
Am Fam Physician. 2007;76(4):533-538
Author disclosure: Nothing to disclose.
The American College of Radiology has developed appropriateness criteria for a number of clinical conditions and procedures. Criteria are available on imaging tests used in the evaluation of acute chest pain—suspected myocardial ischemia. Imaging tests for a suspected cardiac etiology include transthoracic echocardiography, transesophageal echocardiography, radionuclide perfusion imaging, radionuclide ventriculography, radionuclide infarct avid imaging, and positron emission tomography. If the cardiac ischemic work-up is negative or indeterminate, applicable tests include chest radiography; conventional, multidetector, and electron beam computed tomography; and magnetic resonance imaging. A summary of the criteria, with the advantages and limitations of each test, is presented in this article.
Persons presenting to the emergency department with chest pain may be experiencing acute coronary syndrome, dissecting aortic aneurysm, pulmonary embolism, or possibly a less serious event. Timing is important when diagnosing these patients, so it is vital to quickly and accurately establish a diagnosis. The American College of Radiology (ACR) recently elected to evaluate and assign appropriateness ratings for selected imaging tests used in the evaluation of acute chest pain—suspected myocardial ischemia.1
In most patients with acute coronary syndrome, the initial evaluation is done with electrocardiography and measurement of serum creatine kinase-MB isoenzyme or serum cardiac troponin levels. Electrocardiography and elevated cardiac markers may be all that are needed to establish a diagnosis and initiate treatment; however, if these tests are indeterminate, other imaging tests need to be considered. Most of the 5 million patients with chest pain presenting to the emergency department do not have a cardiac etiology and, therefore, other imaging tests are usually needed.2 Tests for evaluating patients with acute chest pain include chest radiography, transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), computed tomography (CT), nuclear medicine imaging, and magnetic resonance imaging (MRI). The ACR has developed appropriateness criteria and ratings for these tests to better understand the role of imaging in the patient with acute chest pain.
Illustrative Case
A 54-year-old man with diabetes presents to the emergency department with dyspnea on exertion and a remote history of chest pain. He is a two-pack-per-day smoker and has a strong family history of heart disease. Two weeks ago, he experienced an episode of chest pressure that was accompanied by diaphoresis. His physical examination was normal with the exception of a recorded blood pressure of 149/87 mm Hg and a fasting blood glucose level of 275 mg per dL (15.3 mmol per L). An electrocardiogram, chest radiograph, and initial set of enzymes were normal; however, the patient was still admitted for further evaluation because of the classic cardiac symptoms and risk factors for coronary artery disease. The preliminary diagnosis was chest pain of suspected ischemic origin, and it was decided that the patient should undergo conventional coronary angiography.
Before doing the more invasive conventional coronary catheterization, it was elected to do a transthoracic echocardiography and a single-photon emission computed tomography (SPECT) thallium scintigraphy to look for a perfusion deficit. Echocardiography showed a 71 percent ejection fraction with normal cardiac valve motion. The SPECT study revealed a perfusion deficit that was later confirmed with coronary angiography. The patient ultimately underwent successful bypass grafting.
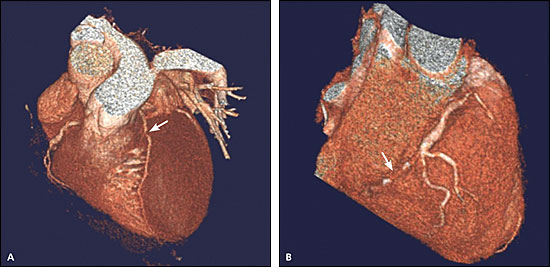
An alternative approach to this patient would have been to order a multidetector CT coronary calcium study and a coronary CT angiography to document that coronary stenosis was indeed present. For example, if the calcium study showed that the patient had a calcium score of 163, he would be categorized as likely to have coronary stenosis with an 83 percent risk of a cardiac event compared with his peer group. A correlating coronary CT angiography might show an 80 percent stenosis of the mid-left anterior descending artery (Figure 1A), a 50 percent stenosis of the proximal right coronary artery, and a complete occlusion of the right coronary artery distal to two acute marginal arteries (Figure 1B). This would also be an indication for a confirmatory coronary CT angiogram and subsequent bypass grafting.
