
Am Fam Physician. 1999;59(9):2475-2482
A more recent article on recurrent ischemic stroke is available.
This is Part I of a two-part article on stroke. Part II, “Management of Acute Ischemic Stroke,” will appear in the next issue.
See related patient information handout on preventing stroke, written by the authors of this article.
Clinical trials conducted during the past five years have yielded important results that have allowed us to refine our approach to stroke prevention. Treatment of isolated systolic hypertension prevents stroke and is generally well tolerated. New antiplatelet agents (clopidogrel and the combination of aspirin plus high-dose dipyridamole) have been shown to be effective in reducing vascular events in survivors of ischemic stroke, although aspirin remains the mainstay of antiplatelet therapy for stroke prevention. Several clinical trials support the benefit of lipid-lowering agents (“statins”) in reducing stroke. Warfarin reduces stroke for high-risk patients with atrial fibrillation. Carotid endarterectomy is highly beneficial in reducing stroke for symptomatic patients with severe carotid stenosis (greater than 70 percent), but the benefit is less for symptomatic patients with a moderate degree of stenosis (50 to 69 percent) and for patients with asymptomatic carotid disease of any severity.
During the past five years, important results in an unprecedented number of clinical trials have refined the approach to stroke prevention. This review highlights new developments in the prevention of ischemic stroke (Table 1). Stroke prevention is cost-effective and often cost-saving. Most strokes can now be prevented using proven interventions, but the challenge remains to apply these treatments effectively in clinical practice. Developments in the treatment of acute stroke will be reviewed in the second part of this article.
| Value of treating isolated systolic hypertension has been confirmed. |
| Cholesterol lowering with statins reduces stroke risk. |
| The new antiplatelet agent clopidogrel (Plavix) has been shown to be efficacious. |
| High-dose dipyridamole (Persantine) added to aspirin may be of value. |
| Risk stratification identifies high-risk patients with atrial fibrillation who benefit most from warfarin (Coumadin). |
| Asymptomatic carotid stenosis carries a relatively low risk of stroke and can be managed medically or surgically. |
Comparing the Impact of Therapies
A useful concept to assess the importance of a therapy is the “number-needed-to-treat.” This approach combines the relative risk reduction provided by a therapy with the absolute rate of occurrence of the event(s) of interest, to yield the actual number of patients that would need to be treated to prevent one event.1 Considering relative risk reduction without also considering the absolute rate can distort the importance of a therapy. For example, carotid endarterectomy for patients with severe carotid artery stenosis reduces the incidence of stroke by about 60 percent both for patients with ipsilateral strokes or transient ischemic attacks (TIAs) and for asymptomatic patients. However, because patients with ipsilateral symptoms have a far greater risk of stroke, the number-needed-to-treat with carotid endarterectomy to prevent one stroke is 10 times greater for asymptomatic patients than for those with recent ipsilateral symptoms.
To calculate the number-needed-to-treat, the absolute risk reduction by a therapy is divided into 100. For example, if the rate of stroke following a TIA averages 8 percent a year and aspirin therapy reduces this rate by 25 percent, the absolute rate reduction by aspirin is 2 percent per year (8 percent − 6 percent). The number of TIA patients that would need to be treated with aspirin for one year to prevent one stroke is 100 divided by 2, equaling 50.
