
Am Fam Physician. 2002;65(9):1805-1811
The Achilles tendon, the largest tendon in the body, is vulnerable to injury because of its limited blood supply and the combination of forces to which it is subjected. Aging and increased activity (particularly velocity sports) increase the chance of injury to the Achilles tendon. Although conditions of the Achilles tendon are occurring with increasing frequency because the aging U.S. population is remaining active, the diagnosis is missed in about one fourth of cases. Injury onset can be gradual or sudden, and the course of healing is often lengthy. A thorough history and specific physical examination are essential to make the appropriate diagnosis and facilitate a specific treatment plan. The mainstay of treatment for tendonitis, peritendonitis, tendinosis, and retrocalcaneobursitis is ice, rest, and nonsteroidal anti-inflammatory drugs, but physical therapy, orthotics, and surgery may be necessary in recalcitrant cases. In patients with tendon rupture, casting or surgery is required. Appropriate treatment often leads to full recovery.
The Achilles tendon spans two joints and connects the calcaneus to the gastrocnemius and soleus muscles, comprising the largest and strongest muscle complex in the calf (Figure 1). The tendon is vulnerable to injury because of its limited blood supply, especially when subjected to strong forces.
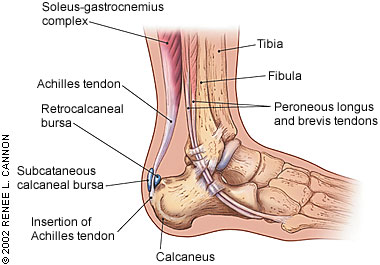
The blood supply to the tendon is provided by longitudinal arteries that run the length of the muscle complex. The area of the tendon with the poorest blood supply is approximately 2 to 6 cm above the insertion into the calcaneus.1 The blood supply diminishes with age, predisposing this area of the tendon to chronic inflammation and possible rupture.
The Achilles tendon does not have a true synovial sheath but instead has a paratenon. The paratenon is a connective tissue sheath that surrounds the entire tendon and is able to stretch 2 to 3 cm with movement, which allows maximal gliding action. The Achilles tendon has been shown to thicken in response to increased activity. The morphologic changes such as decreased cell density, decreased collagen fibril density, and loss of fiber waviness that occur with aging predispose the tendon to injury.2
The normal gait cycle requires extreme motion from within the ankle. With each step, the subtalar joint typically moves 30 degrees (inverts 20 degrees, everts 10 degrees).3 This movement results in repetitive lengthening and shortening of the Achilles tendon complex. Running and jumping further increase the load on the Achilles tendon. Tendons that transmit large loads under these conditions are subject to injury. Extreme shear forces across the tendon complex are believed to cause prolonged loading of the tendon, resulting in micro-trauma and inflammation.4
Common conditions of the Achilles tendon include tendonitis, peritendonitis, tendinosis, rupture, and retrocalcaneobursitis. These conditions are usually caused by overuse and can occur in adolescents and adults (Table 1). Achilles tendon injuries are increasing in prevalence as physical activity becomes more common, especially in older patients. Men older than 30 years are particularly vulnerable to injuries of the Achilles tendon, but persons beginning a sport or increasing activity levels are also at risk.
| Injury | Predisposing factors | Rate of onset | Age of onset | Symptoms | Signs | Treatment | Recovery time |
|---|---|---|---|---|---|---|---|
| Tendonitis | Increased activity, poor-fitting footwear, excessive pronation, poor flexibility | Gradual | Any | Pain over tendon, heel pain, stiffness | Tenderness with palpation; tendon thickened; pain with range of motion | NSAIDs, ice, rest, increased warm-up/stretching, heel lifts | Weeks to months |
| Rupture | Explosivemovements, long-term chronic tendonitis | Sudden | Late 20s | Feeling of being kicked in hearing a “pop”; mild to moderate pain; inability to continue activity | Swelling, inability to palpate back of ankle; feeling or defect; small knot or bulge at proximal portion of Achilles; inability to perform single-leg toe raise on affected side; abnormal Thompson test* | Surgery or Achilles tendon or palpable immobilization | 6 to 12 months |
| Bursitis | Low-riding shoes | Very gradual | Late 40s | Pain in back of heel, worsening with initiation of activity, improving with rest; pain while wearing shoes; limp develops over time | Tender, palpable bursa posterior to calcaneus | Ice, stretching, NSAIDs, heel cups | Weeks |
Achilles Tendonitis and Peritendonitis
ILLUSTRATIVE CASE ONE
A 45-year-old man presents with pain and a “knot” on his right heel after increasing his running frequency, training time, and distance in preparation for a marathon.
