
Am Fam Physician. 2003;68(6):1135-1142
Pruritus is a common manifestation of dermatologic diseases, including xerotic eczema, atopic dermatitis, and allergic contact dermatitis. Effective treatment of pruritus can prevent scratch-induced complications such as lichen simplex chronicus and impetigo. Patients, particularly elderly adults, with severe pruritus that does not respond to conservative therapy should be evaluated for an underlying systemic disease. Causes of systemic pruritus include uremia, cholestasis, polycythemia vera, Hodgkin's lymphoma, hyperthyroidism, and human immunodeficiency virus (HIV) infection. Skin scraping, biopsy, or culture may be indicated if skin lesions are present. Diagnostic testing is directed by the clinical evaluation and may include a complete blood count and measurement of thyroid-stimulating hormone, serum bilirubin, alkaline phosphatase, serum creatinine, and blood urea nitrogen levels. Chest radiography and testing for HIV infection may be indicated in some patients. Management of nonspecific pruritus is directed mostly at preventing xerosis. Management of disease-specific pruritus has been established for certain systemic conditions, including uremia and cholestasis.
Pruritus is a common dermatologic problem that increases in incidence with age. In some patients, the condition may be so severe that it affects sleep and quality of life. While pruritus most commonly occurs in skin disorders, it may be an important dermatologic clue to the presence of an underlying systemic disease.
Pathophysiology
Pruritus originates within the skin's free nerve endings, which are most heavily concentrated in the wrists and ankles. The sensation of pruritus is transmitted through C fibers to the dorsal horn of the spinal cord and then to the cerebral cortex via the spinothalamic tract.1 Pruritus generates a spinal reflex response, the scratch, which is as innate as a deep tendon reflex.2 Regardless of the cause, pruritus often is exacerbated by skin inflammation, dry or hot ambient conditions, skin vasodilation, and psychologic stressors.3
A single mechanism cannot explain all causes of pruritus. Histamine, which is released by mast cells in persons with urticaria and other allergic reactions, classically is associated with pruritus. However, with the exception of allergic conditions, histamine must be considered only one of several chemical mediators of itch.
Serotonin appears to be a key component of the pruritus that occurs with several diseases, including polycythemia vera, uremia, cholestasis and lymphoma, and of morphine-associated pruritus. Serotonin inhibitors such as cyproheptadine (Periactin), pizotifen, paroxetine (Paxil), and ondansetron (Zofran) have proved effective in treating several of these pruritic conditions.2
The pruritus that occurs in herpes zoster prodrome may be a model for pruritus with a neuropathic cause. Certain idiopathic types of localized pruritus have been attributed to peripheral neuropathy. Brachioradial pruritus is an uncommon condition that presents as lateral arm pruritus and has been associated with spinal disease. Similarly, notalgia paresthetica is thought to be of neuropathic origin, with pruritus limited to the middle of the back. Severe pruritus also has been observed in patients with spinal tumors and multiple sclerosis.2,5,6
Atopic dermatitis appears to involve an immune-mediated release of cytokines and other pro-inflammatory agents, a mechanism analogous to airway hyperreactivity in patients with asthma.7–9 Superimposed on this hyperreactivity is a distorted touch sensation. Although patients without atopic dermatitis perceive mild mechanical stimulation as touch, patients with the condition perceive it as pruritus.8,10
Dermatologic Causes of Pruritus
XEROSIS
| Cause | Features |
|---|---|
| Allergic contact dermatitis | Sharply demarcated erythematous lesion with overlying vesicles |
| Reaction within two to seven days of exposure (see Table 2) | |
| Atopic dermatitis | “Itch that rashes (when scratched)” in patients with atopic conditions (e.g., allergic rhinitis, asthma) |
| Involvement of flexor wrists and ankles, as well as antecubital and popliteal fossae | |
| Bullous pemphigoid | Initially pruritic urticarial lesions, often in intertriginous areas |
| Formation of tense blisters after urticaria | |
| Cutaneous T-cell lymphoma (mycosis fungoides) | Oval eczematous patch on skin with no sun exposure (e.g., buttocks) |
| Possible presentation as new eczematous dermatitis in older adults | |
| Possible presentation as erythroderma (exfoliative dermatitis) | |
| Dermatitis herpetiformis | Rare vesicular dermatitis affecting lumbosacral spine, elbows, or knees |
| Folliculitis | Pruritus out of proportion to appearance of dermatitis |
| Papules and pustules at follicular sites on chest, back, or thigh | |
| Lichen planus | Lesions often located on the flexor wrists “6Ps”: pruritus, polygonal, planar, purple papules, and plaques |
| Pediculosis (lice infestation) | Occiput of school-aged children; genitalia in adults (sexually transmitted disease) |
| Psoriasis | Plaques on extensor extremities, low back, palms, soles, and scalp |
| Scabies | Burrows in hand web spaces, axillae, and genitalia |
| Hyperkeratotic plaques, pruritic papules, or scales | |
| Face and scalp affected in children but not in adults | |
| Sunburn teroidal | Possible photosensitizing cause (e.g., nonsteroidal anti-inflammatory drugs, cosmetics) |
| Xerotic eczema | Intense itching in elderly patients (often during winter months in northern climates) |
| Involvement of back, flank, abdomen, waist, and distal extremities |
Patients with xerosis experience an intense pruritus, usually involving the anterolateral lower legs. Other commonly involved areas include the back, flank, abdomen, and waist. Skin drying and scratching result in red plaques that fissure and whose appearance has been compared to that of cracked porcelain (eczema craquelé).
