
Am Fam Physician. 2005;72(12):2430-2436
to the editor: Posterior reversible encephalopathy syndrome (PRES) is a clinicoradiologic entity with headaches, visual disturbances, and seizures that can be misdiagnosed easily. PRES is diagnosed by an acute to subacute neurologic presentation and posterior transient changes on neuroimaging, with areas of vasogenic edema1 detected by diffusion-weighted magnetic resonance imaging (MRI), which provides prognostic information that guides therapeutic decisions and provides a teaching point. PRES is characterized by reversible white matter lesions; however, ischemic injury with irreversible damage may occur. The prompt control of blood pressure or discontinuation of the offending medication leads to the reversal of the clinical and radiologic abnormalities. When unrecognized, irreversible cytotoxic edema may occur.2
We report a patient with new onset of seizures with accelerated hypertension. MRI showed characteristic abnormalities of PRES. Aggressive management of blood pressure resulted in complete resolution of clinical and radiologic findings.
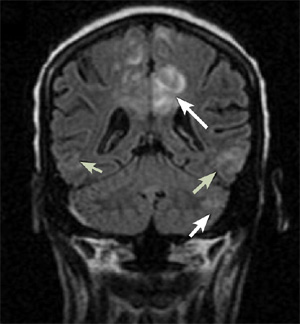
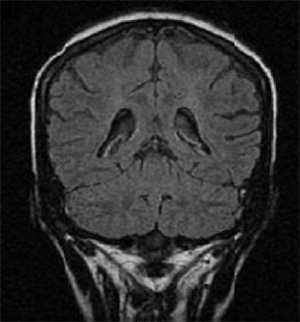
A 19-year-old woman with hypertension, systemic lupus erythematosus, and end-stage renal disease with hemodialysis, was admitted for acute onset of generalized tonic-clonic seizures with postictal confusion. She was receiving prednisone, hydrochloroquine (Plaquenil), cyclophosphamide (Cytoxan), and antihypertensives. Neurologic examination was normal without focal deficits. Her blood pressure was 180s/110s mm Hg, complete blood count was normal, electrolytes showed elevated blood urea nitrogen and creatinine, and cerebrospinal fluid and computed tomography of the head were normal. Electroencephalography showed diffuse slowing without epileptiform discharges. A brain MRI showed abnormal T2 signal, predominantly in the white matter of the posterior temporal, occipital, and parietal lobes, without abnormal enhancement (Figure 1). Diffusion-weighted images (DWIs) showed increased signal in these areas. She was treated with antihypertensives and hemodialysis. Her symptoms resolved in two days. Follow-up brain MRI revealed complete resolution of the increased T2 signals on fluid-attenuated inversion recovery (Figure 2) and DWI.
PRES is not a single disease entity but a clinicoradiologic syndrome with a multitude of clinical disorders including hypertensive encephalopathy, renal disease, seizures, vasculitis-like systemic lupus erythematosus, and many more.
The main cause of PRES is acute elevation of blood pressure above the upper limit of cerebral blood flow autoregulation.3 Diagnosing PRES has important therapeutic implications because of its potential reversibility. Clinical findings can mimic neuroradiologic conditions such as stroke and vasculitis.4 Clinical and neuroradiologic features are typically indistinguishable among cases of PRES, regardless of the underlying cause.
Neuroimaging findings often are characteristic; they may be the first clues to the diagnosis. Typical lesions predominate in the posterior white matter, with some involvement of the overlying cortex, and are hyperintense on T2-weighted images and DWI5 without any decreased signal on the apparent diffusion coefficient map, indicating vasogenic edema.
PRES may be suspected on the basis of history, but clinical signs and symptoms are nonspecific. Recognizing characteristic image findings is the key to diagnosing this syndrome and preventing deleterious work-ups or therapies. MRI with diffusion-weighted sequences and apparent diffusion coefficient values can reliably distinguish between vasogenic and cytotoxic edema and be used to predict conversion to infarction and irreversible tissue damage. Studies combining DWI and perfusion-weighted imaging may shed additional light on the pathophysiology of PRES.