general population. The predominant agents are Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis. Oral ampicillin and amoxicillin are the antimicrobial agents indicated in the treatment of otitis media. β-lactamase–inhibiting factors should be added to the regimen in patients with β-lactamase–producing H. influenzae and M. catarrhalis infection. In toxic patients and those refractory to standard therapy, tympanocentesis should be performed to identify uncommon or resistant pathogens.2 In cases of infection with penicillin-resistant pneumococcus, treatment with the extended-spectrum macrolides clarithromycin (Biaxin) and azithromycin (Zithromax) may result in enhanced bacteriologic eradication compared with penicillin treatment.
Otitis media and mastoiditis caused by Pneumocystis carinii are uncommon opportunistic otologic infections unique to patients with AIDS. An aural polyp is frequently found in the external auditory canal or middle ear that, on biopsy, reveals a typical P. carinii cyst if stained with Grocott-Gomori methenamine–silver nitrate. P. carinii gains access to the middle ear in three ways: (1) it can extend retrogradely through the eustachian tube from a colonized nasopharynx, (2) it can spread medially from the external auditory canal or (3) it can seed the temporal bone hematogenously.2 Oral trimethoprim-sulfamethoxazole (Bactrim, Septra), in a dosage of 15 to 20 mg per kg per day in three to four divided doses for 21 days, is very effective in eradicating the organism.
Inner Ear
As many as 20 to 50 percent of HIV-positive patients have sensorineural hearing loss.9 Since HIV is a known neurotropic virus, sensorineural hearing loss may be explained by direct involvement of the eighth cranial nerve, although no pathologically documented case has been reported.9 On the other hand, central nervous system complications of AIDS, such as cryptococcal meningitis or neurosyphilis, can also cause sensorineural hearing loss.10,11 Evaluation includes a complete audiogram, speech and impedance audiometry, and acoustic reflex testing. Retrocochlear pathology can be assessed by acoustic brainstem response testing. Cerebrospinal fluid should be sent for detection of Treponema pallidum and cryptococcal antigen. Hearing aids can benefit patients with significant hearing loss.2
Nasal and Sinus Manifestations
Nasal Manifestations
Nasal complications of HIV infection and AIDS are very common, presenting in 40 to 70 percent of patients.9 Cutaneous lesions include Kaposi's sarcoma, herpetic infection, seborrhea-like dermatitis and herpes zoster. Some of these lesions may be the first signs that disease is advancing from asymptomatic HIV infection to AIDS.12 Herpes zoster involvement of the fifth cranial nerve can be a sign of decreasing cellular immunity. Activation of the latent varicella zoster virus in the trigeminal ganglion leads to burning pain, dysesthesia and characteristic vesicular eruptions in the dermatomal distribution of the trigeminal nerve. Typically, patients present with vesicles along the external ear and the jaw area. Treatment with acyclovir (Zovirax), famciclovir (Famvir) or valacylovir (Valtrex) can shorten the course of varicella zoster virus activation and may prevent postherpetic neuralgia.12
Patients with AIDS may also have giant herpetic ulcers, which commonly originate in the nasal vestibule and can extend to involve the nasolabial region. The lesion can be diagnosed by history and clinical appearance, and the diagnosis can be confirmed by culture or Tzank smear. Acyclovir, famciclovir or valacylovir can be used to shorten the course of chronic or frequently recurrent disease.9 Foscarnet (Foscavir) can be used in resistant cases; however, it is an intravenous drug and quite toxic.
Nasal obstruction and congestion are caused by a wide range of disorders and occur often in HIV-positive patients. A common cause of this manifestation is adenoidal hypertrophy.13 In fact, the presence of this lesion in an otherwise asymptomatic adult patient should always raise the suspicion of HIV infection. It is thought that infection with HIV, Epstein-Barr virus or cytomegalovirus causes proliferation of B cells in lymphoid adenoidal tissue. The usual presenting symptoms are nasal obstruction and recurrent serous otitis media secondary to eustachian tube obstruction. Adenoidectomy and bilateral tympanostomy with tube placement are indicated for symptomatic relief in patients refractory to medical therapy.12
Systemic high-grade B-cell lymphoma is becoming increasingly common in patients with AIDS.8 This fact may be explained by the increase in survival time, which allows for the development of this malignancy. Patients with nasal lymphoma usually have epistaxis, rhinorrhea and nasal obstruction. This neoplasm can be diagnosed by needle aspiration or tissue biopsy. Treatment is aggressive systemic chemotherapy which, unfortunately, could have serious complications in already immunocompromised patients. Radiotherapy is reserved for patients with mass-effect abnormalities involving the orbit, face or airway.12,14
Sinus Manifestations
The prevalence of rhinosinusitis ranges from 20 to 70 percent in patients with AIDS. Sinusitis is a spectrum of inflammatory diseases involving the nose and paranasal sinuses. This spectrum includes acute and chronic sinusitis, with or without mucopurulent post-nasal drainage (Figure 4). Causative organisms include atypical opportunistic organisms (Figure 5), as well as agents responsible for sinusitis in hosts without AIDS. Opportunistic fungal sinusitis is caused by organisms such as Alternaria alternata, Aspergillus, Pseudallescheria boydii, Cryptococcus and Candida albicans.9,15,16 Interestingly, the incidence of zygomycosis is not higher in HIV-infected patients as it is in diabetic patients. The organisms that cause acute sinusitis in both immunocompromised and immunocompetent populations include S. pneumoniae and H. influenzae. Staphylococcus aureus and P. aeruginosa are more commonly associated with chronic sinusitis.17
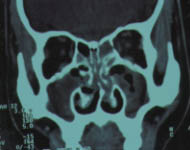

