
Am Fam Physician. 2007;76(1):86-89
Patient information: See related handout on Dupuytren's disease, written by the authors of this article.
Author disclosure: Nothing to disclose.
Dupuytren's disease is a progressive condition that causes the fibrous tissue of the palmar fascia to shorten and thicken. The disease is common in men older than 40 years; in persons of Northern European descent; and in persons who smoke, use alcohol, or have diabetes. Patients present with a small, pitted nodule (or multiple nodules) on the palm, which slowly progresses to contracture of the fingers. The disease initially can be managed with observation and non-surgical therapy. It will regress without treatment in approximately 10 percent of patients. Steroid injection into the nodule has been shown to reduce the need for surgery. Surgical referral should be made when metacarpophalangeal joint contracture reaches 30 degrees or when proximal interphalangeal joint contracture occurs at any degree. Timing of surgical intervention varies, but surgery is usually performed when the metacarpophalangeal joint contracture exceeds 40 degrees or when the proximal interphalangeal joint contracture exceeds 20 degrees. In-office percutaneous needle aponeurotomy is an alternative to surgery.
Dupuytren's disease is the shortening and thickening of ligaments that anchor skin to the palmar fascia. The disease initially presents as a firm nodule (or multiple nodules) on the palm of the hand proximal to the metacarpophalangeal (MCP) joint. Patients usually have difficulty with tasks such as face washing, hair combing, and putting their hands in their pockets.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Surgery should be performed in patients with Dupuytren's disease when the metacarpophalangeal joint contracture exceeds 40 degrees or when the proximal interphalangeal joint contracture exceeds 20 degrees. | B | 2, 3, 12 |
| Steroid injections into grade 1 Dupuytren's disease nodules can reduce the need for surgery. | B | 16 |
Clinical Presentation
Dupuytren's disease can be distinguished from other causes of hand contracture because it begins as a nodule and slowly progresses to contracture of the fingers. During the physical examination, physicians should note the site of the nodule and the presence of contractures; bands; and skin pitting, tenderness, and dimpling.
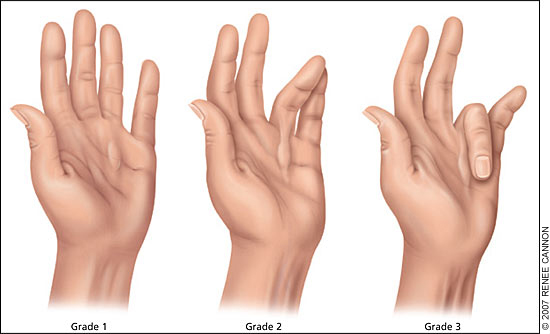
If contractures are present, the angles should be noted at the MCP and proximal interphalangeal (PIP) joints. A functional history and rate of progression also should be noted.1 The Hueston tabletop test can help with the diagnosis. If a patient is unable to lay his or her palm f lat on a tabletop, the test is positive. Disease progression is classified using a grading system (Figure 1). Grade 1 disease presents as a thickened nodule and a band in the palmar aponeurosis; this band may progress to skin tethering, puckering, or pitting. Grade 2 presents as a peritendinous band, and extension of the affected finger is limited. Grade 3 presents as f lexion contracture.2
Bilateral involvement is common, although one hand is usually more severely involved than the other; the patient's dominant hand is not a predictor of severity.3 The fingers most commonly involved (in decreasing order) are the fourth, fifth, third, and second. Soft tissue tumors of the palm and digits may be confused with Dupuytren's disease.3
Clinical Associations
Studies have identified Dupuytren's disease in persons of all racial groups,5–7 but the highest prevalence has been seen in northern Scotland, Iceland, Norway, and Australia.3 Evidence suggests an autosomal dominant pattern of inheritance with incomplete penetrance.8 Dupuytren's disease is more common in men and usually presents after 40 years of age.
