
Am Fam Physician. 2003;67(3):511-517
A more recent article on dental problems in primary care is available.
Dental caries, a bacterial disease of teeth characterized by destruction of enamel and dentine, is often the underlying cause of dental pain. When a carious lesion impinges on the dental pulp, pulpitis follows and, ultimately, necrosis of the pulp occurs. Untreated necrosis may lead to a localized abscess or a spreading infection into the surrounding soft tissue that results in cellulitis. Immediate treatment involves antibiotic therapy for cellulitis, perhaps with drainage of abscesses, while definitive treatment requires root canal therapy or extraction of the involved tooth. Pericoronitis is an inflammation of the soft tissue overlying a partially erupted tooth. Localized cases respond to irrigation. Secondary cellulitis can develop. Definitive treatment may require surgical extraction of the underlying tooth or excision of the gum flap. Avulsion of a permanent tooth secondary to trauma is a true dental emergency. The tooth should be reimplanted on the spot, and the patient should be seen immediately by a dentist for splinting and antibiotic prophylaxis. Most dental problems can be prevented with regular dental care and steps to minimize risks of oral trauma.
Dental emergencies (Table 1) are extremely common in America. In one recent survey,1 22 percent of the general population had experienced orofacial pain in the preceding six months, and 12 percent experienced toothache. In 1996, American students missed 1,611,000 school days because of acute dental problems.2
| Diagnosis | Definition | Presentation | Complications | Treatment |
|---|---|---|---|---|
| Reversible pulpitis | Pulpal inflammation | Pain with hot, cold, or sweet stimuli | Periapical abscess, cellulitis | Filling |
| Irreversible pulpitis | Pulpal inflammation | Spontaneous, poorly localized pain | Periapical abscess, cellulitis | RCT, extraction |
| Abscess | Localized bacterial infection | Localized pain and swelling | Cellulitis | I & D and RCT or extraction |
| Cellulitis | Diffuse soft tissue bacterial infection | Pain, erythema, and swelling | Regional spread | Antibiotics and RCT or extraction |
| Pericoronitis | Inflamed gum over partially erupted tooth | Pain, erythema, and swelling | Cellulitis | Irrigation, antibiotics if cellulitis also present |
| Tooth fracture | Broken tooth | Clinical examination and radiography | Pulpitis and sequelae | Fillings, with or without RCT, extraction |
| Tooth luxation | Loose tooth | Clinical examination and radiography | Aspiration, pulpitis, and sequelae | Splinting, with or without RCT, extraction |
| Tooth avulsion | Missing tooth | Clinical examination | Ankylosis, resorption | Reimplantation and splinting |
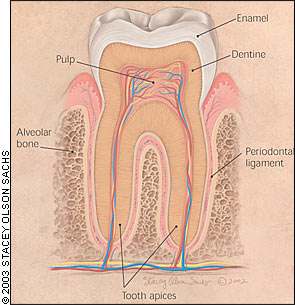
Dental Anatomy
All human teeth are composed of three structural layers3 (Figure 1). The outer layer of enamel is an extremely hard, highly mineralized, crystalline structure that covers and protects the crown of the tooth. The core structure of the tooth is composed of dentine. At the center of the tooth is the pulp chamber, which contains blood vessels and nerves that connect to the jaw's vascular and nervous supply through the tooth apices. The tooth roots are attached to the surrounding alveolar bone of the tooth socket via the periodontal ligament.
Dental Pain
The first step in the evaluation of oral pain should be to determine its etiology. Dental sources are most common. However, pain arising from nondental sources such as myofascial inflammation, migraine headache, maxillary sinusitis, nasal tissues, ears, temporomandibular joints, and neuralgias always must be considered and excluded.4
CARIOUS ORIGIN
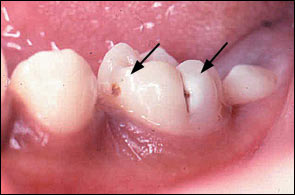
Dental caries is a bacterial disease of teeth characterized by demineralization of tooth enamel and dentine by acid produced during the fermentation of dietary carbohydrates by oral bacteria, predominately Streptococcus mutans.5,6 Dental decay presents visually as opaque white areas of enamel with grey undertones (Figure 2) or, in more advanced cases, as brownish, discolored cavitations (Figure 3). Caries is initially asymptomatic. Pain does not occur until the decay impinges on the pulp, and an inflammatory process develops.