Just as in hosts without HIV infection, HIV-positive patients with sinusitis have signs and symptoms of fever, general and localized headaches, and mucopurulent drainage from sinus ostia. Computed tomographic (CT) scan of the sinuses determines the extent of disease. Medical outpatient therapy for sinusitis is often effective and includes treatment with a combination of antibiotic and decongestant for three weeks. Amoxicillin-calvulanate potassium (Augmentin), trimethoprim/sulfamethoxazole double-strength or cefuroxime (Ceftin, Kefurox, Zinacef) are better than amoxicillin alone. Oral pseudoephedrine or similar decongestants can be used in combination with the antibiotic.12

Oral Manifestations
Recurrent aphthous ulcers are common among HIV-positive persons. These are solitary or multiple lesions that occur on the nonkeratinized mucosa of the oral cavity. They vary in size, ranging from 1 mm to 2 cm. They are well circumscribed, with an erythematous halo, and tender to palpation. Topical steroids or topical anesthetics provide symptomatic relief. Biopsy may be considered in patients with large recurrent aphthous ulcers (1 to 2 cm in diameter), which mimic malignant lesions.18
Immunosuppressed persons have an increased tendency to develop warts, including those involving the oral cavity. These lesions are caused by human papillomavirus and present in three variant forms: cauliflower, spikey and flat (focal epithelial hyperplasia). Surgical or laser excision of these lesions is the treatment of choice, despite their tendency to recur.18
Oral candidiasis is the most common abnormal finding in patients infected with HIV and is often an indication of poor prognosis for long-term survival. Oral candidiasis can take several forms and appearances, the most common of which is a pseudomembranous white plaque that can be scraped off. Scraping the lesions reveals an erythematous bleeding base. The atrophic form is erythematous and tender to touch. The hyperplastic form has thick, peaked white plaques that cannot be scraped off, most commonly involving the buccal mucosa. Angular cheilitis appears as an erythematous erosion of the oral commissure with erythema of adjacent skin.7,19
C. albicans is the most common of the 80 species of candida that cause these lesions. Potassium hydroxide preparation of the surface scraping reveals the characteristic mycelia, spores or hyphae.7
Treatment varies according to the degree of immunosuppression in the patient. For minimally immunocompromised patients, nystatin (Mycostatin, Nilstat, Nystex) solution swished and swallowed five times daily is often successful.
In moderate cases of immunosuppression, systemic antifungal agents are used, such as fluconazole (Diflucan), at 200 mg for the first dose, then 100 mg once a day for several days to several weeks, depending on the severity of disease and the response of the patient to treatment.20 Prophylactic use of antifungal agents is indicated in patients with frequent episodes (e.g., fluconazole in a dosage of 100 mg orally once a week).7 When patients present with symptoms of dysphagia or odynophagia, the esophagus should also be evaluated to rule out esophageal candidiasis. Azole-resistant oropharyngeal or esophageal candidiasis can be treated with fluconazole in a very high dosage (800 mg per day) or amphotericin B (Abelcet, Amphotec, Fungizone).
Hairy leukoplakia is a newly recognized, coarsely textured lesion of the oral cavity, unique to HIV-positive persons. It is a white lesion that forms most often on the lateral borders of the tongue. The lesion is raised, cannot be scraped off and has a hairy appearance. It resembles the hyperplastic form of candidiasis that is refractory to antifungal therapy. The lesion often indicates progression to full-spectrum AIDS.21 Epstein-Barr virus has been suggested as the causative agent. Hairy leukoplakia is usually asymptomatic and rarely requires treatment. It can be treated with zidovudine (Retrovir) or high doses of acyclovir (800 mg four times per day).22
Herpes simplex infections occur at a higher frequency in the HIV-positive population than in the general population.7 Of the two subtypes, HSV-1 and HSV-2, the former is far more commonly the causative agent of lesions in the oral cavity. Herpes labialis is the most common presentation of this infection. In HIV-infected patients, however, these lesions are larger and more numerous, recur more frequently and last longer than such lesions in HIV-negative patients. The lesions appear as ulcerations with raised borders (Figure 7) and are painful and tender to touch. They occur on heavily keratinized mucosal surfaces.7

