
Am Fam Physician. 2002;66(1):99-102
The development of topical anesthetics has provided the family physician with multiple options in anesthetizing open and intact skin. The combination of tetracaine, adrenaline (epinephrine), and cocaine, better known as TAC, was the first topical agent available for analgesia of lacerations to the face and scalp. Cocaine has been replaced with lidocaine in a newer formulation called LET (lidocaine, epinephrine, and tetracaine). For analgesia to nonintact skin, LET gel is generally preferred over TAC because of its superior safety record and cost-effectiveness. EMLA (eutectic mixture of local anesthetics) is perhaps the most well-known topical anesthetic for use on intact skin. EMLA can be used to anesthetize the skin before intramuscular injections, venipuncture, and simple skin procedures such as curettage or biopsy. To be fully effective, EMLA should be applied at least 90 minutes before the procedure. ELA-Max is a new, rapidly acting topical agent for intact skin that works by way of a liposomal delivery system and is available over the counter. Other delivery vehicles for topical anesthesia currently in development, including iontophoresis and anesthetic patches, may one day give patients and physicians even more flexibility.
Topical anesthetics were developed in the latter half of the 19th century, starting with a description of the topical uses for cocaine.1 However, it has taken nearly a whole century for effective and safe topical anesthetics to become readily available. Today, pain can be effectively alleviated for such procedures as cryotherapy, shave biopsy, and curettage of molluscum contagiosa. Procedures such as laceration repair, which at one time required the use of painful infiltrative anesthetics, can now be accomplished safely and comfortably with the use of topical anesthetics. An additional advantage of topical anesthetics in laceration repair is that wound margins are not distorted. A summary of various topical anesthetics is provided in Table 1.
| Anesthetic product | Methods | Onset/duration | Effectiveness | Complications |
|---|---|---|---|---|
| TAC (0.5% tetracaine, 1:2,000 epinephrine, and 11.8% cocaine) | 2 to 5 mL (1 mL per cm of laceration) applied to wound with cotton or gauze for 10 to 30 minutes | Onset: effective 10 to 30 minutes after application Duration: not established | May be as effective as lidocaine for lacerations on face and scalp | Rare severe toxicity, including seizures and sudden cardiac death |
| LET (4% lidocaine, 1:2,000 epinephrine, and 0.5% tetracaine) | 1 to 3 mL directly applied to wound for 15 to 30 minutes | Onset: 20 to 30 minutes Duration: not established | Similar to TAC for face and scalp lacerations; less effective on extremities | No severe adverse effects reported |
| EMLA (2.5% lidocaine and 2.5% prilocaine) | Thick layer (1 to 2 g per 10 cm2) applied to intact skin with covering patch of Tegaderm | Onset: must be left on for 1 to 2 hours Duration: 0.5 to 2 hours | Variable, depending on duration of application | Contact dermatitis, Methemoglobinemia (very rare) |
| Iontophoresis | Small current applied to lidocaine-soaked sponges on intact skin | Onset: 10 minutes Duration: 10 to 20 minutes | Good for small procedures, depth of anesthesia greater than EMLA | Stinging sensation; may burn skin if high current |
Tetracaine, Adrenaline (Epinephrine), and Cocaine
Tetracaine, adrenaline, and cocaine (TAC), a compound of 0.5 percent tetracaine (Pontocaine), 0.05 percent epinephrine, and 11.8 percent cocaine, was the first topical anesthetic mixture found to be effective for nonmucosal skin lacerations to the face and scalp.2 From 2 to 5 mL of solution is applied directly to the wound using a cotton-tipped applicator with firm pressure that is maintained for 20 to 40 minutes.2,3 However, the use of TAC is no longer supported by the literature because of general concern about toxicity and expense, and federal regulatory issues involving medications containing cocaine.
Lidocaine, Epinephrine, and Tetracaine
To create a safer and more cost-effective alternative to TAC, 4 percent lidocaine (Xylocaine) was substituted for cocaine and combined with 0.1 percent epinephrine and 0.5 percent tetracaine to create a newer topical anesthetic (lidocaine, epinephrine, and tetracaine [LET]). It is not available commercially and must be compounded as a liquid or gel formulation. LET is used on nonmucosal skin lacerations by placing a few drops directly into the wound. A cotton-tipped applicator with 1 to 3 mL of the gel or solution is then applied directly to the wound with firm pressure for 15 to 30 minutes.4,5 Both the solution and the gel have been safely used in children older than two years of age, and both forms are equally effective.6 Anesthetic failure rates for repair of lacerations on the face and scalp with LET gel were only about 5 percent in one study.7 LET is slightly less effective on extremity lacerations.7 If adequate anesthesia is not achieved topically, an infiltrative anesthetic may be injected locally, provided the maximal lidocaine dosage of 3 to 5 mg per kg of lidocaine is not exceeded.
