
Am Fam Physician. 2001;64(6):981-989
See patient information handout on breastfeeding, written by the authors of this article.
Breast milk is widely accepted as the ideal source of nutrition for infants. In order to ensure success in breastfeeding, it is important that it be initiated as early as possible during the neonatal period. This is facilitated by skin-to-skin contact between the mother and infant immediately following birth. When possible, the infant should be allowed to root and latch on spontaneously within the first hour of life. Many common nursery routines such as weighing the infant, administration of vitamin K and application of ocular antibiotics can be safely delayed until after the initial breastfeeding. Postpartum care practices that improve breastfeeding rates include rooming-in, anticipatory guidance about breastfeeding problems and the avoidance of formula supplementation and pacifiers.
One goal of the Healthy People 20101 initiative is to achieve a breastfeeding initiation rate of 75 percent. Breastfeeding is supported by the American Academy of Family Physicians2 and the American Academy of Pediatrics (AAP).3 The AAP recommends continuation of breastfeeding for at least the first full year of life. Clearly, an important goal of family physicians, whether or not they provide maternity care, is to ensure that all women receive support for breastfeeding and encouragement to provide this ideal form of nutrition to their infants (Table 1).3
This article describes ways in which family physicians can facilitate the early initiation and long-term success of breastfeeding in their patients.
Patient Education
The first strategy in ensuring early initiation of breastfeeding should begin during prenatal care. Prenatal education can integrate written materials, support groups and one-to-one discussions between the patient and physician.4 An excellent example of an effective breastfeeding education program is Best Start (Best Start Social Marketing, Tampa, Fla.), which was found to double breastfeeding initiation rates among an inner-city population.5
After admission of the expectant mother to the hospital, the family physician can reiterate the support of breastfeeding and review plans for early breastfeeding management while in the delivery room. Often, breastfeeding preferences are included in the patient’s personal birth plan.
Effects of Early Contact
Immediately following delivery, the healthy infant should be placed on the mother’s chest or upper abdomen. The infant can be dried by delivery room personnel at the bedside to help lessen evaporative heat loss but at this point, skin-to-skin contact between the mother and infant can facilitate breastfeeding. Results of studies have demonstrated that early skin-to-skin contact improves maternal-infant bonding.6,7 Further, infants who have early maternal contact have been found to nurse more effectively at the first feeding and, in some cases, if the baby is left alone on the mother’s chest, it has crawled spontaneously to the breast and suckled.8
Videotapes of infants at the first breastfeeding reveal that newborns who are allowed to go to the breast spontaneously showed better tongue positioning at latch-on, suggesting that “forcing the infant to the breast might abolish the rooting reflex and disturb placement of the tongue.”9 Therefore, it might be advisable to give newborns an opportunity to root and latch on without assistance for up to 60 minutes before intervening to effect the latch-on.
| Advantages for the newborn | |
| Lower incidence of following conditions: | |
| Allergies and asthma | |
| Bacteremia and meningitis | |
| Botulism | |
| Childhood lymphoma | |
| Chronic constipation | |
| Diabetes | |
| Gastrointestinal infections | |
| Infantile eczema | |
| Inflammatory bowel disease | |
| Iron deficiency anemia | |
| Lower respiratory tract infection | |
| Necrotizing enterocolitis | |
| Otitis media | |
| Sudden infant death syndrome | |
| Urinary tract infection | |
| Increased IQ scores later in childhood | |
| Enhanced neurodevelopmental performance | |
| Advantages for the mother | |
| Delayed ovulation resulting in increased child spacing | |
| Earlier return to prepregnancy weight | |
| Increased bone density resulting in lower postmenopausal fracture rate | |
| Less postpartum bleeding | |
| Lower incidence of ovarian cancer | |
| Lower incidence of premenopausal breast cancer | |
| Advantages to society and family | |
| Economic savings from cost of purchasing infant formula | |
| Reduced employee absenteeism related to child illnesses | |
| Reduced health care costs from fewer physician and hospital visits | |