INCIDENCE
Achilles tendonitis occurs in about 10 percent of runners, but the condition also occurs in dancers, gymnasts, and tennis players.3,4 Running produces forces up to eight times the body's weight, placing significant repetitive stress on the tendon for prolonged periods.5 Tendonitis in athletes is usually caused by training errors such as incorrect running technique or wearing improperly fitting shoes; however, it is also related to hyperpronation of the foot and contracture of the gastrocnemius-soleus complex.6 Abnormal biomechanics and friction from extrinsic or external pressure are believed to cause symptoms.7 Achilles tendonitis is common when persons first take up athletic activities.
Achilles tendonitis often interferes with activities. One study8 showed that 56 percent of competitive track and field athletes with Achilles tendonitis discontinued all sporting activities for a minimum of four weeks to promote healing. Delayed or missed diagnosis of Achilles tendon rupture is also common, with 23 percent of patients initially being misdiagnosed.9 The tendon defect can be disguised by hematoma. Plantar flexion power (from extrinsic foot flexors) may continue to be present, and the Thompson test can be falsely normal if accessory ankle flexors are squeezed during the physical examination.2 Consequently, all patients with heel pain should be evaluated for Achilles tendonitis.
DIAGNOSIS
A detailed history is necessary, including level of training, technique, footwear, previous injury, and treatment. Injury typically occurs in persons who are physically active and subject the tendon to repetitive forces beyond its ability to heal.10 The typical symptom of tendonitis is pain or tenderness proximal to or at the insertion to the calcaneus. Peritendonitis, an inflammation of the tendon sheath, commonly leads to localized tenderness and burning that eventually develop into pain about 2 to 6 cm above the tendon insertion. This pain is related to exercise. In tendonitis and peritendonitis, symptoms usually develop gradually, and the patient typically presents with pain and stiffness over the Achilles region. The pain may lessen with walking or when heat is applied to the area and worsen with more strenuous activity.
A thorough physical examination is very important to the diagnosis, and it should be performed with the patient lying prone, feet hanging off the examination table. Palpation of the Achilles tendon often elicits tenderness along the tendon. Active range of motion may also elicit discomfort. It is important to assess the thickness and consistency of the tendon and palpate for a discrepancy in thickness between right and left legs. Range of motion of the ankle joint should also be evaluated. Pain elicited by rubbing the tendon between the fingers is a sign of peritendonitis. Crepitation is often present within the Achilles tendon, and a slight thickening of the paratenon may be felt. More serious injuries to the tendon, such as tears and ruptures, must be considered during the examination.
TREATMENT
It is important to inform patients that symptoms may persist for several months. The early phase of treatment emphasizes control of inflammation and pain using ice, rest, and non-steroidal anti-inflammatory drugs (Figure 2). Control of biomechanical factors by correcting malalignment with appropriate shoes, using appropriate training techniques, and losing weight is important to reduce further inflammation of the tendon. A slow, gentle warm-up before exercise and icing after exercise will help patients who want to continue athletic training. If conservative measures fail, physical modalities such as ultrasound therapy and flexibility training may be added to the treatment protocol. Stretching may stimulate a healing response, and one study11 showed that calf muscle training is associated with a faster recovery time. Referral for possible surgical intervention should be made if no improvement occurs after six months of nonoperative treatment.
Tendinosis
Tendinosis is a diffuse thickening of the tendon without histologic evidence of inflammation caused by intertendinous degeneration. This condition is common in persons older than 35 years and may gradually develop as a result of ongoing microtrauma, aging, vascular compromise, or a combination of these factors.12 Pure tendinosis may produce no clinical symptoms or present as a painless, palpable nodule on the Achilles tendon.
The tendinosis cycle begins with an increased demand on the Achilles tendon. Factors such as vascular compromise and aging result in inadequate repair of the tendon matrix and tenocyte death.6 The cycle leads to further impairment of matrix production, causing increased predisposition to injury and microtears within the tendon.2 The cycle ultimately results in collagen degeneration, fibrosis, and calcification within the tendon. The diagnosis of tendinosis is made on physical examination when a thick unilateral or bilateral nodular cord is present. Treatment of tendinosis is the same as that for tendonitis.
Achilles Tendon Rupture
ILLUSTRATIVE CASE TWO
During a basketball game, a healthy 37-year-old man planted his right foot as he moved toward the basket. He later described feeling as though someone had stepped on the back of his shoe while he heard a faint “pop” sound and fell to the ground. He was able to bear weight on his right foot but could not push off it. On physical examination, the patient was found to have some strength on plantar flexion, but he could not perform a toe raise, and he had an abnormal Thompson test (described below).
