
Am Fam Physician. 2003;68(10):1983-1987
The breast mass is a clinical problem commonly encountered by family physicians. Fine-needle and core biopsy techniques require training and cytopathologist support. In contrast, breast cyst aspiration using a 21- or 22-gauge needle is a simple, cost-effective, minimally invasive procedure. The technique is easy to learn and can be practiced on a breast model. Breast cyst aspiration may be attempted in many women who present with a palpable, dominant breast mass. If clear fluid is aspirated and the mass resolves, malignancy is unlikely, and breast cyst is the probable diagnosis. In this situation, reevaluation in four to six weeks is appropriate; if the cyst has not recurred, only routine mammographic surveillance is required. Referral for fine-needle or excisional biopsy is indicated if the aspirate is bloody or extremely tenacious, if no fluid can be aspirated, or if there is residual mass after aspiration. Complications such as local discomfort, bruising, and infection are uncommon.
Breast lumps are a problem for which women commonly consult family physicians.1 Although fine-needle biopsy is not difficult to learn, additional training and adequate cytopathologist support are required. Consequently, family physicians frequently do not offer this procedure, and referral for surgical biopsy is necessary. The resultant delay in determining whether a mass is benign or malignant increases patient anxiety.
Breast cyst aspiration is a simple, easily mastered procedure in which a needle and syringe are used to drain and diagnose a presumed breast cyst. Differentiation of a cyst by this technique may reduce the waiting time for diagnosis in select patients. Breast cyst aspiration is a safe, well-tolerated, and timely diagnostic procedure that family physicians may be able to offer women who present with a new breast mass.
Patient Selection
Breast cysts usually form because of obstruction, involution, or aging of ducts within the breast. These masses are usually well circumscribed and mobile; on palpation, they can be tender.
Cysts are a common cause of palpable breast masses in premenopausal women older than 40 years. They are relatively uncommon in postmenopausal women who are not receiving hormone therapy.2 In women younger than 40 years, fibroadenomas and other solid benign lesions are the most likely cause of newly discovered dominant breast lumps.
It often is difficult to differentiate cystic from solid lesions by physical examination alone. Ultrasonography or mammography can help, but performance of either study involves a time delay and another appointment for the patient. Thus, breast cyst aspiration is an appropriate first step in the care of women who present with a dominant breast mass suspected of being a cyst.3 [Evidence level C, consensus expert guidelines]
Breast Cyst Aspiration Technique
Potential complications should be discussed with the patient and informed consent obtained before the procedure is performed.
EQUIPMENT
Breast cyst aspiration requires minimal equipment: povidone-iodine solution, alcohol swabs, sterile drapes, sterile gloves, a 21- or 22-gauge needle with a semiopaque needle hub, a 5-mL syringe or specialized cyst aspirator syringe, and a plastic strip bandage.
SITE PREPARATION
The breast mass should be located and the area cleansed with povidone-iodine solution, followed by an alcohol swab. To reduce the risk of postprocedure infection, sterile drapes should be placed around the site, and sterile gloves should be worn.
Local (skin) anesthesia generally is not needed for simple breast cyst aspiration. The procedure itself requires only one needle stick, rather than the multiple sampling sticks used in fine-needle biopsy.
PROCEDURE
The 21- or 22-gauge needle is attached to the syringe. A small amount of air is suctioned into the syringe to break the seal.
The mass is immobilized between the index and middle fingers of the nondominant hand (Figure 1, top). To reduce the remote risk of pneumothorax, a rib may be palpated, the mass may be moved to lie over the rib, and the rib may be used as a guard before aspiration is performed.
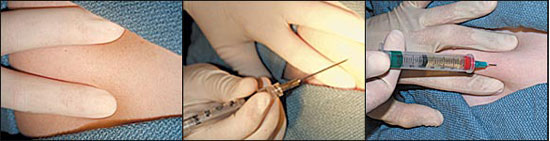
The syringe is held like a pencil by the dominant hand while the needle is inserted into the center of the mass (Figure 1, center). The fingers of the dominant hand slowly walk up the syringe, and the thumb pulls the plunger up to aspirate the contents of the cyst (Figure 1, bottom). In the case of a “dry tap” (i.e., no fluid is aspirated), needle placement should be adjusted to ensure that the cyst was not missed.
Once the mass has been aspirated, pressure on the plunger is released, and the needle is withdrawn. The risk of hematoma formation can be decreased by applying local pressure at the aspiration site once the needle has been removed. The biopsy site is then covered with a plastic strip bandage.
EVALUATION OF ASPIRATE
Cystic fluid is seldom colorless. It is typically white, yellow-green, brown, or frankly bloody. If the fluid is nonbloody and watery, and the mass completely disappears with aspiration, the fluid can be discarded, and the patient can be reassured that the mass was cystic. Routine examination of watery, non-bloody cystic fluid is not indicated.3,4 [Reference3—Evidence level C, consensus/expert guidelines; reference4—Evidence level B, descriptive study]
Surgical or radiologic referral is necessary if no fluid is aspirated, the aspirated fluid is bloody or unusually tenacious, or there is residual mass. A physician trained in fine-needle biopsy techniques may proceed to sample a solid mass and send the sample for immediate evaluation. Bloody aspirate should be sent to the laboratory for evaluation, but additional biopsy will be needed.
Management and Follow-up
Breast cyst aspiration is a diagnostic procedure that is potentially therapeutic if a watery, nonbloody aspirate is obtained and the cyst resolves completely. However, follow-up is imperative, because the false-negative rate for the procedure may be as high as 15 to 20 percent.5 With appropriate follow-up, the false-negative rate becomes negligible.6
Further evaluation is required for breast cysts that remain palpable after aspiration, contain bloody or unusually tenacious fluid, or subsequently refill. In these situations, patients should be referred for biopsy, even if the mammogram is normal.3,6 [Reference3—Evidence level C, consensus/expert opinion; reference6—Evidence level B, observational study]
In summary, after-care and follow-up include the following3:
Palpation of the cyst after aspiration to ensure complete resolution.
Reevaluation of the patient in four to six weeks to be certain that the cyst has not refilled.
Referral of the patient for surgical biopsy if there is refilling or residual mass.
Possible complications of the breast cyst aspiration technique include discomfort at the aspiration site, bruising, localized infection, small hematoma formation and, rarely, pneumothorax. No evidence shows that aspiration of a breast carcinoma spreads cancer cells or worsens survival.7
Breast cyst aspiration does not appear to increase the number of false-positive mammograms as long as the mammographer has information about the exact location of the aspiration.8,9 The sensitivity (79 percent) and specificity (94 percent) of mammography performed within two weeks of fine-needle biopsy are similar to those of routine screening.8,9 Similar sensitivity and specificity may be expected for mammography performed after breast cyst aspiration.
Breast Model
A breast model can be used to practice breast cyst aspiration technique.10 In addition to a 21- or 22-gauge needle with a semi-opaque needle hub and a 5-mL syringe or specialized cyst aspirator syringe, required equipment includes two balloons, one cup of flour, and one or two bath beads or vitamin E capsules.
Two balloons are hand stretched or are filled with air and then deflated. The end of one balloon is cut, and the balloon is filled with one cup of flour. One or two bath beads or vitamin E capsules are placed in the flour to become the “cyst.” The second balloon is stretched over the first balloon to seal in the flour.
Using the previously described breast cyst aspiration technique, the physician can practice localizing the “cyst” with the nondominant hand and holding the syringe like a pencil in the dominant hand. If the needle is placed correctly, oil will be drawn into the syringe. If needle placement is incorrect, flour will be drawn into the syringe.