
Am Fam Physician. 2003;67(9):1953-1956
In children with positional head deformity (posterior plagiocephaly), the occiput is flattened with corresponding facial asymmetry. The incidence of positional head deformity increased dramatically between 1992 and 1999, and now occurs in one of every 60 live births. One proposed cause of the increased incidence of positional head deformity is the initiative to place infants on their backs during sleep to prevent sudden infant death syndrome. With early detection and intervention, most positional head deformities can be treated conservatively with physical therapy or a head orthosis (“helmet”).
In 1992, the American Academy of Pediatrics (AAP) initiated the “Back to Sleep” campaign recommending that infants be placed to sleep in the supine position to reduce the incidence of sudden infant death syndrome (SIDS).1 Although the rate of SIDS decreased from 1992 to 2000,2 the practice of placing an infant on the back during sleep can result in flattening of the occipital area of the skull. The incidence of positional head deformity is estimated to have risen fivefold since 1992, and the condition now may occur in one of every 60 live births.3 Family physicians should look for positional head deformity because early intervention may reduce adverse outcomes.
Illustrated Case
An otherwise healthy 10-week-old boy had facial asymmetry with his eyes not in alignment. He was delivered vaginally after a normal pregnancy, and there were no significant antenatal, delivery, or postnatal complications. At four months of age his eyes appeared unequal in position, the right occiput was markedly flattened, and the right forehead protuberant (Figure 1). Consultation with a craniofacial surgeon produced a diagnosis of positional head deformity (posterior plagiocephaly), and the child was referred to a pediatric physical therapist.
Definitions and Etiology
Plagiocephaly is derived from the Greek words meaning “oblique head.” The condition can result from either premature closure of the lambdoidal suture (synostotic plagiocephaly) or positional head deformity (nonsynostotic plagiocephaly). Synostotic plagiocephaly occurs in approximately one of every 100,000 infants.4 Positional head deformity is not as rare; before 1996, the incidence was one of every 300 healthy infants.5 Positional head deformity is caused by external pressures on the rapidly developing skull from prolonged exposure to one position. Risk factors associated with positional head deformity are premature birth, hypotonic muscle disorders, congenital torticollis, and intrauterine constraint (such as in multiple gestation or oligohydramnios).6
| Examination | Signs of PHD or synostosis |
|---|---|
| Palpate lambdoidal suture | Palpable ridge suggests synostosis. |
| Check ear position | Ear on flattened side more posterior than the other ear suggests synostosis. |
| Ear on flattened side more anterior than the other ear suggests PHD. | |
| Assess facial symmetry | Forehead protruding on the side of the flattening suggests PHD. |
| Observe unilateral “bald spot” | A unilateral bald spot suggests PHD. Physician should palpate occiput for flattening. |
| Inspect by aerial view | “Parallelogram-shaped” head suggests PHD. |
In 1993, the American Society of Craniofacial Surgeons noted an increase in the incidence of posterior cranial deformities in infants who had no predisposing risk factors.7 These reports were similar to increases in the incidence reported in other countries.8 The relationship of this increased incidence to the “Back to Sleep” campaign was proposed in 1996 and was supported by evidence of a rapid increase in positional head deformity without any significant change in the rate of synostotic plagiocephaly.8 A study9 comparing the periods 1990 to 1992 with 1992 to 1994 demonstrated a fivefold increase in the incidence of positional head deformity and found that all affected infants were supine sleepers.
Diagnosis
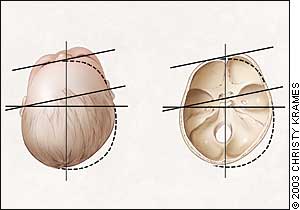
The physician should first determine whether the infant has synostotic plagiocephaly or positional head deformity, because the two conditions have very different clinical implications and treatments (Table 1). In most cases of synostotic plagiocephaly, a palpable ridge will form. The position of the ear also can be used to distinguish between these two causes: if the ear on the flattened side is located more posterior than the other ear, this is suggestive of synostotic plagiocephaly, and if the ear on the flattened side is located more anterior than the other ear, this is suggestive of positional head deformity. Positional head deformity produces more facial asymmetry than synostotic plagiocephaly, because of the forehead protruding on the side of the flattening (Figure 2).
