
Am Fam Physician. 1998;58(1):118-124
Lisfranc joint injuries are rare, complex and often misdiagnosed. Typical signs and symptoms include pain, swelling and the inability to bear weight. Clinically, these injuries vary from mild sprains to fracture-dislocations. On physical examination, swelling is found primarily over the midfoot region. Pain is elicited with palpation along the tarsometatarsal articulations, and force applied to this area may elicit medial or lateral pain. Radiographs showing diastasis of the normal architecture confirm the presence of a severe sprain and possible dislocation. Negative standard and weight-bearing radiographs do not rule out a mild (grade I) or moderate (grade II) sprain. Reevaluation may be necessary if pain and swelling continue for 10 days after the injury. Proper treatment of a mild to moderate Lisfranc injury improves the chance of successful healing and reduces the likelihood of complications. Patients with fractures and fracture-dislocations should be referred for surgical management.
The Lisfranc joint, or tarsometatarsal articulation of the foot, is named for Jacques Lisfranc (1790–1847), a field surgeon in Napoleon's army. Lisfranc described an amputation performed through this joint because of gangrene that developed after an injury incurred when a soldier fell off a horse with his foot caught in the stirrup.1,2 The incidence of Lisfranc joint fracture–dislocations is one case per 55,000 persons each year.2,3 Thus, these injuries account for fewer than 1 percent of all fractures.2,3 As many as 20 percent of Lisfranc joint injuries are missed on initial anteroposterior and oblique radiographs.2–4
Lisfranc joint fracture–dislocations and sprains can be caused by high-energy forces in motor vehicle crashes, industrial accidents and falls from high places.1–3 Occasionally, these injuries result from a less stressful mechanism, such as a twisting fall. Since Lisfranc joint fracture–dislocations and sprains carry a high risk of chronic secondary disability,2 physicians should maintain a high index of suspicion for these injuries in patients with foot injuries characterized by marked swelling, tarsometatarsal joint tenderness and the inability to bear weight.
Illustrative Case
A 20-year-old man had an accident in which he was thrown from a sled. His body weight fell on his left foot, which was folded beneath him. On the day of the injury, his foot was examined in a hospital emergency department. Standard anteroposterior and lateral radiographs revealed no fracture. The foot was placed in slight plantar flexion and immobilized with a soft cast.
After three days, the patient was reevaluated at a student health clinic. His left foot remained edematous, and ecchymosis was noted laterally. Weight-bearing was intolerable. The soft cast was removed, and an elastic wrap was applied.
Seven days after the injury, the patient was evaluated in the authors' sports medicine clinic. His foot still could not bear weight, and edema extended from the midtarsal area distally into the toes. Ecchymosis along the metatarsophalangeal joint line extended to the lateral calcaneus. Marked dorsal tenderness was noted over the second through fourth tarsometatarsal joints and in the second through fifth metatarsophalangeal region. Palpation elicited only minimal tenderness on the plantar surface, with the tenderness limited to the region of the second and third tarsometatarsal joints.
A pedal pulse was present, and the patient was able to perform dorsiflexion of all toes against resistance. In addition, his ankle showed physical findings of a grade I anterior talofibular ligament sprain.
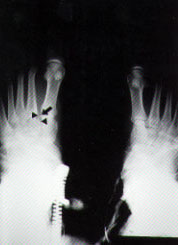
A review of the patient's initial lateral radiograph noted subtle dorsal displacement of the base of the second metatarsal (Figure 1). Weight-bearing anteroposterior radiographs were then obtained. These films showed a 3-mm separation of the first and second metatarsal bases and the presence of a bony fragment (fleck sign) in the Lisfranc joint space (Figures 2 and 3).


The patient was referred to an orthopedist. Treatment was open reduction and internal screw fixation, followed by a period of non–weight-bearing.
Definitions and Anatomy
To lessen ambiguity, some investigators5 have suggested that the term “Lisfranc joint complex” should be used to refer to tarsometatarsal articulations and that the term “Lisfranc joint” should be applied to medial articulation involving the first and second metatarsals with the medial (first) and middle (second) cuneiforms (Figure 4).
