
Am Fam Physician. 2008;77(4):444
As a high school and college basketball player I suffered my fair share of bumps and bruises. My left ankle received the most serious mistreatment, including a bad break and multiple severe sprains; I imagine it was pleased when I graduated and my playing days were over. Still, the ankle worsened, until even walking was painful. Surgery became inevitable.
There is never a “good” time to have ankle surgery, especially with a full-time job and living in Boston in winter. Between the pain, the awkwardness of cast and crutches, the danger of ice and snow, and being dependent on public transportation, I was not only exhausted, but also depressed. I spent most of my time in front of the computer or TV.
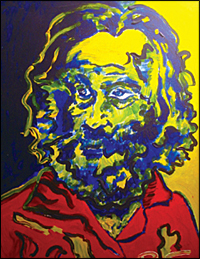
In December, my fiancée gave me a collection of poems I had written, each paired with a photograph of canvases I had painted. She wanted to remind me of what I could still do in hopes I would stop concentrating on what I couldn't. Over the next months, I endeavored to do exactly that. I wrote more poetry and completed a few paintings (above). I also got together with friends more often and reminded myself that I wanted to be somebody they enjoyed being around as much as I enjoyed being around them.
These activities were not a panacea; it was easier to wallow in frustration and self-pity than to change my pattern of unhappy inactivity. The most challenging aspect of my surgery was forcing myself to tackle the difficult task of elevating my own mood, and making the conscious effort to adjust my attitude and approach to recovery.—r.s.
COMMENTARY
The impact of chronic illness is easily underestimated by physicians. It's natural for us to focus our attention on the next patient walking in rather than the one who just left, and to forget about the larger world our patients must navigate outside our office.
R.S.'s attempt to “change my pattern of unhappy inactivity” is easy to understand, but difficult to implement. As family physicians, we are uniquely positioned to address our patients' biopsychosocial stressors and positively impact their lives.
I have found the BATHE psychotherapy technique (background, affect, troubling problem, handling of the problem, empathy) can help patients to improve the quality of their own lives when they feel surrounded by chronic pain or feelings of helplessness.1 It is easy to facilitate in a brief office visit, and safer than throwing another medication at an overburdened patient.