
Am Fam Physician. 2000;62(7):1513-1519
to the editor: A 61-year-old woman presented to the emergency department in respiratory distress. A chest radiograph was obtained and was clear. Although the patient had been previously diagnosed with chronic bronchitis and emphysema, she presented with an unusual worsening of her chronic respiratory symptoms over the previous six months, which was unexplained by clinical examination or chest film. The admitting diagnosis was straightforward asthma and chronic bronchitis exacerbation. Her mental status remained intact throughout the course of her hospitalization.
Over the subsequent three weeks, despite moderate- to high-dose steroids, frequent bronchodilator treatments and antibiotics, the patient's condition deteriorated to the point that she required admission to the intensive care unit.
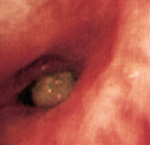
On admission, a computed tomographic (CT) scan of the chest was obtained to search for another etiology of her exacerbated respiratory distress. CT results revealed a soft tissue density in the right lower lobe bronchus (Figure 1). On subsequent fiberoptic bronchoscopy, a mucoid impaction was identified in the right lower lobe bronchus with surrounding erythema and edema (Figure 2). On removal of the plug, the patient's acute and subacute symptoms subsided immediately.
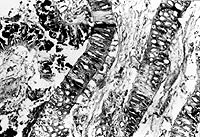
The pathology specimen (Figure 3) consisted of green, soft, amorphous material embedded in mucin, measuring 1.5 × 0.5 × 0.3 cm in aggregate. The histologic examination revealed strips of plant tissue with prominent thick cell walls that were admixed with bacterial colonies, inflammatory debris, mucin and respiratory epithelial cells.
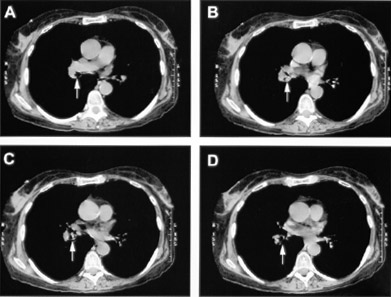
The diagnosis of foreign-body aspiration with secondary mucoid impaction in healthy adults is subtle. Here, despite the localized unilateral position of the impaction, no roentgenographic signs such as volume loss or opacities were evident, and the clinical findings were bilateral.
Foreign-body aspiration is commonly considered in children who have persistent or recurrent wheezing and pulmonary infection,1,2 and in adults who have a history of altered mental status. Although there are a number of reports documenting foreign-body aspiration in healthy adults,3,4 this possibility is often overlooked. Ironically, metered-dose inhalers (MDIs) are often implicated in foreign-body aspiration.5 If the mouth portion of the MDI is not capped, foreign objects may accidentally enter the MDI; subsequently, foreign-body aspiration may occur when the MDI is used. Furthermore, normal protective mechanisms (e.g., coughing) deteriorate as persons age,4 making the diagnosis of foreign-body aspiration more likely.
This diagnosis is challenging because the presentation and the subsequent course are often atypical. Patients present with nonspecific symptoms such as wheezing, cough with sputum3 and a normal chest film. As few as 6 to 8 percent of foreign-body aspirations are reported to result in abnormal chest films.6 Furthermore, one study1 reported that symptoms of foreign-body aspiration often respond, at least partially, to standard asthma therapy: seven out of 10 patients obtained relief in the uninvolved lung, while two out of 10 patients obtained relief in both lungs following standard asthma therapy.
The initial event of this patient's illness was inhalation of plant material that lodged in the right lower lobe bronchus. With time, local inflammation and bronchial secretions resulted in the foreign body becoming adherent and coated with mucus, which desiccated in situ. This inflammatory process continued, and the patient remained symptomatic until the impaction was diagnosed and the foreign-body was removed. This case illustrates that foreign-body aspiration must be considered as one of several possible etiologies in patients presenting with respiratory distress.