Imaging
The ACR appropriateness criteria for the imaging tests used in the evaluation of acute chest pain—suspected myocardial ischemia are listed in Table 1.3 A more detailed discussion of the criteria, as well as the strength of the references supporting these criteria, can be found in the original ACR article.1
| Radiologic examination | Appropriateness rating* | Comments |
|---|---|---|
| Chest radiography | 9 | Needed to exclude other etiologies for chest pain |
| Coronary angiography | 8 | May be necessary to define the extent of stenosis or occlusion; always done before surgery; typically done late in the work-up |
| Transthoracic echocardiography | 7 | Indicated as a screening test to evaluate cardiac function; inexpensive and portable |
| Left ventricular angiography | 7 | May be indicated to evaluate ventricular function as part of the ischemic work-up; typically done late in the work-up |
| Radionuclide perfusion imaging | 6 | Helpful in evaluating extent of ischemia; typically done if initial screening tests suggest an ischemic origin |
| Radionuclide ventriculography | 6 | May be indicated in evaluating cardiac function |
| Radionuclide infarct avid imaging | 5 | May be indicated to better define infarction |
| Transesophageal echocardiography | 4 | May be indicated in evaluating cardiac function or in assessing aortic dissection |
| Electron beam and multidetector computed tomography with contrast agent | 4 | Probably not indicated except in assessing ventricular function; noncontrast images have usefulness in screening for coronary calcification; is often indicated if the cardiac work-up is negative |
| Magnetic resonance angiography | 4 | Few indications in patients with acute chest pain |
| Conventional computed tomography with contrast agent | 3 | Little indication, except for documenting other etiologies of chest pain |
| Magnetic resonance imaging | 3 | Little indication, except in screening for aortic dissection; may have applicability in evaluating cardiac function |
| Magnetic resonance perfusion imaging | 2 | Recent studies show promise in evaluating infarction; not currently used in patients with acute chest pain |
| Positron emission tomography | 2 | May be useful in indeterminant cases |
TESTS INDICATED FOR SUSPECTED MYOCARDIAL ISCHEMIA
Cardiac Catheterization with Coronary Angiography and Ventricular Angiography
The first-line and ultimate determinant of coronary obstruction and ventricular function is cardiac catheterization with coronary and ventricular angiography.4 Although this test is valuable, it is often the last one performed. Cardiac catheterization is always indicated before a definitive surgical procedure or angioplasty.
TTE
Myocardial ischemia may be the etiology for chest pain, especially if abnormalities of left ventricular wall motion are detected.5–8 The most significant advantages of TTE are its portability and noninvasiveness. Depending on the location, wall-motion abnormalities are often, but not always, identifiable with TTE.6 In addition to wall-motion abnormalities, other helpful findings would be the identification of a left ventricular aneurysm or the presence of valvular dysfunction. TTE also is helpful in diagnosing pericardial effusions.
TEE
TEE is more invasive and is less useful in the evaluation of acute chest pain. It is useful for ruling out aortic dissection, valvular dysfunction, intracardiac thrombi, and intracardiac shunts. Because these findings are uncommon, TEE generally is not indicated in the immediate work-up unless aortic dissection is highly suspected.9,10 Of note, CT would be the preferred initial study if aortic dissection is suspected, but TEE would be an alternative.11
Radionuclide Perfusion Imaging
For the most part, these tests are relatively inexpensive and are not associated with significant morbidity or mortality. SPECT tests have a long and appealing history of accurately assessing myocardial ischemia. Commonly used agents include thallium-201, sestamibi, and tetrofosmin. Myocardial perfusion imaging using SPECT thallium-201 scintigraphy is one of the more valuable tests.8,12–14 A thallium-201 perfusion deficit on exercise that is absent or markedly diminished at rest is a key identifier of myocardial ischemia.12–16 Radionuclide perfusion imaging typically requires transport of the patient to the imaging suite, and false-positive and false-negative results are not uncommon.
Radionuclide Ventriculography
Radionuclide ventriculography may be indicated in patients with acute chest pain of ischemic origin. This test is inexpensive and reasonably accurate, and it can demonstrate abnormalities in left ventricular function. Because of its accuracy, low cost, wide availability, and minimal morbidity, radio-nuclide ventriculography may be indicated, especially if other studies for suspected myocardial ischemia are indeterminate or if the assessment of left ventricular function is important in determining future therapy.