Etiology and Risk Factor Management
Stroke is a heterogeneous syndrome in which multiple disorders can lead to occlusion or rupture of blood vessels supplying the brain (Figure 1). Optimal prevention depends on identifying the specific cause of threatened stroke. Severe cervical carotid artery stenosis is present in about 15 percent of patients with brain ischemia.2
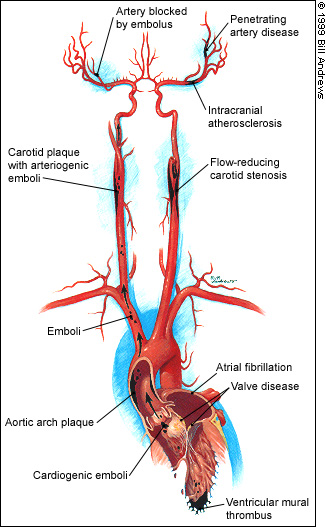
Nonstenotic atherosclerotic plaques can cause TIAs and stroke by acting as a source of arteriogenic emboli that migrate to obstruct distal vessels. Antiplatelet agents probably reduce stroke by inhibiting clot formation on thrombogenic surfaces of atherosclerotic plaques. Primary occlusive disease of the small penetrating arteries leads to small subcortical infarcts (often called “lacunes”), which are pathologically distinct from atherosclerosis. Cardiogenic emboli arise from valvular disease and from the cardiac chambers, with atrial fibrillation (AF) as the most common underlying cause. No specific cause can be identified in about 30 percent of patients (“cryptogenic stroke”); strokes with no identifiable cause are more frequent in younger stroke victims.2
Isolated Systolic Hypertension. Treatment of isolated systolic hypertension in the elderly reduces the risk of stroke and is generally well tolerated if carefully administered. A recent large, randomized trial showed that the benefits of treatment can be achieved with dihydropyridine calcium channel blockers and angiotensin-converting enzyme inhibitors.3 For those with a systolic blood pressure greater than 160 mm Hg, the number-needed-to-treat for one year to prevent one stroke is about 120. Treatment also reduces the incidence of congestive heart failure and other cardiovascular events.3
Cholesterol Reduction With Statin Drugs. Although large observational studies have failed to implicate increased cholesterol levels as an independent risk factor for stroke,4 clinical trials testing cholesterol reduction with statin drugs (3-hydroxy-3-methylglutaryl co-enzyme A [HMGCoA] reductase inhibitors) in persons with coronary artery disease or coronary risk factors consistently demonstrate a reduction in the rate of stroke.5 Recent meta-analyses of clinical trials using HMGCoA reductase inhibitors in patients with coronary artery disease showed a risk reduction in fatal and nonfatal stroke of 25 percent.5,6 At present, the value of cholesterol reduction with statins to prevent stroke has not been established specifically by clinical trials for patients with threatened stroke. Nonetheless, the use of statins in patients with cerebral ischemia to prevent myocardial infarction and vascular death is often clinically indicated.
Homocysteine. Elevations of serum total homocysteine levels have been correlated with risk for myocardial infarction and ischemic stroke, especially in middle-aged persons.7 Because small doses of folate correct the abnormality, there is considerable interest in this easily treatable potential risk factor for stroke. Until results of ongoing clinical trials are available to define levels requiring treatment and clinical response, we reserve homocysteine screening for use in patients with evidence of premature atherosclerosis in the absence of major atherosclerosis risk factors.
Antiplatelet Therapies for Cerebrovascular Disease
Aspirin and ticlopidine (Ticlid) are widely recognized as being effective for prevention of recurrent stroke in patients with TIA or ischemic stroke.8 Two additional antiplatelet therapies for stroke prevention have recently emerged: clopidogrel (Plavix) and high-dose dipyridamole (Persantine). Other new anti-platelet agents, such as the oral glycoprotein-IIb/IIIa inhibitors triflusal and indobufen, have not yet been adequately tested in patients with threatened stroke because of cerebrovascular disease.
Aspirin. Aspirin reduces the incidence of stroke by about 25 percent (the number of typical TIA or minor ischemic stroke survivors that need to be treated with aspirin for one year to prevent one stroke is about 50).8 Aspirin dosages between 50 and 1,300 mg per day have been shown to be effective for stroke prevention. The optimal dosage of aspirin to prevent stroke remains controversial, and both extremes of this range have been advocated. In the absence of convincing evidence favoring a specific dosage, most clinicians prescribe 325 mg per day. No patient subgroups have been defined for whom aspirin offers more or less protection (i.e., by gender or age).8
The preliminary report of a recently completed randomized trial comparing different dosages of aspirin in patients following carotid surgery indicated a statistically significant difference favoring the lower dosages (81 to 325 mg per day) when the event constellation of stroke, myocardial infarction and death was considered.9 Although the relevance of these findings to other situations is open to question, it lends support for the use of 325 mg per day pending additional trials. The U.S. Food and Drug Administration recently recommended that aspirin dosages between 50 and 325 mg per day be used for stroke prevention. The monthly cost of aspirin in a dosage of 325 mg per day is about $1.
Ticlopidine. Ticlopidine is significantly more effective than aspirin for prevention of stroke in patients with TIA or minor ischemic stroke.10 However, the magnitude of difference between ticlopidine and aspirin therapy appears to be relatively small: the number-needed-to-treat with ticlopidine instead of aspirin for one year to prevent one stroke is about 80.