There have been no reports of toxicity with LET, but avoiding mucous membranes is recommended. When working near mucous membranes, LET gel is better than the solution because it stays within the wound. Because LET contains epinephrine, application to end-arteriolar parts of the body, such as the digits, should be avoided. Caution must also be exercised when contemplating the use of LET in contaminated wounds, complex wounds, or wounds larger than 6 cm. LET and TAC do not work on intact skin.
Eutectic Mixture of Local Anesthetics
Most pure anesthetic agents exist as solids. Eutectic mixtures are liquids and melt at lower temperatures than any of their components, permitting higher concentrations of anesthetics. Eutectic mixture of local anesthetics (EMLA) represents the first major breakthrough for dermal anesthesia on intact skin. It consists of 25 mg per mL of lidocaine, 25 mg per mL of prilocaine, a thickener, an emulsifier, and distilled water adjusted to a pH level of 9.4.3
EMLA is applied in a thick layer (1 to 2 g per 10 cm2, up to a maximal dose of 10 g) to intact skin.8 After application, the area is covered with a patch of Tegaderm or clear plastic wrap to facilitate penetration through the stratum corneum (Figure 1). Depth of anesthesia depends on contact time with EMLA. Anesthetic effect has been shown to reach a maximal depth of 3 mm after a 60-minute application, and 5 mm after a 120-minute application.9 It was also found that dermal analgesia continues and may even increase for 30 to 60 minutes after the cream is removed.9 EMLA should not be applied to the palms and soles because of variable penetration.

EMLA has been approved by the U.S. Food and Drug Administration (FDA) only for use on intact, nonmucosal skin. Recent studies have shown that EMLA can also be effectively used on extremity lacerations. One study showed that 85 percent of children whose lacerations were treated with EMLA required no further anesthesia before suturing.10 The drawback is the 90-minute wait required between the application of EMLA and onset of laceration repair. EMLA has been shown to work effectively on genital mucosa in a study of women undergoing laser treatment of condylomata acuminata.11 Current studies have not established safe and optimal dosages for either of these off-label uses.10
EMLA has been associated with occasional adverse reactions, including blanching and redness at the application site.8,12 Perhaps the most serious complication is methemoglobinemia. Cases of methemoglobinemia have occurred in infants younger than three months of age who were exposed to high doses of EMLA for prolonged periods.8 Since then, other studies have demonstrated that 1 g of EMLA applied to the penis for one hour is safe to use in healthy, full-term neonates before circumcision.13,14 Although using EMLA is better than using no anesthesia at all, the dorsal penile nerve block still offers superior analgesia before circumcision, and the methods may be combined.13
Liposomes
Liposomes are comprised of lipid layers surrounded by aqueous layers. They are able to penetrate the stratum corneum because they resemble the lipid bilayers of the cell membrane. A liposomal delivery system recently became available as an over-the-counter product called ELA-Max. It contains 4 percent lidocaine cream in a liposomal matrix and is FDA-approved for the temporary relief of pain resulting from minor cuts and abrasions. ELA-Max is applied to intact skin for 15 to 40 minutes without occlusion.15–17 In limited studies, ELA-Max has also proved effective in providing dermal analgesia before chemical peeling.18 The safety of its application to mucous membranes has not been evaluated.5 Despite a paucity of data and lack of an FDA indication, clinicians are beginning to use ELA-Max for topical anesthesia before other dermatologic procedures.
Anesthetic Patches
Several anesthetic patch preparations using varying concentrations of lidocaine have shown promise for topical anesthesia. The lidocaine gel patch known as Lidoderm was recently approved by the FDA for the treatment of pain caused by postherpetic neuralgia, but it has not been studied for use in procedures.
Iontophoresis
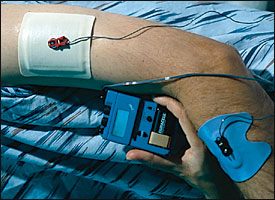
Iontophoresis is a method of delivering a topical anesthetic with a mild electric current. Lidocaine-soaked sponges are applied to intact skin, and electrodes are placed on top of the anesthetic. A DC current is then applied to the skin (Figure 2). The anesthetic effect occurs within 10 minutes and lasts approximately 15 minutes. The depth of anesthesia can reach up to 1 to 2 cm.12
Although the effectiveness of iontophoresis has been compared favorably to that of EMLA, it remains underused. Some patients find the mild electrical sensation uncomfortable. The apparatus is expensive and bulky, and cannot be used over large surface areas of the body.8 Other applications using iontophoresis are still being developed.