
Am Fam Physician. 2000;61(11):3385-3386
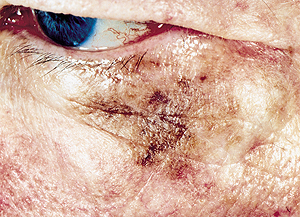
A 63-year-old man presented to the office for evaluation of a brown patch on his upper cheek and lower eyelid (see the accompanying photo). The patch had been present for more than 10 years and was gradually increasing in size. The patient had no visual complaints, adenopathy or other suspicious lesions. He has had a number of basal cell and squamous cell carcinomas excised over the past two decades. On physical examination, the patch demonstrated an irregular border and uneven pigmentation.
Question
Discussion
The answer is D: perform the largest incisional biopsy you can close without impairment of eyelid function. Lentigo maligna melanoma1 is an in-situ presentation of malignant melanoma. The usual presentation is on sun-exposed areas such as the face or bald scalp. The lesion typically has a very indolent course, which may span decades. While many spread superficially and remain in-situ, that is, confined to the epidermis and dermal-epidermal junction, others may become more invasive, and death from metastatic disease may occur. Older names, such as “Hutchinson's melanotic freckle,” obscure the fact that lentigo maligna melanoma is a potentially lethal condition that should be treated definitively as soon as it is identified and is not a condition to be followed clinically until it becomes obviously invasive.
Some suggest that one or more punch biopsies through “the most suspicious part” of a pigmented lesion are adequate for diagnosis. Unfortunately, one cannot always predict by visual inspection alone which part of a large lesion will be the most diagnostic or where the deepest invasion of a melanoma occurs. In the best-case scenario, melanoma will be recognized pathologically although the maximum depth of the tumor (which is the most important factor for prognosis) remains unknown, and the optimal margins for excision will be difficult to determine. In the worst-case scenario, the sample size will be too small (especially with small punches), the melanoma will be missed, and the patient and physician will be falsely reassured. The best way to biopsy a suspected melanoma is complete removal or, when not practical, obtaining the largest amount of tissue possible. Partially removing a melanoma does not make it more likely to metastasize.
Cryotherapy is often used for treatment of actinic keratoses, warts and seborrheic keratoses but is not recommended for destruction of melanocytic nevi or it may obscure an occult melanoma. Any lesion, even one presumed benign, that repeatedly recurs after proper cryotherapy should be biopsied. Topical hydroquinone may be effective therapy for melasma and, on some occasions, for treatment of post-inflammatory hyperpigmentation.