Tests of the borders of the ulcer using Tzanck preparation, or viral cultures, help in confirming the diagnosis. Treatment of significant herpetic lesions in HIV-positive persons consists of acyclovir (or a similar antiviral agent) in a dosage of 200 mg five times a day. This treatment is effective only if started early in the course of the lesion. Mild to moderate oral herpetic lesions should be treated with oral acyclovir. In severely immunocompromised patients with frequent recurrence of oral herpetic lesions, prophylaxis with acyclovir is indicated.7 Foscarnet can be used in cases of acyclovir-resistant oral herpetic lesions.
HIV-infected persons may present with a wide range of periodontal diseases, from marginal inflammation (HIV gingivitis) to localized acute necrotizing ulcerative gingivitis and from localized periodontitis to necrotizing stomatitis. Patients with HIV gingivitis present with a bright erythematous line along the gingival margin and complain of spontaneous bleeding. In acute necrotizing ulcerative gingivitis, the gingiva appear erythematous, with ulcerations of the papillae that become tender and bleed when teeth are brushed. Rapid bone and soft tissue loss and loosening teeth are characteristic of HIV periodontitis. This group of patients complains of “deep” pain, and the condition can rapidly progress to large areas of necrotizing stomatitis.18
These patients should be referred to an oral surgeon for debridement, scaling and curettage of the involved areas. This treatment is followed by administration of metronidazole (Flagyl), in a dosage of 250 mg four times a day for five to six days, irrigation with povidone iodine and daily mouth rinsing with chlorhexidine gluconate (Peridex). Because it may potentiate peripheral neuropathy, metronidazole should not be given to patients taking didanosine (ddI; Videx) or zalcitabine (ddC; Hivid). In these patients, clindamycin (Cleocin), one 300-mg tablet three times daily, or amoxicillin, 250 mg three times daily, is prescribed.18
Some oral cavity neoplasms occur at a higher frequency in persons with AIDS. These include Kaposi's sarcoma, non-Hodgkin's lymphoma and squamous cell carcinoma.7,18 Kaposi's sarcoma is by far the most common oral neoplasm in AIDS patients. It is more common among homosexual and bisexual males with AIDS than in persons who contracted the HIV virus from any other source. Kaposi's sarcoma in patients under 60 years of age almost always indicates AIDS and fulfills the Centers for Disease Control and Prevention's requirement for the definition of AIDS.
The palate serves as the site for 95 percent of these oral lesions, while any other mucosal surface of the mouth can also be a site.7,23 In the early stages, the lesions are macular, dark or erythematous, maturing into more raised and lobulated mucosa. The lesions can ulcerate but rarely bleed or become tender. Kaposi's sarcoma is usually slow to develop but, in some reported cases, the lesions rapidly disseminate to involve the thoracic and abdominal viscera.23 Symptoms include increasing pain, odynophagia, dysphagia and difficulty in mastication. Therapy for patients with oral Kaposi's sarcoma ranges from no intervention for asymptomatic lesions to radiation, surgical removal and chemotherapy in patients with symptomatic lesions.23
Non-Hodgkin's lymphoma, in contrast to Kaposi's sarcoma, occurs most commonly in intravenous drug abusers with AIDS. After Kaposi's sarcoma, this is the most common neoplasm in patients with AIDS. The lesions of non-Hodgkin's lymphoma are red and exophytic, and commonly involve the alveolar ridge, the gingiva and the palate. The disease can also present as a rapidly enlarging neck mass. Most lesions are of large B-cell origin and originate extranodally. Non-Hodgkin's lymphoma can be diagnosed by tissue biopsy. The diagnosis carries a poor prognosis. Treatment varies from chemotherapy to radiotherapy or surgical excision, according to the site and extent of involvement.7,24,25
Squamous cell carcinoma most commonly involves the tongue and occurs with increased frequency in patients with AIDS compared with an age-matched control group. Patients present with a firm mass in the oral cavity (Figure 8), with or without pain. Diagnosis is confirmed by tissue biopsy. Treatment of such lesions depends on the overall condition of the patient and the stage of the disease. Patients may benefit from surgical resection and neck dissection since they do not tolerate high-dose radiation therapy well.7,18