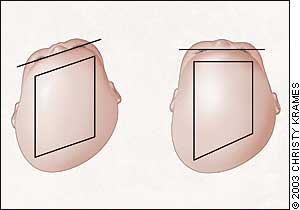
Physicians often measure the head circumference but fail to evaluate the shape of the head. Most infants will have a “bald spot” caused by sleeping in a supine position. If the bald spot is predominantly unilateral, the physician should palpate the occiput for significant flattening. Viewing the infant from an aerial view may show the typical “parallelogram” shape of positional head deformity (Figure 3).6 The physician should confirm that the infant's ears are in a similar position on each side of the head and that the line of the eyes is horizontal. If either of these facial features is different, a positional head deformity may be present.
| Prevention | ||
| Two-week well-child visit: Physician educates caregiver regarding prevention of PHD. | ||
| Two-month well-child visit: Physician assesses head shape and facial asymmetry, and makes further recommendations for PHD, if necessary. | ||
| Treatment | ||
| For characteristic PHD: | ||
| Refer to pediatric physical therapy: | ||
| (1) To educate the child's caregivers about PHD. | ||
| (2) To teach exercises to correct the shortened sternocleidomastoid muscle. | ||
| If PHD does not improve after four to eight weeks of physical therapy: | ||
| Confirm patency of sutures by radiography of the head and/or computed tomographic scan of the head with three-dimensional reconstruction. | ||
| Arrange for head orthosis (“helmet”) if patient sutures confirmed. | ||
Treatment
Early recognition of positional head deformity is crucial given the rapidly growing skull of an infant. As the child develops a preference for positioning, the ipsilateral sternocleidomastoid muscle shortens resulting in torticollis. This is in contrast to the infant with congenital torticollis in which the rotate and tilt of the head initiates the side preference and the occiput flattens correspondingly. Sleeping in the supine position and feedings always offered from the same side correlate with a positional head deformity.10 Physical therapy aims to educate the child's parents and caregivers about positional head deformity and to teach them exercises that will correct the shortening of the sternocleidomastoid muscle (Table 2). Pediatric physical therapists can teach caregivers how to carry the child to lengthen the sternocleidomastoid muscle, how to encourage prone playing, and how to alter eating positions to diminish the side preference.

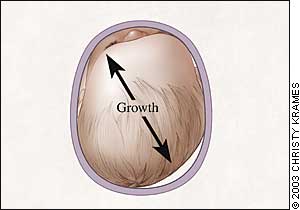
If the positional head deformity does not improve within the first four to eight weeks of physical therapy, the patency of the sutures should be confirmed by radiography of the head. If the sutures appear poorly visualized or closed, a computed tomographic (CT) scan of the head with three-dimensional reconstruction should be obtained.11 If the radiograph shows patent sutures but the child is not improving with therapy alone, a head orthosis (“helmet”), which is custom molded to the infant's head, may be needed (Figure 4). The skull undergoes 85 percent of its postnatal growth within the first year of life. The helmet alleviates the pressure on the flattened area of the occiput and allows the skull to grow faster in the desired directions (Figure 5). In a prospective series12 of 71 infants with positional head deformity studied from 1992 to 1995, one half of the infants improved with physical therapy and the others improved with the use of a head orthosis. The five infants who did not improve had hypotonia, developmental delay, or were referred later than six months of age.12
The long-term consequences of positional head deformity are controversial. A 1994 commentary by the AAP Task Force on Infant Sleeping Position and SIDS stated that: “the initial concern, that a shift away from prone sleeping might result in an increase in undesirable complications, has not materialized.”13 However, the increased incidence of positional head deformity from supine sleeping contradicts this statement. Although positional head deformity does not result in the loss of life, the emotional costs of the facial asymmetry may be high. Mild to severe cosmetic deformities persist in 10 percent of infants affected by positional head deformity.14 Flattening of the occiput remained in nearly one third of infants with positional head deformity who were followed for two to three years.10 One recent study14 suggests that infants with positional head deformity are at a higher risk for subtle developmental difficulties that present at elementary school-age. Finally, in treating the positional head deformity, the family of the child may acquire significant medical, emotional, and personal costs. Early recognition of positional head deformity is extremely important to initiate early intervention for treatment or referral of the infant.
Prevention of Positional Head Deformity
Prevention of positional head deformity is even more important than early recognition of the condition (Table 2). Prevention begins with educating the infant's caregiver. If minor skull flattening is noted during the two-month visit, the physician can encourage the caregiver to place the infant prone for supervised play. In one study,15 25 percent of parents never placed their infants prone, even for play. The prone position can be made more comfortable during play by placing toys in front of the child and having the caregiver join the infant on the floor. Infants may cry if they are not accustomed to the prone position. The caregiver can pick up the infant before they become very upset and then slowly increase the time the infant lies on his or her stomach. During feeding, the caregiver can approach the infant from the side opposite the flattened area to encourage head turning and lengthening of the sternocleidomastoid muscle. Caregivers should be discouraged from using a swing or car seat for prolonged sitting because a young infant cannot hold his head midline and will quickly develop an occipital preference.
If the cause of an abnormal skull shape is uncertain, referral to a pediatric neurosurgeon or craniofacial clinic is warranted. If the child develops a characteristic positional head deformity, the physician can refer the child to a pediatric physical therapist who is competent to treat the abnormality. If the infant does not improve rapidly with therapy, radiographic evaluation should be done, and a head orthosis should be considered (Table 2).