
Am Fam Physician. 2001;63(11):2211-2218
See patient information handout on complications of scuba diving, written by the author of this article.
Recreational scuba diving has become a popular sport in the United States, with almost 9 million certified divers. When severe diving injury occurs, the nervous system is frequently involved. In dive-related barotrauma, compressed or expanding gas within the ears, sinuses and lungs causes various forms of neurologic injury. Otic barotrauma often induces pain, vertigo and hearing loss. In pulmonary barotrauma of ascent, lung damage can precipitate arterial gas embolism, causing blockage of cerebral blood vessels and alterations of consciousness, seizures and focal neurologic deficits. In patients with decompression sickness, the vestibular system, spinal cord and brain are affected by the formation of nitrogen bubbles. Common signs and symptoms include vertigo, thoracic myelopathy with leg weakness, confusion, headache and hemiparesis. Other diving-related neurologic complications include headache and oxygen toxicity.
Recreational scuba diving, which is defined as pleasure diving without mandatory decompression to a maximum depth of 130 ft, has become a popular activity in the past 20 years. In the United States alone, there are almost 9 million certified divers.1 Although divers are concentrated along coastal regions, many others dive in inland lakes, streams, quarries and reservoirs, or fly to distant dive sites. Physicians practicing almost anywhere in the United States may see a patient with a dive-related injury or complaint.
In general, severe injury and death are uncommon in recreational diving accidents.1–5 The Divers Alert Network1 reports an average rate of 90 fatalities per year since 1980. Each year, between 900 and 1,000 divers are treated with recompression therapy for severe dive-related complications. In many of these patients, one or more of the major symptoms are neurologic in origin. The nervous system is frequently involved in dive-related complications and fatalities.5 Physicians need to be aware of the broad spectrum of neurologic injuries that can occur during dive accidents to ensure early recognition, accurate diagnosis and appropriate therapy.
Dive-Related Barotrauma
During descent and ascent in the water, the diver is constantly exposed to alterations of ambient pressure. Barotrauma refers to tissue damage that occurs when a gas-filled body space (e.g., lungs, middle ear) fails to equalize its internal pressure to accommodate changes in ambient pressure.2–4 The behavior of gasses at depth is governed by Boyle's law: the volume of a gas varies inversely with pressure.6 During descent, as ambient pressure increases, the volume of gas-filled spaces decreases unless internal pressure is equalized. If the pressure is not equalized by a larger volume of gas, the space will be filled by tissue engorged with fluid and blood. This process underlies the common “squeezes” of descent that affect the middle ear, external auditory canal, mask, sinuses and teeth.
OTIC AND SINUS BAROTRAUMA
Barotrauma to the middle or inner ear can occur during the descent or ascent phases of the dive and may cause vertigo and other neurologic symptoms.2–5,7 Middle ear barotrauma of descent is the most common type of diving injury and may involve hemorrhage and rupture of the tympanic membrane. Symptoms include the acute onset of pain, vertigo and conductive hearing loss that lateralizes to the affected side during the Weber's test. In severe cases (usually during ascent), increased pressure in the middle ear can cause reversible weakness of the facial nerve and Bell's palsy (facial baroparesis).8
Vertigo can also be induced if barotrauma differentially affects the two vestibular organs (alternobaric vertigo). The vertigo resolves after pressure equalization occurs. Treatment of middle ear barotrauma involves decongestants (e.g., intranasal oxymetazoline, oral pseudoephedrine), antihistamines, analgesics and antibiotics (amoxicillin-clavulanate [Augmentin] in a dosage of 500/125 mg three times per day or clindamycin [Cleocin] in a dosage of 300 mg three times per day for 10 to 14 days) in patients with otorrhea and perforation.2,4,7
Inner ear barotrauma also can develop in patients with middle ear barotrauma.2–5,7 A pressure gradient between the perilymph of the inner ear and the middle ear cavity can occur, causing rupture of the labyrinthine windows (round and oval) and leakage of perilymph into the middle ear (i.e., fistula). Symptoms include the acute onset of vertigo, sensorineural hearing loss, tinnitus, nausea and emesis. The Weber's test will lateralize to the unaffected side in this group of patients. Reducing intracranial and perilymphatic pressures through bed rest, head elevation and with stool softeners can help. Surgical exploration may be necessary for repair of the fistula if conservative treatment is ineffective within five to 10 days (i.e., the symptoms persist or worsen).