There is conflicting evidence about the long-term effects of early contact on continued, successful breastfeeding. While a 1994 Cochrane Library10 systematic review found three randomized trials reporting no increase in the success of long-term breastfeeding in infants with early contact, results from another trial revealed that breastfeeding rates at weeks 6 and 12 were higher in infants who were allowed early contact with their mother.7 In addition, suckling and skin-to-skin contact within the first hour following birth resulted in a mean duration of breastfeeding that was 2.5 months longer than the duration in maternal-infant pairs not afforded the same early contact.11 Conversely, when infants were separated from their mothers during the early stage of the hospital stay, only 37 percent were breastfeeding at three months compared with 72 percent of infants not separated from their mothers during the early stage of the hospital stay.12
Because early maternal-infant contact is a pleasurable and low-risk intervention, it seems reasonable, based on available evidence, to promote early initiation of breastfeeding. If a mother is separated from her infant, and early contact is not possible, measures should be taken to ensure high quality contact as soon as possible. Support and encouragement by well-trained professionals—physicians, nurses or a lactation consultant—can be of great benefit.13
Positioning and Latch-On
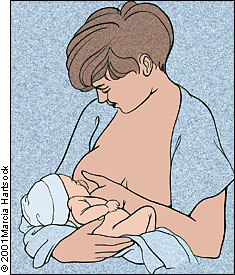
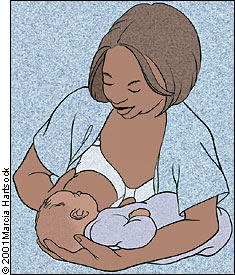
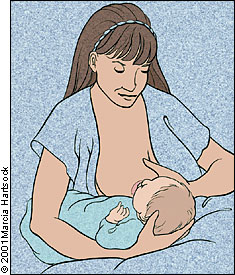
It is unclear whether the use of a specific breastfeeding position in the delivery room is correlated with better outcomes; therefore, it would be prudent to allow the mother to breastfeed in any position that seems comfortable for her or her infant. Options include the cradle hold, cross-cradle hold, football hold, side-lying position and Australian hold (Figures 1 through 5). The latter position might be more difficult to accomplish if the physician needs to perform a perineal repair at this time.
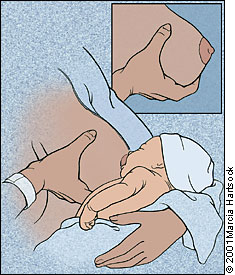
To achieve a proper latch-on, the mother should support her breast using the C-hold (Figure 6). It is important not to have her fingers too close to the nipple because this can result in distortion of the natural shape of the nipple. The infant is then brought close to the breast, with the mother just touching the nipple gently on the baby’s lips. This touch should initiate a reflex causing the infant to open its mouth widely. At this point, the infant should quickly be brought closer to allow a proper latch-on. If the latch-on is done correctly, the entire nipple and most of the areola should be in the baby’s mouth. Newborns are often quite alert during the first hour of life. If a good latch-on is achieved, the infant should be sucking well at the breast and may continue to do so for about 10 minutes.


Effect of Intrapartum Analgesia and Anesthesia
Brazelton, a pioneer in infant behavior, provided evidence as early as 1961 that maternal analgesia led to disorganized behavior in the infant, which can result in a delay in effective breastfeeding and infant weight gain.14 More recent data reveal that both butorphanol (Stadol) and nalbuphine (Nubain) cause a delay in the time to effective breastfeeding when administered to women during labor, particularly if administered more than one hour before delivery.15
Epidural anesthesia has become increasingly popular for pain control during labor. Unfortunately, its effect on breastfeeding when given intrapartum has not been directly studied. In a review of 13 trials evaluating the neurobehavioral effects of epidural anesthesia on infants, seven of these trials showed a negative effect on infant behavior, which the reviewer infers might affect lactation.16 When epidural administration of anesthesia is used to control postoperative pain following cesarean delivery, breastfeeding is affected negatively, but only if a narcotic agent (e.g., buprenorphine [Buprenex]) is infused in the epidural space.16 Postoperative epidural infusion of the anesthetic bupivacaine (Marcaine) alone does not affect the success of breastfeeding and may, in fact, have even less effect on successful breastfeeding than oral ibuprofen.17,18
Effect of Cesarean Delivery
Early, successful breastfeeding can be affected negatively by cesarean delivery.19 Results from one study revealed that women who underwent cesarean delivery were one half as likely to breastfeed exclusively during their hospital stay.20 Nevertheless, if the infant is put to the breast within the first two hours following delivery, the long-term success rate of lactation is unaffected.21 We recommend that an attempt be made to initiate lactation before the end of the first hour (but no longer than two hours) of birth following cesarean delivery. Positioning may be more difficult because of postoperative pain; using the lateral decubitus position for breastfeeding might be preferable. Pillows may also be used to provide support for the area of incision.