ATOPIC DERMATITIS
Atopic dermatitis can result in severe pruritus and is often described as “the itch that rashes (when scratched).” Atopic dermatitis affects 10 percent of children and often develops before six months of age.7,9 Atopic dermatitis often persists into adulthood and may be exacerbated during pregnancy. Patients with atopic dermatitis usually have a family history of asthma and allergic rhinitis.
In infants with atopic dermatitis, eczema usually involves the face, scalp, trunk, extensor arms, and legs. Older children and adults experience “hot and sweaty fossae and folds” involving flexor surfaces such as the antecubital and popliteal fossae, as well as the flexor wrists and ankles.8 Adults also may develop atopic dermatitis of the hands, upper eyelids, and anogenital region.
ALLERGIC CONTACT DERMATITIS
A careful history is important in patients with allergic contact dermatitis, another common cause of pruritus. Allergic contact dermatitis may be caused by exposure to substances such as nickel, latex, cosmetics, rhus oils (e.g., poison ivy), and topical medications such as benzocaine (Americaine) and neomycin (Table 2).2,11,13,14 Information on occupational causes of allergic contact dermatitis is available online (www.hazmap.com) and in a recent review.13
| Allergic contact dermatitis13 |
| Cosmetics, black hair dye |
| Latex |
| Laundry detergents, fabric softeners |
| Nickel |
| Ointments that are highly concentrated in inert oil |
| Paint-on tattoos (paraphenylenediamine), tattoo dye (cadmium yellow, mercuric sulfide [red]) |
| Rhus oil (e.g., poison ivy) |
| Topical medications: benzocaine (Americaine), neomycin |
| Heat exposure11 |
| Cholinergic urticaria (response to hot bath, fever, exercise) |
| Miliaria rubra (prickly heat) |
| Occupational exposure13 |
| Fiberglass |
| Glyceryl monothioglycolate (in permanent-wave solution) |
| Methyl methacrylate (e.g., Plexiglas) |
| Potassium dichromate in cements and dyes |
| Rosins or epoxy resins in adhesives |
| Rubber |
| Systemic medications11 |
| Antifungal agents: fluconazole (Diflucan), itraconazole (Sporanox), ketoconazole (Nizoral) |
| Aspirin |
| B vitamins, including niacinamide |
| Drug hypersensitivity: rifampin (Rifadin), vancomycin (Vancocin) |
| Nitrates (food preservatives) |
| Quinidine |
| Spinal narcotics (pruritus affecting face, neck, and upper chest) |
| Water exposure2,11,14 |
| Aquagenic pruritus (associated with polycythemia vera, itching within 15 minutes of any water contact) |
| Cholinergic urticaria (response to warm water) |
| Polycythemia vera |
| Swimmer's itch (seven-day eruption after freshwater swimming) |
Like xerosis and atopic dermatitis, allergic contact dermatitis is an eczematous reaction, but the reaction is localized to allergen-exposed areas. It can be difficult to distinguish allergic contact dermatitis from irritant contact dermatitis, which is often a reaction to the frequent use of concentrated organic solvent or soap. However, allergic contact dermatitis tends to develop rapidly, and the lesions have more distinct borders than those of irritant contact dermatitis.