Neck Manifestations
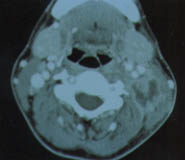
One of the earliest signs of HIV infection is persistent generalized lymphadenopathy, also known as HIV lymphadenopathy. This entity is defined as unexplained generalized lymphadenopathy involving two or more extrainguinal sites and lasting more than three months. The axilla is the most common site of lymphadenopathy, but head and neck sites are also very common (Figure 9). Patients often have no symptom other than neck swelling. Tissue sampling should be performed when malignancy is suspected.26 Indications for biopsy include recent weight loss, and lymph nodes that rapidly increase in size, and are firm or nonmobile.

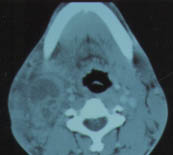
A number of opportunistic and nonopportunistic infections involving the neck present as cervical lymphadenopathy or an enlarging neck mass (Figures 10 and 11). The incidence of Mycobacterium tuberculosis infection has increased in HIV-positive patients, and 30 to 50 percent of these infections have extrapulmonary involvement. Of extrapulmonary sites, the cervical lymph nodes and the bone marrow are most commonly involved.26 Lymph nodes are firm and nontender.27 Purified protein derivative (PPD) tests, along with skin anergy testing, is indicated in cases in which tuberculosis is suspected. In HIV-positive patients, any skin reaction 5 mm or more in diameter is considered a positive result.28 If no response is noted on the skin anergy test, other modes of diagnosis, such as fine-needle aspiration or tissue biopsy, are indicated. Definitive diagnosis is made by culturing the organism.27,29 It is important to rule out pulmonary and systemic involvement after diagnosing cervical tuberculous lymphadenitis. Treatment consists of long-term, multiple antibiotic therapy for both pulmonary and extrapulmonary tuberculosis.27

Mycobacterium avium complex is the most common type of mycobacterial infection among HIV-positive patients (Figure 12). The disseminated form of the disease occurs in approximately 10 to 20 percent of patients with end-stage AIDS. This organism can be present in cervical lymph nodes, as well as other sites of dissemination, but it commonly appears in blood.30 M. avium complex is an acid-fast bacillus that can be located within foamy macrophages using Fite's method. Blood culture remains the unequivocal method of diagnosing disseminated M. avium complex infection.
As with tuberculosis, systemic involvement should be ruled out when M. avium complex has been identified in cervical lymph nodes. A triple antibiotic regimen of rifabutin (Mycobutin), in a dosage of 300 mg per day, plus ethambutol (Myambutol), in a dosage of 15 mg per kg per day, and clarithromycin, in a dosage of 500 mg twice a day, is well tolerated.30 Prophylaxis against disseminated infection with M. avium complex can be achieved with weekly azithromycin, clarithromycin or rifabutin in nonresistant paients.31 In cases of problematic drug interactions between rifabutin and HIV protease inhibitors, two-drug therapy with ethambutol and clarithromycin is acceptable.
A neck mass in an HIV-infected person can also be the presenting form of fungal infection, including cryptococcosis, histoplasmosis and coccidioidomycosis, for which the incidence is determined by geographic distribution of the organism. Cryptococcal meningitis is a more common presenting manifestation in HIV-infected patients.32
Pulmonary histoplasmosis and coccidioidomycosis are increasing in frequency along with the increase in incidence of HIV-positive patients in their endemic areas.
Parotid gland involvement is common in patients with HIV and can result from a wide range of pathologic conditions. Lymphoepithelial cyst of the parotid gland (Figure 13) is unique to HIV-positive patients. Often these patients have bilateral progressive swelling and tenderness at the angle of the mandible or upper neck. Tissue biopsy can be used as an adjunct to CT scan and fine-needle aspiration for diagnosis.

The pathogenesis of these true cysts remains unclear. They have a very benign course but at times grow fairly large. Repeated needle aspirations may be required to decompress the cysts. Tetracycline sclerosis offers an alternative to parotidectomy.26