
Am Fam Physician. 2001;64(2):279-287
Osteoarthritis is one of the most prevalent and disabling chronic conditions affecting older adults and a significant public health problem among adults of working age. As the bulk of the U.S. population ages, the prevalence of osteoarthritis is expected to rise. Although the incidence of osteoarthritis increases with age, the condition is not a normal part of the aging process. More severe symptoms tend to occur in the radiographically more advanced stage of the disease; however, considerable discrepancy may exist between symptoms and the radiographic stage. Roentgenograms of involved joints may be useful in confirming the diagnosis of osteoarthritis, assessing the severity of the disease, reassuring the patient and excluding other pathologic conditions. The diagnosis of osteoarthritis is based primarily on the history and physical examination, but radiographic findings, including asymmetric joint space narrowing, subchondral sclerosis, osteophyte formation, subluxation and distribution patterns of osteoarthritic changes, can be helpful when the diagnosis is in question.
Worldwide, osteoarthritis is the most common form of arthritis.1 It is among the most prevalent and disabling chronic conditions in the United States.2 The prevalence increases with age, and by the age of 65, approximately 80 percent of the U.S. population is affected.3–5 The functional impairments secondary to osteoarthritis also occur more frequently in older adults. Pain and limitation of motion restrict the independence of older adults by impairing their performance of activities of daily living.6,7 As a result, dependence is especially common for ambulation, stair climbing and other lower-extremity functions.8
Costs directly attributable to osteoarthritis are considerable in the United States, with work loss accounting for more than one half of the estimated annual expense of $155 billion (in 1994 dollars).9 Another major expense is the number of joint arthroplasties performed in patients in the advanced stage of the disease.10–12
Etiology and Risk Factors
Although osteoarthritis is especially common in older adults, its pathology of asymmetric joint cartilage loss, subchondral sclerosis (increased bone density), marginal osteophytes and subchondral cysts is the same in younger and older adults.1 Primary osteoarthritis is the most common form and is usually seen in weight-bearing joints that have undergone abnormal stresses (e.g., from obesity or overuse).13–16 The precise etiology of osteoarthritis is unknown, but biochemical and biomechanical factors are likely to be important in the etiology and pathogenesis.1 Biomechanical factors associated with osteoarthritis include obesity, muscle weakness and neurologic dysfunction. In primary osteoarthritis, the common sites of involvement include the hands, hips, knees and feet13,17 (Figure 1). Secondary osteoarthritis is a complication of other arthropathies or secondary to trauma. Gout, rheumatoid arthritis and calcium pyrophosphate deposition disease are correlated with the onset of secondary osteoarthritis.
Clinical Manifestations
Osteoarthritis is primarily assessed through a history and physical examination. The cardinal symptom of osteoarthritis is pain that worsens during activity and improves with rest. Instability of joints is a common finding, especially of the knees and first carpometacarpal joints. Early morning stiffness is common and characteristically lasts one hour or more, depending on severity. Stiffness may occur following periods of inactivity. Musculoskeletal examination may reveal swelling, deformities, bony overgrowth (referred to as Heberden's nodes when involving the distal interphalangeal joints and Bouchard's nodes when involving the proximal interphalangeal joints of the hands), crepitus and limitation of motion. Muscle spasm, and tendon and capsular contractures also may be observed, depending on the site and duration of involvement.
Pain caused by osteoarthritis may develop in any part of the involved joint or tissue. Typically, pain progresses gradually over time and increases with weight bearing. A patient with primary osteoarthritis seldom has any attributable systemic symptoms (e.g., fatigue or generalized weakness). The progression of symptoms in patients with osteoarthritis is fairly consistent. Mild discomfort first occurs in a joint when it is in high use, but the pain is relieved by rest. Symptoms progress to constant pain on use of the affected joint and finally, with more advanced joint involvement, pain occurs at rest and at night. Generally, little tenderness occurs outside the joint, but pain can occur with extremes in range of motion. Limitation of motion is often prominent.
Cervical and lumbar pain may result from arthritis of the apophyseal joints, osteophyte formation, pressure on surrounding tissue and muscle spasm. Nerve root impingement causes radicular symptoms. Cervical and lumbar stenosis develop when facet joints hypertrophy, the disc degenerates and bulges, and the ligamentum flavum becomes lax and widens. The spinal canal narrows and compresses the cord. Posterior vertebral osteophytes may also contribute to cord compression. Patients may develop lumbar pain, extremity weakness, gait ataxia or abnormal neurologic findings. Pseudoclaudication is a characteristic feature of lumbar stenosis and is described as pain in the buttocks or thighs occurring with ambulation and relieved by rest. Hip pain is usually felt in the groin or the medial aspects of the thigh; however, it can be referred to the knee or buttocks and may be misdiagnosed as lumbar stenosis.