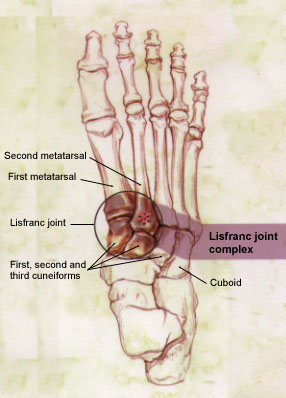
The Lisfranc ligament is a large band of plantar collagenous tissue that spans the articulation of the medial cuneiform and the second metatarsal base.4,6,7 While transverse ligaments connect the bases of the lateral four metatarsals, no transverse ligament exists between the first and second metatarsal bases. The joint capsule and dorsal ligaments form the only minimal support on the dorsal surface of the Lisfranc joint.3,6,7 The bony architecture of this joint, specifically the “keystone” wedging of the second metatarsal into the cuneiform, forms the focal point that supports the entire tarsometatarsal articulation.2 This anatomy establishes a “weak link” that, with stress, is prone to injury.
The anatomic complexity at the Lisfranc joint complex leads to multiple injury patterns.6 Sprains are the most common injury, with the midfoot sprain being the least severe injury.8 The severity of the sprain usually depends on the energy absorbed at the time of injury. Most tarsometatarsal ligament injuries are grade I (pain at the joint, with minimal swelling and no instability) or grade II (increased pain and swelling at the joint, with mild laxity but no instability). The more severe grade III sprain represents complete ligamentous disruption and may represent fracture-dislocation.9 Several further classifications of true fracture-dislocations are used,10 but they do not predict prognosis.4,6
Mechanisms of Injury
Lisfranc joint complex injury can occur as a result of direct or indirect trauma.3,11 Direct trauma occurs when an external force strikes the foot. With indirect trauma, force is transmitted to the stationary foot so that the weight of the body becomes a deforming force by torque, rotation or compression.2,5,7
Functionally, the foot is divided into three sections: the hindfoot, which absorbs shock during ambulation; the midfoot, which helps translate force and provides rotational stability of the foot; and the forefoot, which assists in the “toe-off ” phase of gait. The Lisfranc joint promotes energy dissipation by allowing force to be transferred between the midfoot and the forefoot.
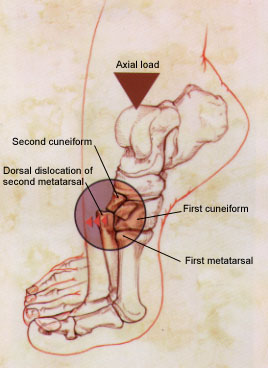
Because of its limited mobility, the Lisfranc joint provides a stable axis for rotation, and it is also the keystone for plantar flexion and dorsiflexion. The horizontal axis, about which plantar flexion and dorsiflexion occur, goes directly through the junction of the metaphysis and diaphysis of the base of the second metatarsal. Thus, with the lack of dorsal support and the immobility of the second metatarsal, placing the foot in extreme plantar flexion with an axial load can provide sufficient stress to cause dorsal displacement of the second metatarsal base (Figure 5).
Clinical Diagnosis
Presentation
Apart from a crush injury with marked swelling and radiographic changes, the Lisfranc joint injury can be difficult to diagnose. Gross subluxation or lateral deviation of the forefoot is rare.2 Swelling in the midfoot region and an inability to bear weight may be the only findings that suggest the diagnosis. Lisfranc joint injury should be suspected when the mechanism of injury is consistent with this traumatic injury and soft tissue edema or pain in the foot persists five or more days after the initial injury.2
Physical Examination
When Lisfranc joint complex injury is suspected, palpation of the foot should begin distally and continue proximally to each tarsometatarsal articulation. Tenderness along the tarsometatarsal joints supports the diagnosis of midfoot sprain with the potential for segmental instability.4
Pain can localize to the medial or lateral aspect of the foot at the tarsometatarsal region on direct palpation, or it can be produced by abduction and pronation of the forefoot while the hindfoot is held fixed.4 Another diagnostic clue is the patient's inability to bear weight while standing on tiptoe.3
The dorsalis pedis pulse and capillary refill should also be evaluated. The dorsalis pedis artery courses over the proximal head of the second metatarsal. Thus, it is susceptible to disruption in a severe dislocation.11
Radiographs
The initial radiographs of a suspected Lisfranc joint injury should include weight-bearing anteroposterior and lateral views, as well as a 30-degree oblique view.1,4,9,12 A weight-bearing radiograph is necessary, because a non–weight-bearing view may not reveal the injury. As an example, Figure 6 is a non–weight-bearing radiograph of the foot shown in Figure 2. Note that the patient's foot appears to be normal in the non–weight-bearing view. The diastasis between the base of the first and second metatarsals or the medial and middle cuneiforms should be evaluated carefully and compared with the unaffected side.