There is a strong association between diabetes and Dupuytren's disease. Studies have found a 3 to 33 percent prevalence of Dupuytren's in patients with diabetes3,9; however, these patients tend to have a mild form of Dupuytren's with slow progression.3 Greater alcohol intake per week is associated with increased risk of Dupuytren's disease, but most patients with the disease are not alcoholics.3 Smoking also increases the risk of the disease.10 Although the reason for this association is unclear, microvascular changes in smokers may play a role.10
Other associations, such as trauma or epilepsy, are not well defined.3 Although trauma has been reported as a cause of Dupuytren's disease, studies have had mixed results.3,5,7,11 A connection between epilepsy and Dupuytren's disease has been reported,12 and some symptoms (e.g., palmar cords, knuckle pad thickening) have been shown to regress when anticonvulsant medications are discontinued.3 However, more recent, large cohort studies have not found an association between the disease and epilepsy or the use of epilepsy medication.11,13
Treatment
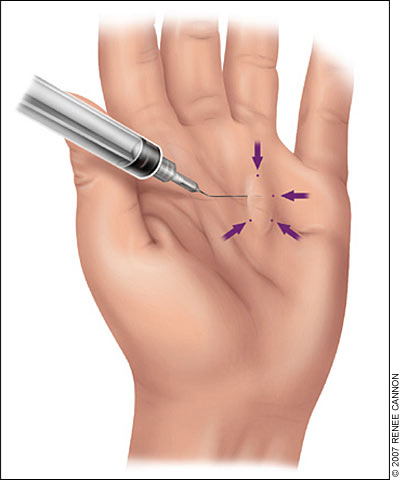
Grade 1 disease initially can be managed expectantly, but injecting the nodule with a steroid (Table 1 and Figure 2) can be helpful. Surgery is recommended if function is impaired, contracture is progressing, or severe deformity is disabling. Referral to a hand surgeon is indicated if the MCP joint contracture reaches 30 degrees or if PIP joint contracture occurs at any degree.2 The Hueston tabletop test is a good indication for referral. Timing of surgical intervention varies, but surgery is usually performed when the MCP joint contracture exceeds 40 degrees or when the PIP joint contracture exceeds 20 degrees.2,3,12
| Supplies |
| Lidocaine 2% (Xylocaine) |
| Triamcinolone acetonide (Kenalog; 40 mg per mL) |
| 21- and 25-gauge needles on 3-mL syringes |
| Povidone-iodine solution |
| Gauze |
| Bandage |
| Procedure |
| Clean the area with povidone-iodine solution |
| Using a 25-gauge needle, inject 1 to 2 mL of lidocaine 2% into the nodule (proximal to and along the sides of the nodule) |
| Using a 21-gauge needle, inject 2 to 3 mL triamcinolone acetonide (depending on size of nodule) into the nodule perpendicular to the axis of the digit; make injections in a star pattern |
| If it is difficult to access the nodule, use forceps to bend the needle by 45 degrees (see Figure 2) |
| Clean the area and apply dressing |
PIP joint contractures are more likely to cause stiffness and less likely to respond to surgery if more severe.14 The longer a deformity is present, the greater the risk of an irreversible joint contracture.
Surgery is usually successful, but recurrence is common.2 Percutaneous needle aponeurotomy of the nodule is an alternative to surgery.15 The in-office fasciotomy procedure includes a percutaneous needle technique using local anesthesia; it is performed more often in Europe than in the United States.15
A study showed that injections with tri-amcinolone acetonide (Kenalog) monthly for up to five months, or every six weeks for up to three injections, followed by a six-month respite, lead to significant disease regression.16 In the study, an average of 3.2 injections per nodule was needed for improvement of the nodule and hand function.16 Surgery was needed in fewer patients who received injections than would be anticipated in patients receiving expectant management alone.16 Possible complications of the procedure include tenderness, transient depigmentation, or atrophy at the injection site and rupture of the flexor tendon (more likely after repeated injections).16
No study has evaluated the effects of smoking cessation, decreased alcohol use, or diabetes control in patients with Dupuytren's disease. Patients requiring surgery have an increased overall and cancer-related mortality risk,17 probably secondary to smoking, alcohol use, and diabetes.