PULMONARY BAROTRAUMA
Pulmonary barotrauma is the most severe form of barotrauma and occurs during ascent.2–4,9 In accordance with Boyle's law, as the ambient pressure is reduced during ascent, gas inside the lungs will expand in volume.6 If the expanding gas is not allowed to escape by exhalation, the alveoli and surrounding tissues will tear. The most common cause of pulmonary barotrauma among recreational divers is breath holding. Other causes are related to pulmonary obstructive diseases, such as asthma or bronchitis, which can lead to the trapping of gas. Several forms of pulmonary barotrauma can develop, including mediastinal emphysema, subcutaneous emphysema, pneumothorax and arterial gas embolism. Arterial gas embolism is the most dangerous form of pulmonary barotrauma and accounts for nearly one fourth of fatalities per year among recreational divers.3 In addition, it is the only form in which neurologic symptoms predominate over pulmonary symptoms.9
Arterial gas embolism develops when free air enters the pulmonary vasculature and is carried to the heart and arterial circulation.9,10 A large proportion of air bubbles can reach the brain, occlude blood vessels and cause stroke-like events. The most common signs and symptoms of arterial gas embolism are neurologic (Table 12,4,6,7), although pulmonary symptoms may also be present. In more than 80 percent of patients, symptoms develop within five minutes of reaching the surface, but they also can occur during ascent or after a longer surface interval.
| Sign or symptom | Percentage |
|---|---|
| Stupor or confusion | 24 |
| Coma without seizures | 22 |
| Coma with seizures | 18 |
| Unilateral motor deficits | 14 |
| Visual disturbances | 9 |
| Vertigo | 8 |
| Unilateral sensory deficits | 8 |
| Bilateral motor deficits | 8 |
| Collapse | 4 |
Almost two thirds of patients with arterial gas embolism have alterations of consciousness (i.e., coma or obtundation). Seizures, focal motor deficits, visual disturbances, vertigo and sensory changes are also common. Spinal cord lesions occur less frequently. Many patients show initial improvement within minutes to hours, secondary to partial clearance of air emboli. Magnetic resonance imaging (MRI) may demonstrate focal lesions in the brain after arterial gas embolism.10 Arterial gas embolism can mimic decompression sickness, and the presentation of the two syndromes may be clinically indistinguishable (Table 21–5,7–10).2,4,6 Arterial gas embolism and decompression sickness can develop simultaneously in some patients. In fact, the air emboli of arterial gas embolism may act as a nidus, or “seed,” to precipitate decompression sickness. Therefore, the two syndromes are often described and treated together using the more global term, decompression illness.4
| Disorder | Clinical features | Dive profile | Treatment |
|---|---|---|---|
| Middle ear barotrauma of descent | Acute pain, vertigo, hearing loss, rupture or hemorrhage of tympanic membrane | During descent usually, possible during ascent | Improved equalization techniques, oral and nasal decongestants; with otorrhea use antibiotics |
| Facial baroparesis | Ipsilateral facial paralysis, resolves within hours | During ascent | No treatment |
| Inner ear barotraumas | Acute vertigo, nausea, emesis, tinnitus, sensorineural hearing loss; often associated with middle ear barotrauma | During descent usually, possible during ascent | ENT evaluation, bed rest, head elevation, stool softeners; consider surgical exploration if symptoms persist |
| Arterial gas embolism | Stupor, confusion, coma, seizures, focal weakness, visual loss | Within five minutes of surfacing (> 80 percent) or during ascent; significant time-depth exposure not required | 100 percent oxygen, United States Navy Table 6 algorithm recompression, supportive care |
| Inner ear DCS | Acute vertigo, nausea, emesis, nystagmus, tinnitus, sensorineural hearing loss | Within 30 to 60 minutes of surfacing (> 50 percent), 90 percent by six hours; significant time-depth exposure required | Same as above |
| Cerebral DCS | Confusion, focal weakness, fatigue, visual loss, diplopia, speech dysfunction, gait abnormality, headache | Same as above | Same as above |
| Spinal cord DCS | Paresthesias/sensory loss in trunk and/or extremities, leg weakness, loss of bowel/bladder function | Same as above | Same as above |
| Headache (arterial gas embolism or DCS) | Severe generalized headache associated with alteration of consciousness and other signs | Usually develops within minutes of ascent, may persist without recompression treatment | Same as above; analgesics |
| Headache (migraine) | Pounding, throbbing pain; nausea, emesis, photophobia | Usually precipitated during pre-dive activities or at depth | Avoid precipitating stimuli, dive conservatively, consider prophylactic therapy |
| Oxygen toxicity | Focal seizures, visual constriction, nausea, emesis, vertigo, paresthesias, rare generalized seizures | Occurs at depth | Reduce depth and oxygen exposure, supportive care, seizure management; see arterial gas embolism treatment |
Oxygen reduces ischemia in affected tissues and accelerates the dissolution of air emboli. Seizures, arrhythmias, shock, hyperglycemia and pulmonary dysfunction should be treated, if present. Recompression therapy should be initiated immediately, using the United States Navy (USN) Table 6 algorithm.2–5,10,11 Recompression therapy reduces the size of air bubbles by increasing ambient pressure, expedites passage of emboli through the vasculature and re-establishes blood flow to ischemic tissues.
