
Am Fam Physician. 2004;69(4):919-921
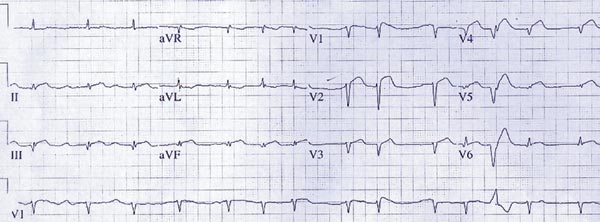
A 67-year-old woman with a mechanical mitral valve presented to the emergency department with fever for two days, a sudden onset of crushing, substernal chest pain, and this electrocardiograph (ECG) reading (Figure 1). Of note, she had been admitted to the hospital one month earlier for evaluation of a transient ischemic attack (TIA), which manifested as right arm weakness and numbness. A head computed tomography scan during that admission was normal, and a transthoracic echocardiogram showed a normally functioning mechanical mitral valve, which had been placed two years earlier. Review of her anticoagulation monitoring revealed that all recent international normalized ratio measurements were within the therapeutic range.
Question
Discussion
The correct answer is B: prosthetic valve endocarditis with coronary embolization. The quality and sudden onset of the patient's chest pain, in combination with the ECG findings of anterolateral and inferior ST elevations, strongly suggested an acute myocardial infarction. The history of a recent TIA raised the possibility of a previous embolic event. The patient was taken emergently to cardiac catheterization, which revealed 100 percent occlusion of the distal left anterior descending artery but otherwise normal coronary arteries. Attempts to reduce the thrombus via angioplasty resulted in distal migration of the blockage, suggesting an embolic etiology. Transesophageal echocardiogram was performed, revealing a 3-cm vegetation on the anterior portion of the mitral valve (Figure 2). During emergent surgery to replace the prosthetic valve, large vegetations adherent to the valve were seen (Figure 3).
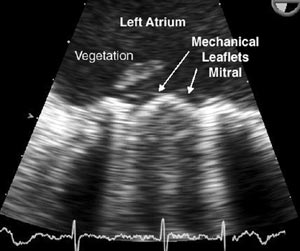
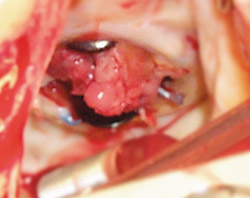
Endocarditis is a feared complication of prosthetic valve implantation, involving 1 to 4 percent of all prosthetic valves.3 Transthoracic echocardiogram has poor sensitivity (less than 60 percent) in detecting valve vegetations, and in this case, may have missed a vegetation that caused the patient's TIA one month earlier.4,5
Thrombotic acute myocardial infarction represents the most common cause of acute myocardial infarction in the United States. While this patient did experience a myocardial infarction, the preceding TIA and presence of a mechanical valve are important clues, raising the possibility of an embolic source of infarction.
Prosthetic heart valve failure may be chronic, subacute, or acute. Chronic or subacute failure of the mitral valve typically would lead to pulmonary edema, presenting with fatigue, dyspnea on exertion, and auscultation of crackles at the lung bases. Acute mitral valve failure leads to more sudden and severe pulmonary edema, characterized by marked shortness of breath, cardiogenic shock, and respiratory failure. Valve failure typically would not present with the crushing, substernal chest pain noted in this patient.
Aortic dissection usually presents with tearing chest pain that radiates to the back. An ascending dissection occasionally can occlude the ostium of a coronary artery and lead to myocardial infarction. The previous TIA and mechanical valve in this case make the rare likelihood of an embolic source for the myocardial infarction somewhat more likely than the even more rare chance of an ascending dissection. Emergent angiography would provide helpful information in arriving at a diagnosis.
Pericarditis does not present with crushing, substernal chest pain. Though it may lead to ST-segment elevation, this usually can be differentiated from ischemia by its more widespread distribution and the tendency for the elevated ST segment to retain some of its usual concavity, unlike the convex, dome-shaped elevations seen with ischemia.