On the radiographs, dislocation of the tarsometatarsal joint is indicated by the following: (1) loss of in-line arrangement of the lateral margin of the first metatarsal base with the lateral edge of the medial (first) cuneiform; (2) loss of in-line arrangement of the medial margin of the second metatarsal base with the medial edge of the middle (second) cuneiform in the weight-bearing anteroposterior view1 (Figure 2) and (3) the presence of small avulsed fragments (fleck sign), which are further indications of ligamentous injury and probable joint disruption5 (Figure 3).
The lateral radiographic view of the foot may show a diagnostic “step-off,” which means that the dorsal surface of the proximal second metatarsal is higher than the dorsal surface of the middle cuneiform (Figure 1). On an oblique view, the medial edge of the fourth metatarsal base should be aligned with the medial edge of the cuboid.12 The radiographic evaluation may be negative in the patient who, in attempting ambulation, has caused the dislocation to spontaneously reduce.7
Some investigators13 have suggested that radiographic displacement or flattening of the longitudinal arch of the foot is associated with a poor prognosis. This finding may also correlate well with the patient's functional result, even after treatment.13 Other physicians caution that this radiographic abnormality pertains specifically to subtle injuries of the Lisfranc joint.14
Treatment
Early diagnosis of a Lisfranc joint injury is imperative for proper management and the prevention of a poor functional outcome.3 With a general knowledge of both conservative and operative treatment options, the primary care physician can decide whether to treat the injury nonoperatively or refer the patient to an orthopedist.
Nonoperative Treatment
If the clinical evaluation indicates the probability of a mild or moderate sprain and the radiograph shows no diastasis, immobilization is suggested. Treatment with a short-leg walking cast,6 a removable short-leg orthotic or a non–weight-bearing cast4 is continued for four to six weeks or until symptoms have resolved. The potential for disability following a Lisfranc joint injury justifies the use of a non–weight-bearing cast.
After the period of immobilization, ambulation and rehabilitation exercises should be progressive. If the symptoms persist up to two weeks after rehabilitation has begun, a repeat weight-bearing radiograph must be obtained to evaluate the joint articulation for instability5 and evidence of delayed separation (i.e., disarticulation worsened after weight-bearing).
Nonoperative vs. Operative Treatment
The treatment of Lisfranc joint complex fracture–dislocations remains controversial. Some investigators5,6,11 believe that nonoperative management of fractures and fracture-dislocations is ineffective, because the reduction and alignment that occur with casting are lost when soft tissue swelling decreases.
According to some investigators,3,6 a displacement of more than 2 mm requires open reduction and internal fixation to avoid a poor outcome,3,6 especially in athletes.4 Others13 report no correlation between the degree of diastasis and the eventual functional outcome. All studies indicate that timely diagnosis facilitates treatment and decreases long-term disability.
Operative Treatment
While some orthopedists3,4,6 prefer closed fixation with percutaneous K-wires (Kirshner wires), others5,11 report that this method does not hold anatomic reduction and fixation. An alternative method involves the use of open reduction and internal fixation with AO screw fixation (i.e., meets Arbeitsgemeinschaft für Osteosynthesefragen international standards). An open surgical field allows easier removal of fragments or soft tissue that may be hindering reduction of the dislocation.3,5,6
After open reduction and internal fixation, most orthopedists suggest that the foot be immobilized in a cast for eight to 12 weeks with minimal (toe-touch) weight-bearing.3,5,11 Noncasted, full weight-bearing usually is not allowed until the AO screw or similar device is removed at eight to 12 weeks.3,5 For three months after cast removal, the patient should wear a protective shoe with a well-molded orthotic.11
Complications
No consensus exists regarding the most effective treatment for Lisfranc joint injury when the diagnosis is delayed.3 Whether delayed treatment will prevent post-traumatic arthrosis and chronic pain is also controversial.3,13 The three factors that appear to be most important in predicting the occurrence of complications with Lisfranc joint injuries are the extent of local trauma, a delay in injury recognition and the degree of displacement.16 In general, procedures such as arthrodesis for post-traumatic arthritis should not be performed until at least one year after the initial injury.4,13,16