Decompression Sickness
Decompression sickness is caused by the release of inert gas bubbles (usually nitrogen) into the bloodstream and tissues after ambient pressure is reduced.2–5,10 At depth, the partial pressures of gasses in the breathing mixture increase in proportion to the ambient pressure, according to Dalton's law.6 Although oxygen is actively metabolized, nitrogen is inert and becomes dissolved in body tissues until saturation, proportional to the ambient pressure as defined by Henry's law.6 The propensity for the formation of nitrogen bubbles depends on the depth of the dive, the length of time at depth and the rate of ascent. If ambient pressure is released too quickly, the dissolved nitrogen gas that cannot remain in solution will form air bubbles within the blood, interstitial fluids and organs (Figure 1).
Decompression sickness is traditionally classified into type I and type II. In type I decompression sickness, symptoms are usually mild and may manifest as fatigue or malaise (i.e., constitutional decompression sickness) or may be more specific, involving the muscles, joints and skin.10 Type II decompression sickness is more severe and can affect the lungs, vestibular apparatus and the nervous system.
In inner ear and neurologic decompression sickness, the formation of bubbles affects the brain, spinal cord, cranial and peripheral nerves, and the neural vasculature. Nitrogen bubbles can injure neural tissues by mechanical disruption, compression, vascular stenosis or obstruction, and activation of inflammatory pathways (e.g., cytokines, complement).4,10 Cerebral decompression sickness (30 to 40 percent of cases) usually involves arterial circulation, while spinal cord decompression sickness (50 to 60 percent of cases) involves obstruction of venous drainage and the formation of bubbles within the cord parenchyma.12
The incidence of decompression sickness among recreational scuba divers is estimated to be one case per 5,000 to 10,000 dives.1 Diving within the limits of dive tables is no guarantee against decompression sickness, because more than 50 percent of cases of decompression sickness occur after no-decompression dives. In addition to the dive profile and rate of ascent, other factors may influence the risk of decompression sickness, including hypothermia, fatigue, increased age, dehydration, alcohol intake, female gender, obesity and patent foramen ovale.2–5,13
In type II neurologic decompression sickness, more than 50 percent of patients develop symptoms within one hour of ascent; within six hours, 90 percent of divers are symptomatic.1,4,14 Inner ear decompression sickness presents with acute vertigo, nausea, emesis, nystagmus and tinnitus. The pathophysiology remains unclear; one mechanism is bubble rupture of the intraosseous membranes in the semicircular canals. In many cases, inner ear decompression sickness is clinically indistinguishable from otic barotrauma, although the dive profile and timing of symptoms may help to clarify the diagnosis (Table 2).2–5,7,10
Neurologic decompression sickness can present with a wide spectrum of symptoms (Table 3). The most severe presentation is partial myelopathy referable to the thoracic spinal cord.10,15 Patients complain of paresthesias and sensory loss in the trunk and extremities, a tingling or constricting sensation around the thorax, ascending leg weakness ranging from mild to severe, pain in the lower back or pelvis and loss of bowel and/or bladder control. The neurologic examination will often reveal monoparesis or paraparesis, a sensory level and sphincter disturbances. However, neurologic examination also may be normal.