Radiographic Findings
The diagnosis of osteoarthritis is often suggested on physical examination. Plain film radiographs are usually adequate for initial radiographic evaluation to confirm the diagnosis or assess the severity of disease if surgical intervention is being considered. Two views of the involved joint should be obtained, with the possible exception of the sacroiliac joints and the pelvis. The two views should be obtained in orthogonal planes to one another (i.e., anteroposterior [AP] and lateral). Additional views of weight-bearing joints (knees, hips) may be necessary. Correlation of radiographic evidence of degenerative joint changes and symptoms described by patients vary by joint. Abnormalities detected in the knees correlate with pain in 85 percent of patients, the fingers and carpometacarpal joints in approximately 80 percent and the hips in 75 percent.6
The radiographic hallmarks of primary osteoarthritis include nonuniform joint space loss, osteophyte formation, cyst formation and subchondral sclerosis. The initial radiographs may not show all of the findings. At first, only minimal, nonuniform joint space narrowing may be present. The involved joint spaces have an asymmetric distribution. As the disease progresses, subluxations may occur and osteophytes may form. Subchondral cystic changes can occur. These cysts may or may not communicate with the joint space, can occur before cartilage loss and have a sclerotic border. Subchondral sclerosis or subchondral bone formation occurs as cartilage loss increases and appears as an area of increased density on the radiograph. In the advanced stage of the disease, a collapse of the joint may occur; however, ankylosis does not usually occur in patients with primary osteoarthritis.
| Condition | History | Physical | |
|---|---|---|---|
| Primary osteoarthritis | Gradual progression of pain Morning stiffness of one hour or more Pain increasing with weight bearing Night pain No systemic symptoms | Bony enlargement of joints: DIP, PIP, first carpometacarpal, hips, knees, feet Usually no wrist, elbow, ankle or involvement of MCP | |
| Bursitis/tendonitis | Pain increased with movement Pain worse at night No systemic symptoms Pain on some maneuvers, not others | No joint abnormality or swelling Certain passive maneuvers produce pain Pain on resisted active range of motion of affected muscles | |
| Mechanical intra-articular conditions | Recurrent joint swelling Joint locks Joint “gives way” Intermittent pain with pain-free intervals | Pain and limitation at certain points of flexion or extension Pain on combined rotation and extension of the knee | |
| Rheumatoid arthritis | Often insidious onset Morning stiffness of one hour or more Systemic symptoms Associated symptoms (e.g., Raynaud's syndrome, skin rash) | Involvement of MCP, wrist, elbows, ankles Synovial thickening Classic deformities: Swan neck Boutonniere Ulnar deviation Loss of range of motion of wrist, elbows | |
KNEE
When evaluating patients with osteoarthritis of the knee, AP and lateral radiographs allow an adequate evaluation of the medial and lateral joint spaces. To adequately assess the joint space, the AP view should be obtained with the patient in a standing position. The lateral view also allows evaluation of the patellofemoral joint; however, an additional view, known as the sunrise view, can offer even more information about this joint space.

Radiographic findings in patients with osteoarthritis include medial tibiofemoral and patellofemoral joint space narrowing, as well as subchondral new bone formation.18,19 Next, lateral subluxation of the tibia occurs, and osteophyte formation is most prominent medially. Lateral joint space narrowing can also occur but not as prominently as the medial narrowing (Figures 2a and 2c). Cartilage is lost, and subchondral bone formation occurs. Marked osteophyte formation also occurs (Figures 2b and 2d), and osteophytes are seen anteriorly and medially at the distal femur and proximal tibia, and posteriorly at the patella and the tibia.
HAND
The hand can be evaluated with AP and oblique views; however, more detail is evident with magnified views of the entire hand or of a specific joint. Magnification views are particularly helpful in evaluating the soft tissues and the fine detail of specific bone. The most commonly involved joints in the hand and wrist are the first carpometacarpal joints, the trapezionavicular joint and the proximal interphalangeal and distal interphalangeal joints. Joint space loss is nonuniform and asymmetric (Figure 3). Erosive changes are not seen in primary osteoarthritis. In cases where an underlying disease process (such as an inflammatory arthropathy) is present, secondary osteoarthritis can occur. Postmenopausal women may have a variant of osteoarthritis, known as erosive arthritis.20 Only erosive osteoarthritis has erosions and ankylosis. The distribution in the hands and the feet is similar to that of osteoarthritis.
HIPS AND PELVIS
AP views of the pelvis can be used to assess arthritic changes in the hips as well as the sacroiliac joints (Figure 4). Changes associated with the hip include superolateral joint space narrowing with subchondral sclerosis. The superolateral portion of the joint is the weight-bearing portion. Cystic changes can occur, and the femoral head can appear to be irregular.