SCABIES OR LICE
Pruritus may be the chief complaint in patients with scabies or lice. In contrast to the pathognomonic burrows within the hand web spaces, axillae, and genitalia, nonspecific pruritic papules may be the only sign of scabies. Despite careful examination by the keenest of eyes, physicians have historically misdiagnosed the surreptitious spread of the scabies mite.15
Systemic Causes of Pruritus
Pruritus can be an important dermatologic clue to the presence of significant underlying disease in 10 to 50 percent of older adults.16 Systemic causes must be considered, especially in elderly patients in whom pruritus is persistent and refractory to xerosis management and other nonspecific therapies.12,17
Pruritus has been associated with a wide variety of systemic conditions (Table 3).1–3,6,11,18–27 In up to 30 percent of patients, the diagnosis of Hodgkin's lymphoma is preceded by intense, chronic, generalized pruritus.21 Pruritus also may be a presenting feature in patients with cutaneous T-cell lymphoma.28 Patients with human immunodeficiency virus (HIV) infection commonly have itching, which is most often considered secondary to comorbid dermatologic conditions such as xerosis, seborrheic dermatitis, candidiasis, psoriasis, scabies, or eosinophilic folliculitis.20 Uremia causes severe paroxysms of pruritus (especially during the summer) in 25 percent of patients with chronic renal failure and 86 percent of patients who are receiving hemodialysis.29
| Cause | Features | |
|---|---|---|
| Cholestasis18,19 | Intense itching (hands, feet, pressure sites) that becomes worse at night | |
| Reactive hyperpigmentation that spares the middle of the back (butterfly-shaped dermatitis) | ||
| Chronic renal failure | Severe paroxysms of generalized itching, worse in summer | |
| Delusions of parasitosis | Focal erosions on exposed areas of arms and legs | |
| Hodgkin's lymphoma21 | Prolonged generalized pruritus often preceding diagnosis | |
| Human immunodeficiency virus infection20 | A common presenting symptom resulting from secondary causes (eczema, drug reaction, eosinophilic folliculitis, seborrhea) | |
| Hyperthyroidism22,23 | Warm, moist skin; possibly, pretibial edema | |
| Associated conditions: onycholysis, hyperpigmentation, vitiligo | ||
| Iron deficiency anemia24 | Signs in addition to pruritus: glossitis, angular cheilitis | |
| Malignant carcinoid | Intermittent head and neck flushing with explosive diarrhea | |
| Multiple myeloma | In elderly patients: bone pain, headache, cachexia, anemia, renal failure | |
| Neurodermatitis or neurotic excoriations25 | Bouts of intense itching that may awaken patients from sound sleep | |
| Involvement of scalp, neck, wrist, extensor elbow, outer leg, ankle, and perineum | ||
| Parasitic infections | Usually in returning travelers or immigrants | |
| Filariasis | Tropical parasite responsible for lymphedema | |
| Schistosomiasis | Freshwater exposure in Africa, the Mediterranean area, or South America | |
| Onchocerciasis | Transmitted by black fly in Africa or Latin America | |
| Trichinosis | Ingestion of undercooked pork, bear, wild boar, or walrus meat | |
| Parvovirus B19 infection | “Slapped cheek” appearance in children; arthritis in some adults | |
| Peripheral neuropathy | ||
| Brachioradial pruritus | Involvement of lateral arm in white patients who have traveled to the tropics6 | |
| Herpes zoster | Pruritus accompanying painful prodrome two days before appearance of rash | |
| Notalgia paresthetica | Pruritus in middle of back with hyperpigmented patch2 | |
| Polycythemia rubra vera26 | Pricking-type itch persisting for hours after hot shower or bath | |
| Scleroderma | Nonpitting extremity edema, erythema, and intense pruritus | |
| Edema phase with pruritus occurring before fibrosis of skin | ||
| Urticaria | Response to allergen, cold, heat, exercise, sunlight, or direct pressure | |
| Weight loss (rapid) in eating disorders27 | Signs in addition to pruritus: hair loss, fine lanugo hair on back and cheeks, yellow skin discoloration, petechiae | |
Along with uremia, cholestasis is responsible for some of the most intense itching. Cholestasis-related pruritus is most severe at night, with a predilection for the hands and feet. Hyperpigmentation may result in areas of heavy scratching. In patients with hyperpigmentation, the middle of the back is spared, resulting in a classic butterfly-shaped dermatitis.2 Cholestasis may be caused by numerous medications, including oral contraceptive pills, erythromycin, amoxicillin–clavulanate potassium (Augmentin), phenothiazines, and anabolic steroids.
