Am Fam Physician. 2007;76(2):208
The first expansion of allopathic medical education in 35 years is under way; this could eliminate rural physician shortage areas if students more likely to practice in rural areas are preferentially admitted and supported.
Although 21 percent of the U.S. population lives in rural areas, only 10 percent of physicians practice there.1 Currently, allopathic medical schools are expanding, bolstered by calls from the Association of American Medical Colleges and the Council on Graduate Medical Education to increase medical student positions by 15 to 30 percent over the next decade.2 Thus, there exists a rare opportunity to link school expansion to policy goals.
The educational pipeline to rural medical practice is long and complex, from rural elementary education to rural residency training tracks. Increasing the number of rural-background students in medical school is important to reduce disparities in physician distribution. Solutions must be aimed at selecting the “right” students and giving them the “right” content and experiences to train them for rural practice. Despite evidence that students of rural origin are more likely to practice in a rural area,3 in the past two decades rural student matriculation has declined while rural health care shortages persist.4
Medical school expansion provides an opportunity to reconsider how the physician workforce can be aligned with national and local needs. Expansion without consideration of physician distribution will likely perpetuate the concentration of physicians in urban areas and near major medical centers. Policies aimed at selecting students most likely to practice in rural areas could assist in securing an adequate supply of well-trained rural physicians.
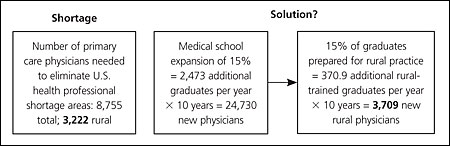
It is estimated that the elimination of primary care health professional shortage areas requires an additional 8,755 primary care physicians,5 3,222 in rural settings.5,6 A medical school expansion of 15 percent (2,473 students per year) could fill this gap in less than 10 years if 15 percent of this increase were prepared and inspired to enter rural practice, and an expansion of 30 percent in less than five years, assuming a stable rural population (see accompanying figure).5,6 Policies supporting preference for rural-born applicants, rural training tracks in medical schools and residencies, financial support for rural physicians, and increased awareness of federal bonus payments for underserved areas are options for increasing rural matriculation and eventual service. Expansion that is not aligned with policy aims is unlikely to address specific needs, whereas thoughtful expansion provides an opportunity to help rural America.