Monitoring of the white blood cell count is required every two weeks during the first three months of therapy with ticlopidine to detect leukopenia, which occurs in 1 to 2 percent of recipients; skin rash and diarrhea preclude continued use of ticlopidine in about 15 percent of patients.10 Because of these potential side effects, most clinicians reserve ticlopidine for use in patients who experience cerebral ischemia while they are taking aspirin or for aspirin-intolerant patients. The monthly cost of ticlopidine at the usual dosage of 250 mg twice daily is about $115.
Clopidogrel. Clopidogrel, a congener of ticlopidine, was compared to aspirin in an international mega-trial involving more than 19,000 participants with varying clinical manifestations of vascular disease.11 Of the subset of 6,431 patients with recent ischemic stroke, the small reduction in subsequent stroke attained by use of clopidogrel compared to aspirin was not statistically significant. When all participants in the trial were considered, a small but statistically significant decrease in the event constellation of stroke, myocardial infarction and vascular death was achieved by use of clopidogrel relative to aspirin (P = 0.04).11 The toxicity of clopidogrel in a dosage of 75 mg per day was comparable to that of aspirin in a dosage of 325 mg per day, with no increase in leukopenia. It is not clear whether clopidogrel offers important benefits over aspirin for most patients with recent cerebral ischemia who are able to take aspirin. The monthly cost of clopidogrel in a dosage of 75 mg per day is currently about $87.
Dipyridamole. Dipyridamole combined with aspirin was widely used in the early 1980s for stroke prevention, until critical analysis cast doubt on its efficacy. A recent large European randomized trial found high-dose dipyridamole (200 mg twice daily, in a sustained-release preparation) plus aspirin (25 mg twice daily) to be superior to aspirin alone, with a 21 percent risk reduction relative to aspirin (P = 0.006).12 The number-needed-to-treat with dipyridamole plus aspirin compared to aspirin alone for one year to prevent one stroke is about 80. Side effects of high-dose dipyridamole included headache and required discontinuation of the drug in 6 percent of participants. At present, the role of high-dose dipyridamole with aspirin for prevention of stroke in patients with cerebrovascular disease remains controversial. The sustained-release preparation is not currently available in the United States. The monthly cost of dipyridamide in a dosage of 200 mg twice daily ranges from about $27 for generic to $156 for a brand-name product.
Based on different mechanisms of platelet inhibition, the combination of aspirin with other antiplatelet agents could theoretically enhance stroke prevention. Except for the combination of aspirin with dipyridamole, the efficacy and safety of combinations have not been established by clinical trials for patients with cerebrovascular disease. Thus, their routine use cannot be recommended at present.
With four antiplatelet agents proved to prevent stroke in patients with cerebrovascular disease, optimal antiplatelet therapy has become a subject of controversy. Each of the four agents has been advocated for use as first-line antiplatelet therapy to prevent stroke. Experts disagree about the strength of existing evidence and the clinical importance of therapy-related differences in outcome. The relative efficacies of these four agents, based on indirect comparisons, are estimated in Table 2. At present, we prescribe aspirin as first-line antiplatelet therapy, reserving clopidogrel for “aspirin failures” or aspirin-intolerant patients. More data are needed about the value of high-dose dipyridamole plus aspirin and other combinations.
Warfarin. Available antiplatelet agents offer only partial protection against strokes (i.e., 25 to 40 percent risk reduction), and more efficacious antithrombotic agents would be useful. However, anticoagulation with warfarin (Coumadin) has not been established as beneficial for patients with TIA or ischemic stroke caused by common cerebrovascular diseases. In contrast, warfarin is highly efficacious for prevention of stroke in patients with cardioembolic causes of brain ischemia. A multi-center European randomized trial comparing anticoagulation (target International Normalized Ratio [INR] range: 3 to 4.5; mean achieved INR: about 3) to aspirin was stopped because of an intolerably high rate of brain hemorrhage in those assigned anticoagulation.13 A large ongoing trial sponsored by the National Institutes of Health is testing lower INRs (target range: 1.4 to 2.8) and has entered over 2,000 participants, with results expected next year.
Until further data are available regarding the efficacy and safety of anticoagulation for use in patients with cerebrovascular disease, warfarin should not be routinely prescribed in patients without AF. Some clinicians advocate the use of warfarin for patients with inoperable symptomatic carotid stenosis, intracranial atherosclerotic stenosis or “anti-platelet failures.” Although these approaches are within the range of reasonable management, scientifically sound evidence favoring them is lacking.
