
Am Fam Physician. 2001;64(3):455-459
Fingertip amputations are injuries commonly seen by family physicians. The classification of fingertip injuries corresponds with the normal anatomy of the tip of the digit. There are three zones of injury; the V-Y plasty technique is used to repair zone II injuries. The plane of the injury can be described as dorsal, transverse or volar. The dorsal and transverse planes lend themselves to the use of the V-Y plasty technique. In carefully selected injuries, the family physician can use this technique to repair the injured digit. The use of a single V-Y plasty has replaced the original technique that repaired the digit and restored the contour of the fingertip. Good cosmetic and functional results can be obtained. Complications may include flap sloughing, infection and sensory changes.
Fingertip amputation is a common injury.1 Multiple repair techniques have been described in the literature, including skin grafts, local or distant flap procedures, and partial toe transplantation. Many of these techniques are complex and can only be performed by specially trained physicians. The V-Y plasty repair is an easy technique to learn and can be valuable to the family physician. Although it is not a routine procedure, family physicians may choose to perform it in certain settings and circumstances.
The V-Y plasty technique is an island pedicle flap procedure. While most local flaps rotate into a wound from nearby tissues, bringing the blood supply with the intact portion of the flap, island pedicle flaps receive the blood supply from below, in the capillaries immediately beneath the dermis. This capillary supply must not be disrupted by undermining the tissue when creating an island pedicle flap.2
Classification of Fingertip Injuries
Many fingertip amputations can be classified consistent with the normal functional anatomy of the tip and perionychium.3 Injuries can be classified according to where the amputation has occurred or whether the injury primarily involves the pulp (soft tissue) or nail bed. These classification systems refer to the zone and the plane of injury3,4 (Figures 1 and 2).
An injury classified as zone I occurs distal to the bony structures of the digit and the distal phalanx is preserved. Most of the nail bed and the integrity of the matrix is intact, allowing for normal nail contours following healing. Treatment of zone I injuries is usually conservative, such as leaving the wound open for secondary healing.3 Meticulous wound care and conservative debridement of these injuries are essential. Wound healing is facilitated by the use of topical antibiotic ointments and by monitoring of the injury to avoid the development of excessive granulation tissue.
Injuries classified as zone II are located distal to the lunula of the nail bed and are complicated by the bony exposure of the distal phalanx. These injuries require local or distant pedicle flap reconstruction.3 The plane of zone II injuries helps determine what type of repair technique should be used.
Injuries classified as zone III involve the nail matrix and result in the loss of the entire nail bed. Most patients with injuries in zone III are not candidates for elaborate reconstruction. The most effective management of these injuries is amputation of the distal phalanx.
Amputation injuries are also classified as dorsal, transverse or volar, according to the plane of the amputation (Figure 2). The plane of the amputation and the condition of the tissue at the injury site help determine the best repair technique for these injuries. The V-Y plasty technique can be used to repair amputations with dorsal or transverse planes.4
In a recent article,5 researchers proposed a new classification system for fingertip injuries. This system classifies a fingertip injury into three areas: pulp, the nail and the bone, or PNB (pulp, nail, bone).5 This classification system may have merit but, because it has not been widely used, it requires further study to be useful for classification of fingertip injuries, including amputations.
Technique of Pedicle Flap Repair
At first glance, the performance of pedicle flaps may seem daunting, but a simple V-Y plasty pedicle flap easily can be advanced to cover the defect left by fingertip injury.4,6–10 The V-Y plasty advancement flap technique should be used when the injury leaves more pulp than nail bed. Attempts to use this technique when the opposite situation occurs results in undue tension on the flap and failure of the procedure. Physicians must consider their experience level when deciding to perform this procedure. The technique is not difficult to learn but, at centers with readily available hand and plastic surgeons, referral may be considered.
The V-Y plasty technique preserves the normal contours of the dorsal finger, helps pad the fingertip and preserves normal sensation.6,7,9 The original technique, which used a double lateral V-Y pedicle advancement to close a fingertip amputation, has been largely replaced by the single V-Y plasty technique4 described below.6–10 Use of loupe magnification may assist the performance of this technique. The 12 steps of the single V-Y plasty technique follow:
Step 1. Perform a digital block using 1 percent lidocaine (Xylocaine) without epinephrine administered on both sides of the proximal finger to achieve adequate anesthesia. If more extensive debridement is needed, consider using conscious sedation with an agent such as midazolam (Versed).
Step 2. Drain blood from the finger and apply a tourniquet using a rubber band or a small Penrose drain at the base of the affected digit.
Step 3. Clean the wound thoroughly using saline or water.
Step 4. Debride any devitalized tissue.
Step 5. If there is a portion of the bone protruding from the distal phalanx, smooth or trim it using a rongeur to allow for the advancement of the flap.
Step 7. Skin incisions are made through the full thickness of the skin. Do not undermine the flap itself, because the blood supply for this island pedicle flap comes from beneath. The flap usually has enough mobility to allow for closure of the defect.
Step 8. Advance the flap over the defected area and suture it to the nail bed with either 5-0 or 6-0 nylon sutures (Figure 3b).
Step 10. Remove the tourniquet. Observe the flap for good capillary refill and color. Please note that there may be a delay in filling for five to 10 minutes to access the blood flow.
Step 11. If capillary refill is slow, check the distal sutures to make certain that they were not placed too snugly.
Step 12. The wound is cared for with moist wound healing by applying an antibiotic ointment to the area. A protective splint is often beneficial.
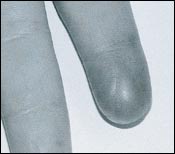
The V-Y pedicle plasty technique allows most patients to regain sensation and two-point discrimination in the fingertip.10 The cosmetic results are usually excellent, with good contour and fingertip padding preserved. Figure 4 shows an example of a fingertip that has undergone the V-Y plasty technique, showing the minimal scar.
Complications
Tissue sloughing can occur if excess tension is applied or if the blood supply is disrupted by undermining the flap. Permanent sensory changes may be noted, including paresthesias, hyperesthesia or a sensation of coldness.6,7,16 Sensory changes are experienced by more than 50 percent of patients with fingertip amputations but often subside with time.16 Infection rarely occurs at this highly vascular location.
While not all fingertip amputations are amenable to the use of the V-Y plasty wounds closed with this technique usually have favorable outcomes. Physicians who perform care in the office, emergency department or urgent care center can readily master this technique.