
Am Fam Physician. 2007;76(1):99-106
Author disclosure: Nothing to disclose.
This article provides answers to many questions medical students ask about the specialty of family medicine. It was developed through the collaborative efforts of several family medicine organizations, including the American Academy of Family Physicians, the Society of Teachers of Family Medicine, the Association of Family Medicine Residency Directors, and the Association of Departments of Family Medicine. The article discusses the benefits of primary care and family medicine, the education and training of family physicians, the scope of medical practice in the specialty, and issues related to lifestyle and medical student debt.
When considering their future specialty, many medical students have questions about family medicine. This article provides answers to the most common of these questions. It is the fifth update of a previous article and was developed through the collaborative efforts of several family medicine organizations, including the American Academy of Family Physicians (AAFP), the Society of Teachers of Family Medicine (STFM), the Association of Family Medicine Residency Directors (AFMRD), and the Association of Departments of Family Medicine (ADFM).1
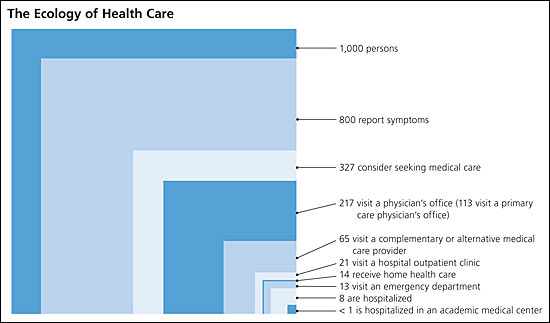
Physicians specializing in family medicine deliver primary care in the United States and around the world. Fifty percent of the care provided in the outpatient setting is delivered by primary care physicians (Figure 1).2 Students who choose a career in family medicine become part of the foundation of the health care system, establishing long-term relationships with patients and their family members and providing more than 90 percent of the health care that patients need throughout their lives.3 It is this close relationship between physician and patient over time that both patients and physicians say they value most.4
Why is family medicine/primary care important?
The lack of a primary care focus in the U.S. health care system has resulted in poorer health outcomes for Americans compared with persons in other industrialized countries.5 In a comparison with other developed countries, the United States ranked lowest in primary care functions and in health care outcomes despite having the highest level of health care spending.6–9
Several decades of accumulated evidence shows that a health system that focuses on primary care is more effective, more efficient, and more equitable. These benefits are demonstrated by reduced all-cause mortality rates,10 less frequent use of emergency departments and hospitals,11,12 better preventive care,13–15 improved detection of and reduction in mortality from several cancers,16–18 less frequent testing and medication use, better patient satisfaction,19–20 and a reduction in health disparities.4,21,22
What makes family medicine unique?
Family medicine's cornerstone is an ongoing, personal patient–physician relationship. Whereas other specialties are limited to a particular organ system, technology, disease, age, or sex, family medicine integrates care for each person. Family physicians' unique contributions to health care access stem from the breadth of their training and adaptability of their work, combined with a sense of social responsibility.
Patients value a physician who listens to them, who takes time to explain things to them, and who is able to effectively coordinate and integrate their care.4 Since its inception, family medicine has been grounded in the core values of a continuing relationship between patient and physician, and the provision of comprehensive care that includes prevention, acute intervention, chronic disease management, end-of-life care, and coordination of care throughout the health care delivery system.
What career opportunities will be available to me as a family physician?
Training in family medicine gives a physician the flexibility to adapt to different practice environments.23 Family physicians work in multispecialty group practices and in solo practice settings. More than 80 percent of family physicians choose to have hospital privileges.23 Some limit their practice to an emergency department or work exclusively within the hospital. Many family physicians provide care in a combination of settings. They may work full-time or part-time. They may work within a managed care plan or a group for a set salary, or they may run their own business. Family physicians may pursue careers in public health, government, academia, and political office.
Is family medicine training good preparation for a career in international medicine, frontier or wilderness medicine, or emergency care?
Family physicians receive broad medical training that prepares them to care for patients in a wide range of settings. With good training, family physicians are competent to practice in a large hospital with many health care resources or in an international or wilderness environment where resources may be scarce.