Effect of Other Labor Medications
Magnesium sulfate is commonly used for tocolysis and the prevention of seizures in preeclamptic patients. The breast milk of women who receive intravenous magnesium sulfate contains higher concentrations of this medication than that of normal control subjects.22 It has been shown that infants who are breastfed by women treated with magnesium sulfate have only minimally higher magnesium levels. Neonatal magnesium levels are back within the normal range by 24 to 48 hours after the infusion is discontinued.22 There are no study data that evaluate the direct effects of magnesium sulfate on the success of lactation. Nonetheless, magnesium sulfate is presumed to be safe in women who are breastfeeding.23
Many more infants are exposed to oxytocin (Pitocin) during labor. Unfortunately, little information is available about its effect on lactation when administered to women during labor. It is known that oxytocin is important for milk let-down, but its physiologic release is pulsatile in nature. Theoretically, continuous high levels of the drug could alter milk production and let-down, but this theory has not been documented.24 It is, however, a safe medication to use during labor and its use is not a contraindication to breastfeeding.23
Length of Labor
Women who experience a long labor are at risk for problems with breastfeeding. Women with longer labors had lower milk volumes at five days postpartum.5 These women also had a delay in the time of perceived breast fullness. Results of this study also reveal that women who scored higher on an exhaustion scale following labor had similar difficulty with lactation, whether or not they had a long labor.25 While these data demonstrate the negative effect of a long labor on breastfeeding success, no randomized trials exist demonstrating that shortening labor with aggressive use of oxytocin can improve this outcome.
Effect of Nursery Routines
Following the birth of an infant, a number of important nursery routines are carried out in most hospitals (e.g., weighing and measuring the infant, swaddling in a blanket, and administering intramuscular vitamin K and prophylactic ocular antibiotic). As mentioned previously, early skin-to-skin contact is beneficial to maternal-infant bonding and probably also to early breastfeeding success. It appears prudent to delay a number of common nursery procedures until after the first hour of bonding and lactation—but is it safe to delay all of these routines?
Clearly, the weighing and measuring of the infant can be delayed. It is unlikely that the small amount of colostrum ingested during the first feeding will significantly alter the birth weight. Similarly, a delay in the swaddling of the infant is also reasonable. Skin-to-skin contact can maintain temperature stability because of the radiation of heat from the mother to the infant.26 Heat loss can be prevented by placing a cap on the infant’s head and covering the infant with a blanket, while still maintaining the direct skin-to-skin contact with the mother, thus facilitating bonding at the initial breastfeeding. Further, when skin-to-skin contact is practiced in the hospital with premature infants, studies document long-term, increased maternal confidence and milk production.27
The rationale for topical prophylactic antibiotic therapy for the infant’s eyes is to reduce the incidence of conjunctival (Chlamydia and gonorrhea) infections. Administration of either erythromycin or silver nitrate within the first hour of birth is recommended.28 Results from a large randomized trial reveal, however, that only a modest benefit is realized from administration of these topical antibiotics when compared to no medication at all.29 It is further suggested that the elimination of topical prophylactic antibiotic administration is acceptable in low-risk women who were previously screened for sexually transmitted diseases.29 Nonetheless, delaying this procedure until one hour after birth still falls within the accepted standards of care.28
Vitamin K administration is recommended to prevent vitamin K–dependent-bleeding in the neonate.28 This is a disorder of low incidence (0.25 to 1.7 percent), but it is associated with significant morbidity.30 Unfortunately, the correct timing of administration is unknown. As in the case of topical prophylactic antibiotic therapy for conjunctival infections, administration of vitamin K can also be delayed for one hour following delivery.28
The introduction of pacifiers and bottles is also a common practice within the nursery setting. It is thought, however, that both bottles and pacifiers cause “nipple confusion” and contribute to breast refusal and less efficient sucking.31 Pacifier use has been associated with a fourfold drop in breastfeeding rates at six months when compared with nonusers.32 When supplementation is medically indicated, alternatives to bottle feeding include a cup feeding, finger feeding, spoon feeding, eye dropper feeding and the use of a supplemental nutrition system. The latter is a tubing device taped to the breast to allow supplemental formula or pumped breast milk to be given during a breastfeeding.