Reversible pulpitis is mild inflammation of the tooth pulp caused by caries encroaching on the pulp. Pain is triggered by hot, cold, and sweet stimuli, lasts for a few seconds, and resolves spontaneously.7 Treatment involves removal of the carious tissue and placement of a dental restoration, or filling.
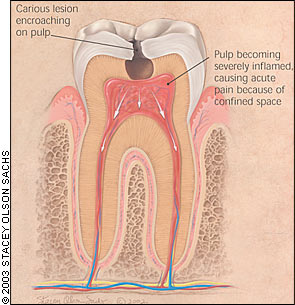
If a carious lesion causing reversible pulpitis is not treated, the condition will progress to irreversible pulpitis, a severe inflammation of the pulp (Figure 4). Pain becomes severe, spontaneous, and persistent, and is often poorly localized.7 The only way to definitively treat the discomfort is root canal treatment (removal of the pulp and filling of the empty pulp chamber and canal) or extraction of the tooth. The urgency of referral to a dentist should be determined by the patient's level of discomfort, but examination should not be delayed for more than a few days. The pain should be managed with appropriate analgesia such as a nonsteroidal anti-inflammatory drug (NSAID) or a weak opioid combined with an NSAID or acetaminophen in an appropriate quantity to last until the dental appointment. Patients should be warned of the risks of further complications if they do not have prompt definitive treatment and advised to return to their physician if symptoms change or worsen before they see the dentist.
A severely inflamed pulp will eventually necrose, causing apical periodontitis, which is inflammation around the apex of the tooth (Figure 5). Pain is severe, spontaneous, and persistent, but unlike that of irreversible pulpitis, localizes to the affected tooth. The tooth is sensitive to percussion with a metal object.7 Regional lymphadenopathy can be present. Management is root canal treatment or extraction. Referral to a dentist should occur as soon as possible, with provision of appropriate pain medication. Antibiotics are not necessary, but patients should be warned to return to the physician immediately if swelling or other evidence of spreading infection occurs.
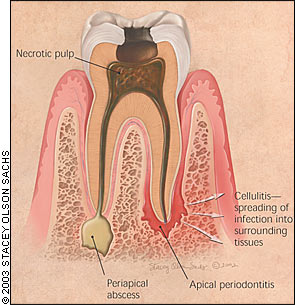
Apical abscess is a localized, purulent form of apical periodontitis (Figures 5 and 6). It may present clinically as a fluctuant buccal or palatal swelling, with or without a draining fistula. Regional adenopathy is usually present. If pus is draining, pain usually is not severe. Antibiotics are not necessary unless concurrent cellulitis is present. Acute incision and drainage of a fluctuant area by an appropriately trained physician would be reasonable. Definitive therapy is root canal treatment or extraction. Patients should be seen by a dentist within one to two days and provided with appropriate pain medication in the meantime.

Cellulitis may follow apical periodontitis if the infection spreads into the surrounding tissues (Figure 5). Diffuse, tense, painful swelling of the affected tissues occurs. Regional lymphadenopathy is common, and fever may be present. The infection can spread into the major fascial spaces of the head and neck,8 with the attendant risk of airway compromise. Maxillary infection also may spread to the periorbital area, increasing the risk of serious complications that include loss of vision, cavernous sinus thrombosis, and central nervous system involvement.8
The examination should focus on determining if the cellulitis remains localized or has spread regionally. Patients with localized cellulitis that is deemed appropriate for outpatient therapy should be treated by the physician with antistreptococcal oral antibiotics, such as oral penicillin in a dosage of 500 mg three times daily in adults or 50 mg per kg per day divided into three doses in children.