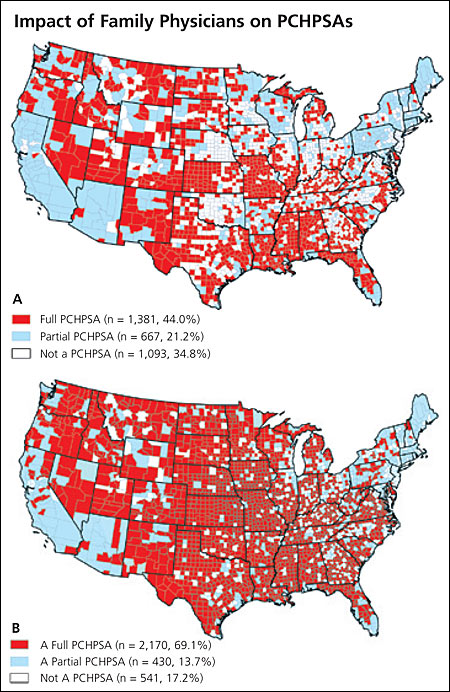
Americans in rural areas depend on family physicians to deliver care in the communities and remote locations in which they live and work. The geographic distribution of family physicians is similar to that of the U.S. population: 24 percent of the population lives in communities of fewer than 10,000 persons, and 23 percent of family physicians practice in such communities.24 Without family physicians, many U.S. counties would be health professional shortage areas (HPSAs)—geographic areas, population groups, or medical facilities that the U.S. Department of Health and Human Services determines to be served by too few health professionals of particular specialties. If all family physicians were withdrawn, 58 percent of U.S. counties would become primary care HPSAs (PCHPSAs) (Figure 2); in contrast, only 8 percent of counties would be PCHPSAs if all general internists, pediatricians, and obstetrician-gynecologists were withdrawn.25 Among physicians working in U.S. emergency departments, approximately 30 percent completed family medicine residencies.26
What is involved in family medicine training, and what are combined residencies?
Family medicine residencies, like pediatric and internal medicine residencies, last three years. Hospital training occurs during each year of family medicine residency training. Family medicine residents work and learn throughout the hospital, in the emergency department, labor and delivery department, the operating room, and intensive care units, and on numerous general and specialty wards.
Family medicine residents care for their continuity patients in a supervised group practice at the residency clinical offices. Residents are assigned a panel of patients and provide continuous care for those patients throughout their training, including inpatient care, maternity care, and hospice care when necessary. Family medicine leads the primary care disciplines in outpatient continuity clinical hours.27 Behavioral science training, counseling, and community outreach are all features of family medicine residency training.
There are more than 460 family medicine residencies in the United States. Combined residencies are hybrids of two residencies (e.g., family medicine and psychiatry, family medicine and internal medicine).
Students often ask about “med-peds” programs and how they differ from family medicine training. Med-peds programs combine three-year residencies in internal medicine and pediatrics into one four-year program, with most med-peds physicians pursuing subspecialty fellowships. The Accreditation Council for Graduate Medical Education does not accredit combined programs as one program but maintains the specialty distinction of the two programs. Graduates of combined programs are eligible to take two certification examinations, according to the expectations of each of the two specialties.
What is the difference between university-based and community-based residency programs?
Traditionally, in university-based programs family medicine residents train alongside residents in other specialties. Residents in university-based programs regularly have the opportunity to teach medical students. Community-based residency programs traditionally are in smaller hospital settings, where family medicine may be the only residency and student contact may be less than that in university-based programs.
Some students think family medicine residents in community-based programs are first in line for admissions and procedures and have more opportunities for supervisory roles, whereas family medicine residents at a university gain exposure to the latest innovations and research discoveries and have more opportunities to develop as teachers. However, these broad characterizations are often inaccurate. Students should decide which overall context will be the best for them, considering factors such as setting (rural or urban), program size, region, patient populations served, and procedural training offered. Most advisers recommend that students look at both university- and community-based programs in their research. Valuable information, tips, and strategies for the residency application process can be found on the Virtual Family Medicine Interest Group (FMIG) Web site (http://fmignet.aafp.org).
What types of advanced training or fellowships are available to family medicine graduates?