INCIDENCE
Achilles tendon rupture occurs most commonly in men 30 to 50 years old and is increasing in frequency as more people exercise. Most ruptures originate during strenuous physical activities, especially basketball, tennis, football, and softball13 (Table 2). Spontaneous rupture can occur in the elderly. The diagnosis can be elusive because some function frequently remains. One study14 showed that as many as 20 to 30 percent of Achilles tendon ruptures are not diagnosed at the initial visit to a physician.
| Tendonitis |
| Cross-country running |
| Track and field |
| Walking |
| Cycling |
| Construction work |
| Achilles rupture |
| Football |
| Baseball |
| Basketball |
| Softball |
| Tennis |
| Racquetball |
The diagnosis is made following an appropriate history and physical examination (Table 1).15 The most common description of injury is feeling or hearing a “pop” in the back of the ankle during strenuous movement. The patient may have only minimal pain. On physical examination, the patient may retain some strength in plantar flexion because of the action of other muscles in the foot and leg (e.g., flexor digitorum, flexor hallucis longus, tibialis posterior, peroneus longus, and peroneus brevis muscles). The Thompson test should be performed on all patients with suspected Achilles tendon injury.
THOMPSON TEST
The patient should lie prone on the examination table, flexing the knee on the injured side. The calf should be gently squeezed by the physician, who watches for plantar flexion in the patient's foot. If the foot moves, the tendon is presumed to be at least partially intact. No movement is indicative of rupture, and the test results are considered abnormal. If the Thompson test is equivocal, a sphygmomanometer should be placed on the patient's calf and inflated to 100 mm Hg. The affected foot should be dorsiflexed. The pressure will rise to approximately 140 mm Hg if the tendon is intact. In a patient with an Achilles rupture, only a flicker of movement on the pressure gauge is discernible with dorsiflexion.16
If the diagnosis is still unclear, an ultrasound or magnetic resonance imaging study may be helpful.
TREATMENT
Treatment of Achilles tendon rupture is controversial. The principal treatment is surgery plus immobilization, or immobilization alone. Early complications from surgery (infection and skin breakdown) occur at higher rates when compared with the rates of immobilization alone (17 percent and 0.8 percent, respectively). Immobilization has a higher rerupture rate than surgery (13.4 percent and 1.4 percent, respectively) and a slower time to full participation in sports.17
The trend in treatment in younger persons who want to return to sports is surgery; casting is preferred for use in older, less active persons. If casting is used, immobilization is recommended for eight to 12 weeks, with at least four weeks of nonweight-bearing. Surgery is usually followed by six to eight weeks of immobilization. The current trend is toward a shorter period of nonweight-bearing (two to three weeks or less). A recent study18 showed that 24 hours of nonweight-bearing followed by six weeks of immobilization with physical therapy and ambulation caused no increase in complications. However, most orthopedic surgeons still recommend the use of crutches for at least two to three weeks before supported ambulation is attempted.
Retrocalcaneal Bursitis
ILLUSTRATIVE CASE THREE
A 57-year-old woman described having significant heel pain. The pain began gradually each morning, and by the end of the day she was unable to walk without a limp. Symptoms seemed to improve slightly on weekends and during vacations. On examination, she was found to have swelling and erythema on the posterior portion of the heel at the tendon insertion. The bursa was easily palpated, and this action produced pain.
INCIDENCE
Retrocalcaneal bursitis usually affects middle-aged and elderly patients but can also occur in athletes as a result of overuse. The most common presentation is pain around the insertion of the Achilles tendon. The pain is usually worse at the beginning of an activity such as walking or running, and diminishes as the activity continues. Patients often develop a limp, and wearing shoes may eventually become increasingly painful. On examination, significant swelling and erythema are present. A characteristic enlargement (known as a “pump bump”) may also be present. It may be possible to palpate the retrocalcaneal bursa and a bursa between the tendon and the skin. Direct palpation often reproduces symptoms. A radiograph of the area often shows a calcified distal Achilles tendon or a bone spur on the superior portion of the calcaneus (called a Haglund deformity).
TREATMENT
Treatment is a course of anti-inflammatory drugs, use of a heel cup, and alternating ice and heat therapy. Stretching the Achilles tendon is very important and should be emphasized. In severe cases, patients can wear an open-back shoe to reduce pain. This area should not be injected with corticosteroids because the Achilles tendon often tears after such treatment. If conservative treatment fails, surgery to excise any bone spurs and debridement of the retrocalcaneal bursa may be helpful.