| Cause | Features |
|---|---|
| Pruritic urticarial papules and plaques of pregnancy (common in third trimester) | Intense pruritus involving abdomen, with spread to thighs, buttocks, breasts, and arms |
| Prurigo of pregnancy (common in second half of pregnancy) | Associated with atopic dermatitis |
| Excoriated papules and nodules on extensor arms and abdomen | |
| Herpes gestationis or pemphigoid gestationis (uncommon) | Autoimmune condition associated with Graves' disease |
| Vesicles and bullae on abdomen and extremities in second half of pregnancy | |
| Responsive to prednisone (dosage: 20 to 40 mg per day)33 | |
| Intrahepatic cholestasis of pregnancy (uncommon) | Trunk and extremity itching without rash in late pregnancy |
| No jaundice in mild form | |
| Responsive to cholestyramine (Questran) and vitamin K130 | |
| Pruritic folliculitis of pregnancy (uncommon, occurs in second half of pregnancy) | Erythematous follicular papules over trunk, with spread to extremities |
| Possibly a variant of prurigo of pregnancy | |
| Other common pruritic conditions exacerbated in pregnancy | Atopic dermatitis, allergic contact dermatitis |
Evaluation of Pruritus
A thorough history and a complete physical examination are central to the evaluation of pruritus. Most pruritic conditions can be diagnosed on the basis of the presence of associated dermatitis, the distribution of the itching or rash, or a history of recent exposure to exogenous causes.
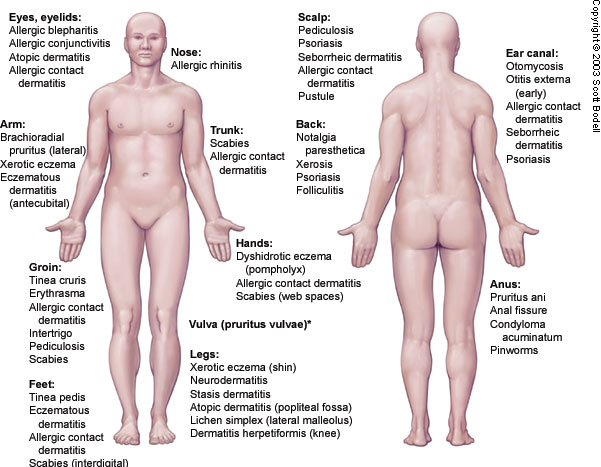
Reassuring factors that suggest a nonsystemic or exogenous cause include acute onset over several days, localized pruritus, limitation of pruritus to exposed skin, presence of pruritus in other household members, or a history of recent travel or occupational exposure.2 The distribution of the pruritus may narrow the list of potential causes significantly or may be pathognomonic for certain conditions, such as scabies with its associated interdigital web-space itch2,34–36 (Figure 1).
A careful skin examination is critical, particularly in older adults. Lack of dermatologic findings in older patients with pruritus compels a more vigorous search for underlying systemic disease. Skin scrapings can identify scabies and dermatophytoses. Skin biopsy may be useful in ruling out more suspicious skin lesions suggestive of mastocytosis, mycosis fungoides, or bullous pemphigoid. The physical examination also should include careful palpation of the lymph nodes, liver, and spleen.
Management of Pruritus
NONSPECIFIC THERAPY
Nonspecific treatment measures generally are useful in alleviating atopic dermatitis and xerosis, but they also may be effective in many other types of pruritus (Table 5).2–4,7,9,10,37 Skin lubricants should be applied frequently during the day and immediately after bathing. Patients should avoid excessive bathing, frequent use of soap, dry environments, topical irritants (e.g., synthetic or wool clothing, topical anesthetics), and vasodilators (e.g., caffeine, alcohol, exposure to hot water).8,10
| Use skin lubricants liberally: petrolatum or lubricant cream at bedtime; alcohol-free, hypoallergenic lotions frequently during the day. | |
| Decrease frequency of bathing and limit bathing to brief exposure to tepid water; after bathing, briefly pat skin dry and immediately apply skin lubricant. | |
| Use mild, unscented, hypoallergenic soap two to three times per week; limit daily use of soap to groin and axillae (spare legs, arms, and torso). | |
| Humidify dry indoor environment, especially in winter. | |
| Choose clothing that does not irritate the skin (preferably made of doubly rinsed cotton or silk); avoid clothing made of wool, smooth-textured cotton, or heat-retaining material (synthetic fabrics); when washing sheets, add bath oil (e.g., Alpha Keri) to rinse cycle. | |
| Avoid use of vasodilators (caffeine, alcohol, spices, hot water) and excessive sweating. | |
| Avoid use of provocative topical medications, such as corticosteroids for prolonged periods (risk of skin atrophy) and topical anesthetics and antihistamines (may sensitize exposed skin and increase risk of allergic contact dermatitis). | |