Family physicians have a variety of advanced training options open to them after completing their residency training. Common reasons for pursuing advanced training include the desire to obtain research training, preparation to enter academics, and gaining more in-depth clinical skills to offer in one's practice. A fellowship directory produced by the AAFP in cooperation with STFM is available at https://www.aafp.org/fellowships. This valuable resource lists fellowships by content area as well as by state.
Fellowship programs in geriatrics, sports, and adolescent medicine lead to a certificate of added qualifications (CAQ) from the American Board of Family Medicine (ABFM). Successful CAQ candidates must be certified in family medicine. More information on CAQs can be found on the ABFM Web site (http://www.theabfm.org). Other fellowships that are popular among graduates of family medicine residencies include faculty development, maternity care, preventive care, research, and palliative care. Many of the fellowship programs listed in the directory are customized arrangements made between an institution and the trainee.
How do family physicians keep current with medical advances in the care of children, adolescents, adults, older adults, men, women, and pregnant women?
Family medicine was the first specialty to require continuing medical education (CME) of its members. Family physicians must earn a minimum of 50 CME credits annually; this training enables them to continue to learn and keep up with medical advances throughout their careers. CME is required for board certification in family medicine, for hospital and practice privileges in many locales, and for membership in the AAFP.
CME is delivered to family physicians through live courses (for new knowledge and for adding procedures to practice) and published materials (print, audio, and video). American Family Physician has the widest circulation of any primary care journal and is available to student members of the AAFP. Family physicians are increasingly obtaining CME through the Internet, where all types of CME are delivered.
A dramatic shift in CME for physicians was created by family medicine in 2002. Evidence-based CME (EB CME) uses internationally accepted sources of medical evidence as the basis for key practice recommendations (https://www.aafp.org/online/en/home/cme/cmea/ebcme.html). EB CME is the basis for two revolutionary formats of CME, jointly developed under the leadership of the AAFP and the American Medical Association (AMA): point-of-care CME and performance improvement CME. These new forms of CME promise not only to improve patient outcomes through evidence-based medicine, but also to prepare family physicians for the measures insurers and payers will require.
What is the scope of practice for family physicians?
The goal of the Future of Family Medicine project (http://www.futurefamilymed.org/index.html), a joint effort of the Family Medicine Working Party, was to develop a strategy to transform and renew the specialty of family medicine to meet the needs of patients and society in a changing environment. One of the lessons learned from this project was that patients want the availability of a broad array of services.4
Sixty percent of family physicians care for newborns. About 15 percent of visits to a typical practice are from children. At the other end of the age continuum, more than 90 percent of family physicians treat Medicare patients.28
Most family physicians have a component of their practice outside the office. A large majority (82 percent) have hospital privileges, and more than 40 percent manage patients in the intensive care unit or coronary care unit. Of family physicians' patients who are admitted to the hospital, most are treated by family physicians, their partners, or a call group. Other family physicians choose to turn over the care of their hospitalized patients to full-time hospitalist physicians, many of whom are family physicians. In addition to patients treated in the clinic or hospital settings, typical family physicians also supervise the care their patients receive while in nursing homes, home health care, or hospices. In some communities, family physicians include a significant amount of maternity care in their practice: 23 percent of residency-trained family physicians deliver babies, with an average of 2.4 deliveries each month.28 Additional information about family physicians' practices can be found at https://www.aafp.org/about/the-aafp/family-medicine-specialty.html.
What elements of family medicine are most rewarding?
Personal rewards of practicing family medicine include the satisfaction of establishing continuous, long-term relationships with patients and partnering with patients in the management of their health. Family physicians gain great satisfaction from the rewards intrinsic to patient care, including a personal connection with and gratitude from patients (Table 14 ).
| A role in integrating patient care |
| Communicating with patients, listening to their secrets and fears, and educating them regarding their health status and care options |
| Generating relevant new knowledge through practice-based research |
| Intellectual stimulation from the variety of scope of family medicine |
| Networking with other practices to provide the best care for their patients |
| The opportunity to provide effective practice administration to support patient care |
| The opportunity to make a difference in the lives of patients, their families, and their communities |
| The opportunity to work in multidisciplinary teams to achieve better health outcomes |
| Using new information technology to deliver and improve care |
Family physicians enjoy the challenge of making the right diagnosis from what may seem to be a series of unrelated and often vague symptoms. Family physicians are highly valued for their diagnostic and patient-advocacy skills. Providing care for patients throughout their lives helps ensure they get appropriate screening and preventive services well before they have established disease. Family physicians take pride in their ability to help patients understand the varied and subtle ways in which a person's health affects the family and community.3
What types of procedures are typically performed by family physicians?