Rooming-In
Having the infant remain in the mother’s room for the entire postpartum stay, commonly known as rooming-in, can have a beneficial effect on breastfeeding and has been shown to increase the number of daily feedings.33 Study results reveal that more frequent and early breastfeeding leads to better long-term success.34–36 Critics of rooming-in believe that new mothers need more rest and that removing the infant to the nursery will allow them this rest. When this supposition was examined, it was found that mothers with rooming-in infants actually had an equal quantity and quality of sleep compared with mothers whose babies went to the nursery during the night.37
| On-demand schedule of eight to 12 feedings per 24 hours |
| Infant mouth open wide before latch-on |
| Latch-on that includes the entire nipple and most of the areola |
| Infant tongue placed under the nipple |
| Brief pauses in sucking with audible or visible swallowing |
| Infant breathing coordinated with suck and swallow cycle |
| Visible movement of temporomandibular joint during active nursing |
| Mother supports breast with hand (C-hold) throughout feeding during first six weeks |
| Wet diapers at least six to eight times per day |
| Adequate infant weight gain, with return to birth weight by two weeks |
Supplemental Formula
The use of supplemental formula is another common nursery practice that can negatively affect lactation.38,39 Women who feed their infants formula supplements before two weeks of age are only one half as likely to still be breastfeeding at 20 weeks.38 Insufficient milk supply, if suspected, is better managed with a breast pump to stimulate milk production. Use of a hospital-grade electric breast pump is preferred because it is more efficient and will allow simultaneous pumping of both breasts. This step is especially important in the care of small, premature infants or sick infants in whom breastfeeding may be temporarily contraindicated.40
Discharge Instructions
Because mothers and infants are often discharged by 48 hours following delivery, it is extremely important that mothers receive proper discharge instructions from their physician. Information on how to assess the adequacy of breastfeeding is listed in Table 2.
At discharge, plans for contraception should be discussed. While it is true that exclusive breastfeeding is effective in preventing pregnancy, many women choose additional protection.3,41 If they desire hormonal contraception, use of progestin-only pills or injectable progestin (Depo Provera) is preferred. In most cases, it is best to wait until six weeks postpartum, when breastfeeding is well established, before giving hormonal contraception.41
Most hospitals give new mothers a discharge pack that includes samples of artificial formula or manufacturers’ coupons for formula. It has been demonstrated that this practice leads to discontinuation of breast-feeding a mean of 4.18 weeks earlier than in women whose discharge packs include a manual breast pump but no formula samples or coupons.42 Discharge packs for lactating women that include formula samples or coupons should be discouraged.
Early follow-up visits are important to assess breastfeeding adequacy. The AAP recommends an office visit within 48 hours of discharge for mothers and infants leaving the hospital within 48 hours.43 The infant’s weight is an important factor to monitor. Breastfed infants should begin to regain weight by days 4 to 5 of life and should exceed their birth weight by days 10 to 14. This early follow-up visit is also an excellent opportunity for the physician to observe the mother breastfeeding, to assess the latch-on and sucking pattern, and to identify problems.
Breastfeeding support can also be provided through a visiting nurse service. Physicians should check with local agencies to see if personnel trained in lactation support are available. Certification by the International Board of Lactation Consultant Examiners is an excellent measure of extensive training in breastfeeding management. Another source of breastfeeding support in most communities is La Leche League, an organization with local chapters throughout the United States.
Staff Training
Support of breastfeeding by the maternity unit nurses is a key component to a successful breastfeeding program. Physicians may feel that their efforts to promote breastfeeding are occasionally at odds with nursing staff biases or nursery routines. The converse may also be true. The problem need not exist if everyone works together to improve breastfeeding success. It has been shown that breastfeeding rates can be improved by “repeated and extensive professional education” of maternity staff.44 An important way to change medical and nursing staff behaviors is to inform them of evidence-based guidelines currently available that support many of the strategies mentioned in this article for the initial management of breastfeeding.45
With solid support from the medical and nursing staff, it is possible to achieve status as “Baby Friendly” according to the “Ten Steps” of the Baby-Friendly Hospital Initiative of WHO/UNICEF (Table 3).46 Hospitals worldwide that have adopted the “Ten Steps” program report an increase in breastfeeding initiation and duration rates.47