Atrial Fibrillation
Clinical trials continue to demonstrate important benefits of warfarin (target INR: 2 to 3) for primary and secondary stroke prevention in high-risk patients with nonvalvular AF.14,15 Adjusted-dose warfarin therapy reduces the risk of stroke in patients with AF by about two thirds.16 Aspirin therapy for preventing stroke in AF patients reduces strokes by about 20 percent.17,18
Patients with nonvalvular AF are clinically heterogeneous, and the rate of stroke varies widely among persons with AF. Many AF patients have a low rate of stroke while taking aspirin or if untreated, and anticoagulation of low-risk AF patients provides only small reductions in the absolute rates of stroke. Risk stratification identifies AF high-risk patients who benefit most from anticoagulation (Table 3).19,20
| Stratification | AFI/ ACCP scheme | SPAF III scheme* | ||
|---|---|---|---|---|
| Clinical features | Approximate stroke rate | Clinical features | Approximate stroke rate | |
| High risk | History of hypertension Diabetes Previous stroke or transient ischemic attacks† Coronary artery disease Congestive heart failure | 6 % per year | Systolic blood pressure greater than 160 mm Hg Left ventricular dysfunction‡ Previous stroke or transient ischemic attack Women older than 75 years | 6 % per year |
| Moderate risk | 65 years or older | 2 % per year§ | History of hypertension | 3 % per year |
| No high-risk features | ||||
| Low risk | No high- or moderate-risk features | 1 % per year | No high- or moderate-risk features | 1 % per year |
The number of high-risk patients with AF who must be treated with warfarin instead of aspirin for one year to prevent one stroke is about 25, compared to 200 for low-risk patients with AF. The decision to treat patients with AF who are believed to have a moderate risk of stroke with warfarin (estimated number-needed-to-treat with warfarin instead of aspirin for one year to prevent one stroke is 50 to 75) should include careful consideration of individual bleeding risks and patient preferences.21
Carotid Artery Stenosis
Carotid endarterectomy reduces stroke for selected patients with cervical carotid atherosclerotic stenosis (Table 4). Based on consistent results of randomized clinical trials, carotid endarterectomy offers important benefits for patients with high-grade (70 percent or more) cervical carotid stenosis who also have ipsilateral focal ischemic events (i.e., symptomatic carotid stenosis).22,23 Symptomatic patients with mild stenosis (less than 50 percent) do not benefit from surgery.24 Patients with moderate (50 to 69 percent) symptomatic stenosis have intermediate benefit from endarterectomy (the number-needed-to-treat with endarterectomy to prevent one stroke during two years is about 20), supporting either surgical or medical management (Figure 2).22,25
| For symptomatic stenosis: | |
| Important benefit for high-grade (≥ 70 percent) stenosis; surgery recommended for most patients | |
| Modest benefit for moderate (50 to 69 percent) stenosis; surgery recommended for selected patients | |
| No substantial benefit over medical management for mild (<50 percent) stenosis* | |
| Reduces stroke in asymptomatic carotid stenosis, but magnitude of benefit is small in unselected patients | |
| Role of carotid angioplasty/stenting now undergoing evaluation in clinical trials | |
Patients with asymptomatic carotid stenosis have a relatively low rate of ipsilateral stroke (about 2 percent per year).26,27 Although carotid endarterectomy reduces the risk of ipsilateral ischemic stroke for patients with asymptomatic carotid stenosis by about 60 percent,26 the magnitude of this reduction is much smaller than for patients with symptomatic stenosis (Figure 3).22,25,27 It is not clear at present whether asymptomatic patients with very severe (greater than 80 percent) stenosis are a higher risk group who would benefit from endarterectomy (a European clinical trial addressing this issue is under way). Hence, routine use of surgery in patients with asymptomatic carotid stenosis is controversial, and both surgery and medical options should be discussed with these patients. A low perioperative complication rate is crucial if benefit from endarterectomy is to accrue to asymptomatic patients. Medical management of carotid stenosis includes the following measures:
Controlling risk factors such as hypertension and smoking.
Educating patients about TIA symptoms.
Identifying and treating existing coronary artery disease.
Performing serial carotid sonograms seeking determination of progression of stenosis, although the accuracy and value are uncertain.
Antiplatelet therapy.
Therapy with HMGCoA reductase inhibitors (statins) if low-density lipoprotein cholesterol level is greater than 130 mg per dL (3.40 mmol per L).
The efficacy, safety and durability of angioplasty, with or without stenting, for management of cervical and intracranial artery stenosis are unclear at present and are currently being assessed in clinical trials.