| Sign or symptom | Percentage |
|---|---|
| Numbness | 59 |
| Pain | 55 |
| Dizziness | 27 |
| Extreme fatigue | 25 |
| Headache | 24 |
| Weakness | 23 |
| Nausea | 14 |
| Gait abnormality | 12 |
| Hypoesthesia | 10 |
| Visual disturbance | 8 |
| Itching | 5 |
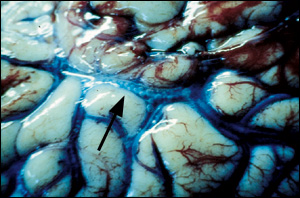
Pathologic features within the spinal cord include hemorrhagic infarctions, edema, bubble defects, axonal degeneration and demyelination (Figure 2).12,15 Cerebral decompression sickness can occur alone or in combination with spinal decompression sickness and manifests as an alteration of mentation or confusion, weakness, headache, gait disturbance, fatigue, diplopia or visual loss. The neurologic examination may show hemiparesis, dysphasia, gait ataxia, hemianopsia and other focal signs. Behavioral and cognitive aspects of cerebral decompression sickness may be persistent or slow to improve.10,16 The pathologic features are similar to those of spinal decompression sickness, although not as pronounced.10,17
The diagnosis of neurologic decompression sickness is clinical and should be suspected in any patient with a recent history of diving who has a consistent presentation. Neuroimaging studies may further clarify the diagnosis but should not delay treatment. MRI demonstrates high-signal lesions of the brain and spinal cord in 30 to 55 percent of cases (Figure 3), which suggests ischemia, edema and swelling. The lesions do not enhance with contrast. However, images on MRI are often normal.5,10,16
The initial management of neurologic decompression sickness is similar to that of arterial gas embolism and decompression illness, and requires transport to a recompression facility.2–5,10,16 If transport by helicopter is necessary, the patient should be flown at an altitude of less than 1,000 ft to minimize exacerbation of symptoms. The definitive treatment is recompression therapy using the USN Table 6 algorithm.11 USN Table 6 consists of initial recompression to 60 ft of salt water with 100 percent oxygen for 60 minutes. The patient is then decompressed to 30 ft of salt water for two additional periods each of breathing pure oxygen and air. Recompression therapy reduces the size of bubbles, allowing easier reabsorption and dissipation, and increases the nitrogen gradient to expedite off-gassing. The majority of recreational divers with neurologic decompression sickness have an excellent recovery after prompt recompression therapy.
The Divers Alert Network (DAN) at Duke University Medical Center, Durham, N.C., is available 24 hours a day to discuss arterial gas embolism or decompression sickness and provide divers a referral to the nearest recompression facility, if necessary. The emergency hotline number is 919-684-8111. For nonemergency medical questions, call DAN at 919-684-2948.
Headache
Headache is a common symptom in divers. There are numerous benign causes, including exacerbation of tension or migraine headaches, exposure to cold, mask or sinus barotrauma, sinusitis and a tight face mask. Migraines are not often precipitated by diving, but can be severe when they occur. If a migraine develops, the dive should be terminated because of the potential for nausea, emesis and alteration of consciousness. Dangerous causes of headache include cerebral decompression sickness, contamination of the breathing gas with carbon monoxide, arterial gas embolism, severe otic or sinus barotrauma with rupture, and oxygen toxicity.2–5,10 If headache occurs in a patient with potential arterial gas embolism or decompression sickness, it should be considered an emergency, because it suggests the presence of intracerebral bubbles. This type of headache usually develops within minutes of ascent. Immediate use of 100 percent oxygen and of recompression therapy is indicated.
Oxygen Toxicity
In the recreational diver, the most likely cause of oxygen toxicity is diving with oxygen enriched air (i.e., Nitrox). Nitrox is a breathing mixture that contains more than 21 percent oxygen (usually 32 to 36 percent), and allows extended bottom time. When diving with Nitrox, the diver is at risk of oxygen toxicity if the maximum oxygen depth limit and/or the oxygen time limit is exceeded. In general, the higher the oxygen content in the Nitrox mixture, the shallower the dive to minimize the potential for oxygen toxicity. Symptoms develop at depth without warning and consist of focal seizures (e.g., facial or lip twitching occurs in 50 to 60 percent of patients), vertigo, nausea and emesis, paresthesias, visual constriction and respiratory changes.18 Generalized seizures or syncope can also occur in 5 to 10 percent of patients. Although uncommon, generalized seizures at depth are often fatal, because divers may drown or arterial gas embolism may be precipitated during rescue to the surface.4 The cause of oxygen toxicity to the nervous system mainly involves oxygen-free radical formation, as well as reduction of the inhibitory neurotransmitter, gamma-aminobutyric acid. Treatment consists of reducing oxygen exposure and dive depth and, if necessary, managing seizures.