| Prevent complications of scratching by keeping fingernails short and clean, and by rubbing skin with the palms of the hands if urge to scratch is irresistible. | |
| Treatments: | |
| Standard topical antipruritic agents: menthol and camphor (e.g., Sarna lotion), oatmeal baths (e.g., Aveeno), pramoxine (e.g., PrameGel), calamine lotion (Caladryl; use only on weeping lesions, not on dry skin), doxepin 5% cream (Zonalon) | |
| Topical antipruritic agents for refractory pruritus (e.g., severe atopic dermatitis): Burrow's solution (wet dressings), Unna's boot, tar emulsion | |
| Systemic antipruritic agents (used in allergic and urticarial disease): doxepin (Sinequan), 10 to 25 mg at bedtime4; hydroxyzine (Atarax), 25 to 100 mg at bedtime; nonsedating antihistamines (e.g., fexofenadine [Allegra])37 | |
MEDICATIONS
Antihistamines may be beneficial in the treatment of urticaria and other allergic causes of pruritus.37 However, other than providing nighttime sedation to assist sleep, antihistamines are not uniformly effective in treating all causes of pruritus.38 Antihistamines also may provoke adverse effects related to sedation and anticholinergic properties, particularly in elderly patients.12
TREATMENT OF SYSTEMIC CAUSES
Management of pruritus should be directed at the underlying cause. In patients with pruritus that has a systemic cause (e.g., hyperthyroidism,22,23 iron deficiency anemia,24 Hodgkin's lymphoma, HIV infection20), itching gradually recedes as the primary condition improves. Although a full discussion of treatment is beyond the scope of this article, specific management strategies for uremic and cholestatic pruritus, as well as other systemic pruritic conditions, are included in Table 6.2,4,18,19,25,26,29
| Cholestasis2,18,19 |
| Cholestyramine (Questran), 4 to 6 g orally 30 minutes before meals |
| Ursodiol acid (Actigall), 13 to 15 mg per kg per day orally |
| Ondansetron (Zofran), 4 to 8 mg IV, then 4 mg orally every eight hours |
| Opiate receptor antagonist such as nalmefene (Revex), 20 mg orally two times per day |
| Rifampin (Rifadin), 300 mg orally twice daily |
| Bile duct stenting for extrahepatic cholestasis |
| Bright-light therapy |
| Neurotic excoriation4,25 |
| Pimozide (Orap) orally for delusions of parasitosis |
| Selective serotonin reuptake inhibitor (e.g., fluvoxamine [Luvox], fluoxetine [Prozac], paroxetine [Paxil]) |
| Notalgia paresthetica2 |
| Capsaicin 0.025% cream (Zostrix) applied to localized areas four to six times daily for several weeks |
| Polycythemia vera26 |
| Aspirin, 500 mg orally every eight to 24 hours |
| Paroxetine (Paxil), 10 to 20 mg orally per day |
| Interferon alfa, 3 to 35 million IU per week |
| Spinal opioid–induced pruritus2 |
| Ondansetron, 8 mg IV, concurrent with opioid |
| Nalbuphine (Nubain), 5 mg IV, concurrent with opioid2 |
| Uremia2,29* |
| Ultraviolet B phototherapy two times per week for one month |
| Activated charcoal, 6 g per day orally |
| Capsaicin 0.025% cream applied to localized areas four to six times daily for several weeks |
Complications of Pruritus
Complications arise when pruritus is accompanied by intense scratching. Lichen simplex chronicus is a localized skin thickening, often appearing over the posterior neck, extremities, scrotum, vulva, anus, and buttocks. In prurigo nodularis, a variant of lichen simplex chronicus, 10- to 20-mm nodules develop over areas within easy scratching reach, such as the extensor arms and legs.11 Prurigo nodularis has been successfully treated with a cream containing 0.025 percent capsaicin (Zostrix) applied topically four to six times per day for two to eight weeks).39 [Evidence level B, nonrandomized clinical studies] Impetigo may result from superinfected excoriations, as commonly occur in patients with atopic dermatitis.7,9
Insomnia, which is a common concern for many older adults, is further exacerbated by pruritus. Lack of sleep may significantly affect quality of life; it can also increase the risk of accidents and injuries, and result in a worsening of comorbid conditions.12