The true synovial joint space of the sacroiliac joint occurs anteriorly and inferiorly. In osteoarthritis, bridging osteophytes develop and extend from the ilium to the sacrum. Sclerotic changes are also noted, but ankylosis or erosions do not usually develop as they do in spondyloarthropathies such as ankylosing spondylitis, psoriasis or Reiter's syndrome.
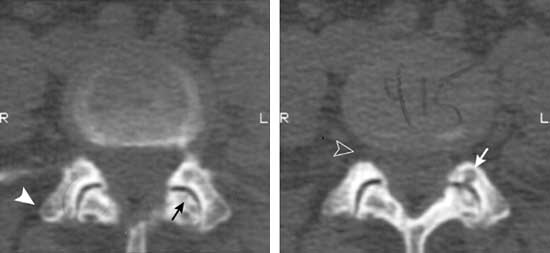
SPINE
Lateral and AP lumbar spine radiographs are adequate to allow identification of osteoarthritic changes in the apophyseal joints. Decreased joint space is noted between the superior and inferior facets. Sclerosis and cyst formation occur in osteoarthritis of the spine. Neural foraminal narrowing may result from the osteophyte formation. These changes can be seen on computed tomographic (CT) scans. Figure 5 illustrates neural foraminal narrowing caused by facet osteophyte formation. Similar changes are seen in the cervical spine. Primary osteoarthritic changes are not commonly seen in the thoracic spine. Osteoarthritis of the spine is often associated with degenerative joint disease.

FOOT
In the foot, AP and lateral radiographs are adequate to assess osteoarthritic changes, but oblique and magnified views may be helpful if a detailed view of a joint space is required. The most common joint involved is the first metatarsophalangeal joint. Again, subchondral sclerosis, osteophyte formation and cystic changes are common. Lateral subluxation of the great toe results in a hallux valgus deformity. Osteoarthritic changes elsewhere in the foot, such as the subtalar joint, are usually caused by altered mechanics from congenital or acquired abnormalities (e.g., pes planus, fusion of two bones) or are secondary to another underlying arthropathy (e.g., psoriasis, Reiter's syndrome).

Disease Progression
Follow-up radiographs are unnecessary in evaluating progression of the disease but can be helpful, especially if surgical intervention is planned or a fracture is suspected. Imaging beyond plain films is not warranted for routine follow-up; however, in the appropriate clinical situation, additional types of imaging may be useful. Nuclear medicine bone scans can show radiopharmaceutical localization but are nonspecific in areas of increased bone production. Tomography is only helpful if an occult fracture is suspected, but routine tomography is not indicated to monitor osteoarthritis.
While a CT scan is not indicated for an initial evaluation or as routine follow-up, it may be helpful in the evaluation of the lumbar spine to check facet hypertrophy in the management of low back pain and spinal stenosis. This evaluation can also be accomplished with magnetic resonance imaging (MRI) studies, although the osseous detail is better appreciated with CT scan. MRI also can be helpful in evaluating cartilage loss but often is unnecessary because plain films provide adequate information. MRI studies should not be routinely performed in diagnosing osteoarthritis unless additional pathology is suspected (e.g., post-traumatic injuries, malignancy, neural foraminal impingement, infectious process). Ultrasonography can be helpful in diagnosing cystic changes in the soft tissue about the joints but is not useful in the initial diagnosis of osteoarthritis.
Differential considerations are based, in part, on which joint is being examined. In general, the major differential diagnosis includes rheumatoid arthritis, psoriatic arthritis, calcium pyrophosphate deposition disease, ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (Table 2).20
| Condition | Bone density | Erosions | Cysts | Joint space loss | Distribution | Bone production |
|---|---|---|---|---|---|---|
| Osteoarthritis | Normal overall | No, unless erosive osteoarthritis | Yes, subchondral | Nonuniform | Unilateral and/or bilateral; asymmetric | Yes; osteophytes; subchondral sclerosis |
| Rheumatoid arthritis | Decreased | Yes | Yes, synovial | Uniform | Bilateral; symmetric | No |
| Psoriatic arthritis | Normal | Yes | No | Yes | Bilateral; asymmetric | Yes |
| CPPD | Normal | No | Yes | Uniform | Bilateral | Yes; osteophytes; chondrocalcinosis; subchondral |
| Ankylosing spondylitis | Early—normal Late—decreased | Yes | No | Yes | Bilateral; symmetric | Yes |
| DISH | Normal | No | No | No | Sporadic | Flowing osteophytes; ossification of tendon, ligaments |