In addition to routine inpatient and outpatient care, family physicians perform a wide range of procedures. Most family physicians (82 percent) perform skin and nail procedures; 35 percent regularly perform colposcopy; and 35 percent perform flexible sigmoidoscopy.29 Family physicians receive training in a variety of procedures, including joint injections, paracentesis, thoracentesis, intubation and advanced life support, ultrasonography, stress testing, colonoscopy, esophagogastroduodenoscopy, vasectomy, tubal ligation, cervical cancer treatment (e.g., loop electrosurgical excision procedure [LEEP], cryotherapy), and pulmonary function testing. Family physicians also receive training in maternity care, which includes prenatal management, intrapartum procedures, delivery, and management of maternal and neonatal complications.
What is the typical medical education debt of family medicine residency graduates, and what types of loan repayment and consolidation options are available to family physicians?
Medical education debt has increased significantly in the past 20 years. According to the Association of American Medical Colleges (AAMC), the median level of debt of medical school graduates in the class of 2005 was $120,000, including undergraduate loans.30 The median level of debt of family medicine residency graduates in 2004 was $145,300, according to the AAFP.23
Medical education financial aid differs from financial aid for any other professional group of students. There is a wide and at times confusing array of options: government (direct) loans, Federal Family Education Loan Program loans, internship/residency forbearance, economic hardship deferments, scholarships, service commitment scholarships, graduated repayment plans, and extended repayment plans.
Students and residents should consider the impact of debt and seek out the best information and advice. The most important source of information is a good-quality loan exit interview, which is required at all U.S. allopathic and osteopathic schools for all students with a federal loan. Financial aid officers have become extremely important resources for medical students, and their expertise should be sought out whenever questions arise.
The AAMC has several useful Web sites for medical students, including http://www.aamc.org/stloan and http://www.aamc.org/students(Table 2). The AMA has information regarding medical student debt in the medical student section of its Web site (http://www.ama-assn.org/ama/pub/category/5010.html). The FMIG Web site is also a good resource. The AAFP Debt Management Guide can be found at http://fmignet.aafp.org/x24.xml. There are several ways to manage loans, and students need to be well informed.
Are family physicians in demand?
The demand for family physicians in the United States has continued to rise since 2003. The Merritt, Hawkins and Associates' 2006 Review of Physician Recruiting Incentives shows a steady increase in demand for family physicians, with family medicine being the second most recruited specialty.31 Job openings continue to be strong for family physicians. In a recent national survey of hospitals that were recruiting physicians, 45 percent were recruiting family physicians, whereas 32 percent were recruiting internists, 21 percent obstetricians, and 20 percent anesthesiologists.31 Similarly, classified advertisements for family physicians increased 12 percent from 2003 to 2004, and 20 percent from 2004 to 2005.32 Demand is expected to remain strong as the U.S. population grows and the need for medical care increases with the increasing prevalence of chronic disease.33 The mean salary of family physicians in 2004 was $143,600.23
What is the future of family medicine?
The Future of Family Medicine report identified what patients want and expect from their primary, personal physician: first, establishment of a continuing relationship; and second, provision of a personal medical home to which they can bring any health problem and where they can partner with their physician to maximize their wellness.4
Based on the findings of the Future of Family Medicine report, a new model of family medicine is being demonstrated; this began in 2006. The family medicine model of care aims to reintegrate and personalize health care for patients, who are increasingly frustrated with the fragmented and complex health care system. This model provides patients with a personal medical home through which they can expect to receive comprehensive health care within the context of a continuing relationship with their physician.
Electronic health records are becoming the central nervous system of the family medicine practice, reducing medical errors and improving quality of care. The AAFP's Center for Health Information Technology provides family physicians with tools and resources to develop health information technology in their practices (http://www.centerforhit.org).
In the future, family medicine will provide a model of care that is fully patient-centered, including innovations such as open-access scheduling, group visits, and improved electronic communication between patients and practice staff to ensure that patients get what they need, when they need it.