Radionuclide Infarct Avid Imaging
Radionuclide infarct avid imaging identifies acute infarction by observing radiotracer uptake in the affected area.17,18 However, the imaging may not become positive until 12 to 36 hours after infarction, making it less useful in the emergency department setting. Cardiac enzyme levels are usually better indicators of acute infarction and, because they can be obtained rapidly and at a lesser expense to the patient, these tests are generally used instead. Radionuclide infarct avid imaging may still have some applicability in quantifying infarct size or in identifying stunned or hibernating myocardium.
Positron Emission Tomography
Positron emission tomography may reliably show myocardial blood flow using N13-ammonia tracers. It can also document anaerobic metabolism with F18 fluorodeoxyglucose.19 This technology is expensive and not universally available. It typically is not indicated in the immediate work-up of a patient with suspected myocardial ischemia.
TESTS INDICATED IF ISCHEMIC WORK-UP IS NEGATIVE OR INDETERMINATE
Chest Radiography
Chest radiography is important in ruling out pathologic conditions that may masquerade as myocardial infarction, including pneumothorax, fractured ribs, and pneumonia.20,21 All of these conditions are generally identifiable on the chest image. Other entities, such as ruptured aneurysms, aortic dissections, and pulmonary emboli may be suggested on chest radiography, but with a lower sensitivity. Myocardial infarction will generally not be diagnosable unless there are associated signs of cardiac enlargement, congestive heart failure, or pulmonary edema.
Coronary CT Angiography
Coronary CT angiography is minimally invasive and is increasingly being used to identify vessel stenosis and occlusion.22,23 Coronary CT angiography can show atherosclerotic plaque in the vessel wall as well as stenoses, and the images correlate well with conventional angiography. Because many conventional catheterizations are normal, coronary CT angiography can help identify persons likely to have stenotic lesions and thus decrease the need for catheterization.
Conventional CT
Conventional CT is widely used in identifying aortic aneurysms and dissections and pulmonary emboli. Pericardial effusions and thickening also are readily identifiable. CT is increasingly used to identify thrombi within pulmonary arteries. However, multidetector CT technology has supplanted conventional CT as the preferred imaging modality.
Multidetector and Electron Beam CT
Multidetector and electron beam CT are the preferred modalities in evaluating patients with acute chest pain of suspected nonischemic origin. Pneumonias, pneumothoraces, tumors, pericardial effusions, pulmonary emboli, and aortic aneurysms and dissections are readily identifiable.24 These modalities also are useful in demonstrating coronary artery calcification as an indicator of atherosclerosis; however, because calcium is not site specific, multidetector CT or electron beam CT should not be used as the sole indicator of stenosis. Recent calcification studies have confirmed that the extent and number of vessels involved are associated with the presence of stenosis and an increased likelihood of a cardiac event.25,26 Alternatively, if no calcium is present, the chances of the chest pain having a cardiac etiology are extremely low.26
MRI
MRI is useful for demonstrating infarcts, abnormalities of wall motion, and pericardial effusions.27–29 At times, MRI may show intracardiac thrombi; however, this technology has little application for imaging patients with acute myocardial ischemia. Other tests, such as radionuclide ventriculography, TTE, or TEE, can provide similar information at much less expense. Magnetic resonance angiography and magnetic resonance atherosclerotic plaque characterization are still investigational and are not yet widely used in a clinical setting.30,31
Magnetic Resonance Perfusion Imaging
Magnetic resonance perfusion imaging is typically not indicated in the work-up of a patient with acute chest pain. Current contrast agents can demonstrate normal myocardium and show signal changes in areas of decreased perfusion. There is a potential for the use of these agents, but their use in the emergency department has not yet been proven. Access to the unstable patient and the patient with claustrophobia are potential problems in using magnetic resonance technology.
Final Comments
Current consensus supports the use of electrocardiography and cardiac enzyme levels in evaluating patients with chest pain, especially if they are unstable. Consensus also supports the use of radionuclide SPECT scintigraphy in the assessment of myocardial perfusion and ventricular function.12,32 Echocardiography is helpful in evaluating wall-motion abnormalities; however, the definitive diagnosis may need to be made with coronary angiography. Recent developments in myocardial perfusion imaging using MRI and positron emission tomography may prove helpful in the future. Recent publications show increasing use of CT in identifying calcium as an indicator of atherosclerosis and cardiac risk, and coronary CT angiography in assessing coronary stenosis and occlusion, but their widespread use in the evaluation of patients with acute coronary syndrome has yet to be fully established.