In the event of true penicillin allergy, erythromycin or clindamycin (Cleocin) may be substituted. Appropriate pain medication should be provided. Definitive therapy is root canal treatment or extraction, which in selected cases may be delayed until swelling has subsided. Patients should be evaluated by a dentist within one to two days but warned to return earlier if swelling or pain worsens.
If infection extends regionally into the deep spaces of the head and neck as evidenced by severe swelling, the risk of life-threatening complications such as airway compromise is substantial. Generally, these patients should be hospitalized and provided with surgical and infectious disease consultation. Imaging, usually with computed tomographic scanning, is mandatory, as is surgical drainage if abscess formation is detected. Intravenous broad-spectrum antibiotic treatment should be started immediately and should include coverage for anaerobes.8
In general, the same principles of initial evaluation and management apply to the primary and permanent dentition. However, carious lesions of the primary teeth less frequently cause pain and abscesses and more frequently drain cutaneously than lesions of the permanent dentition. The systemic effects of infection are more pronounced in children, with rapid temperature elevations, greater risk of dehydration, and more rapid spread of infection.8
PERIODONTAL ORIGIN
Periodontal disease is an inflammatory destruction of the periodontal ligament and supporting alveolar bone. The main etiologic agent is bacterial plaque. Multiple bacteria are implicated, but as the disease progresses, gram-negative anaerobes predominate.5 Patients with chronic periodontal disease or patients who have a foreign object lodged in the gingiva may present with an acute periodontal abscess. Symptoms include throbbing pain with erythema and swelling over the affected tissue. The tooth is normally tender to percussion and shows increased mobility.
If left untreated, the abscess may rupture or, less commonly, progress to cellulitis. Patients require referral to a dentist within 24 hours for drainage and debridement of the infected periodontal area. Antibiotics are not normally indicated if debridement is successful, but their use remains controversial.9
WISDOM TOOTH ORIGIN
Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth, most commonly a wisdom tooth (Figure 7). It occurs when bacterial plaque and food debris accumulate beneath the flap of gum covering the partially erupted tooth. Inflammatory edema, often complicated by trauma from the opposing tooth, leads to swelling of the flap, pain, tenderness, and a bad taste caused by pus oozing from beneath the flap.7 Regional lymphadenopathy is common, and cellulitis and trismus (inability to open the mouth fully) can occur. In severe cases, the oral airway can be compromised.
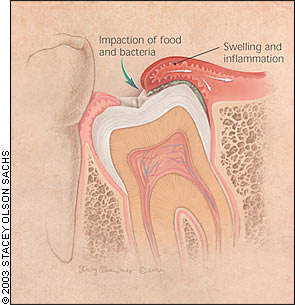
If pericoronitis is well localized, hot salty mouthwashes and irrigation under the flap can resolve symptoms in the majority of cases.10 Localized cases that do not respond to mechanical therapy and more severe disseminated cases with spreading cellulitis should be treated with penicillin and appropriate pain medication as described in the section on carious origin of pain. Referral to a dentist should occur as quickly as possible so the patient can be evaluated to see if symptomatic treatment can suffice until eruption is complete or if surgical therapy to remove the gum flap or underlying tooth is necessary.
Dental Trauma
Dental trauma is extremely common. Children are particularly affected, with one third of five year olds having suffered injury to their primary teeth, and one fourth of 12 year olds having suffered injury to their permanent teeth.11 Injuries to teeth and their supporting structures can be classified as fractures, lateral or extrusive luxation (loosening and displacement of the tooth), intrusion (displacement of the tooth vertically into the alveolar bone), and avulsion (complete displacement of the tooth out of its socket).12
The mechanism of injury and timeline are particularly important aspects of the history because they define the risk of associated injuries and available treatment options. Examination should focus on related soft tissue injuries and the need for suturing, signs of tooth loosening, displacement or fracture, and disturbance in the bite or other signs of alveolar fracture. Complete diagnosis requires at least one dental radiograph in all cases.
All patients with traumatized teeth ultimately need follow-up with a dentist for complete diagnosis and long-term care. Long-term sequelae can include pulp death, root resorption, and displacement or developmental defects of permanent tooth successors.
Tooth fractures may involve the crown, the root, or both, with or without exposure of the pulp. Fractures limited to the enamel and small amounts of dentine that are not sensitive may not require immediate treatment but should be checked by a dentist. Fractures exposing the pulp are often painful, and patients with this condition require timely referral to a dentist. Tooth fragments should be kept hydrated as they could possibly be reattached. Definitive treatment may involve root canal therapy or extraction.
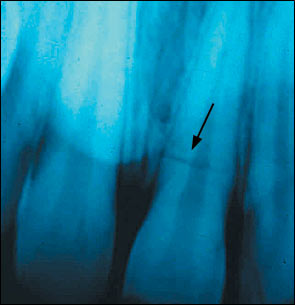
Fractures of the root usually require a radiograph for detection (Figure 8) unless the tooth is particularly loose and the fracture occurred close to the gingival margin. Treatment may involve root canal therapy, splinting, or extraction, depending on the exact nature of the root fracture.
Teeth subject to lateral or extrusive luxation have been displaced and are loose. In the primary dentition, if the traumatized teeth are so loose that they are in danger of being aspirated or if they interfere with normal occlusion, immediate referral to a dentist for extraction is required.12 Luxated permanent teeth require dental referral for repositioning, splinting, or root canal therapy, along with long-term follow-up.13 Any luxated tooth that interferes with normal occlusion requires immediate dental evaluation and treatment to avoid pain and further complications.
Teeth subject to intrusive luxation have been intruded into the alveolar bone, which may occur to the point that the teeth are not visible. With regard to injuries to the primary dentition, dental referral is required for monitoring to determine if the teeth will re-erupt. For injuries to the permanent teeth, dental referral is required for monitoring or treatment to promote re-eruption (surgical or orthodontic), often coupled with root canal therapy.13
Avulsed teeth are a true dental emergency. Primary teeth are never reimplanted.12 In the case of permanent teeth, time is of the essence. Immediate on-scene reimplantation is the preferred method of treatment. If the tooth is visibly contaminated, it should be gently rinsed in cold running tap water and then reimplanted. Care should be taken not to touch, rub, or clean the root, which could remove periodontal ligament fibers and reduce the chance of successful reimplantation. The patient should then see a dentist immediately for splinting and antibiotic prophylaxis.
If immediate on-scene reimplantation is not possible, the tooth should be transported in the patient's buccal sulcus, milk, or a specialized tooth transport container to the physician's or dentist's office. The tooth should then be immediately reimplanted. If rinsing is required, normal saline should be used, and any clot present in the socket should be flushed out before reimplantation.
Antibiotic prophylaxis with penicillin should be prescribed, tetanus vaccine should be administered if the patient has not received it in the past five years,14 and the patient should be immediately referred to a dentist for splinting and further therapy. Avulsed teeth that have not been managed in an appropriate and timely fashion should not be discarded. Alternative, but less optimal, treatments are available.13
Prevention
Dental caries and periodontal disease can be prevented by decreasing ingestion of sugar-containing food items and employing regular tooth brushing and appropriate fluoride use. Regular dental examinations with early treatment of carious lesions can substantially reduce the risk of serious complications.
Most dental trauma occurs in children, and its occurrence can be reduced substantially. Family physicians should advocate the use of appropriate mouthguards and face shields in organized sports.15
Dental Referral
Family physicians often ask the question, “What sort of dentist should I refer this patient to?” In most cases, a general dentist can meet the needs of patients with the problems described in this article. Children younger than three years and children who may present a behavior problem in the dental chair should be referred to a dentist with significant experience in managing children. Adults who do not wish to attempt to keep their teeth or who have significant facial swelling should be referred to an oral surgeon.