
Am Fam Physician. 2008;78(8):953-960
Author disclosure: Nothing to disclose.
The second stage of labor is a dynamic event that may require assistance when maternal efforts fail to effect delivery or when there are nonreassuring fetal heart tones. Therefore, knowing how to perform an operative vaginal delivery with forceps or vacuum is vital for family physicians who provide maternity care. Vacuum is rapidly replacing forceps as the predominant instrument, but each has advantages and disadvantages, including increased risk of maternal trauma with forceps and increased risk of neonatal cephalohematoma with vacuum. Use of a second instrument if the first one fails is associated with worse outcomes. Routine episiotomy in operative vaginal delivery is no longer recommended. The “ABCDEFGHIJ” mnemonic can facilitate proper use and application of the vacuum device and minimize risks, and practicing the techniques on mannequins can provide an introduction to the skills of operative vaginal delivery.
The second stage of labor is a dynamic event that may require assistance when maternal efforts fail to effect delivery or when there are nonreassuring fetal heart tones. Therefore, the ability to perform an operative vaginal delivery with forceps or vacuum remains a vital skill for family physicians who provide maternity care. The World Health Organization considers operative vaginal delivery to be a critical part of basic emergency obstetric care.1
Although rates of operative vaginal delivery are dropping, vacuum has emerged as the most popular delivery instrument in the United States. The rate of operative vaginal delivery fell 45 percent, from 9.4 percent of live births in 1994 to 5.2 percent in 2004.2 Vacuum deliveries comprised 4.1 percent of all live births in 2004, whereas forceps deliveries dropped dramatically, from 5.5 percent of births in 1989 to 1.1 percent in 2004.2 Training in forceps use also has decreased, with one study showing that only one half of graduating obstetrics and gynecology residents surveyed felt comfortable performing forceps deliveries in their practice.3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Operative vaginal delivery using a vacuum device can cause less maternal trauma than forceps, but it can increase the risk of neonatal cephalohematoma and retinal hemorrhage. | A | 11 |
| Vacuum-assisted vaginal delivery using a soft cup causes less neonatal scalp injury than traditional rigid cups, but it also has a higher failure rate. | A | 19 |
| In vacuum-assisted vaginal delivery, proper application and use of the vacuum device, including limiting application time to 20 minutes and three pulls, as well as avoiding multiple disengagements of the vacuum (or “pop-offs”), can minimize adverse events. | B | 23, 27, 28 |
| Episiotomy during an operative vaginal delivery is no longer recommended because it can increase the risk of perineal injury. | B | 29 |
| Operative vaginal delivery using both a vacuum device and forceps has been associated with worse neonatal outcomes than using a single instrument. | B | 18, 30 |
Indications and Prerequisites for Operative Vaginal Delivery
According to the American College of Obstetricians and Gynecologists (ACOG), operative vaginal delivery should be considered when there is a prolonged second stage of labor or nonreassuring fetal heart tones that would indicate fetal compromise, or if the second stage needs to be shortened for maternal benefit (e.g., maternal exhaustion).4 Definitions of prolonged second stage are noted in Table 1.4 Studies have demonstrated the safety of continuing the second stage of labor beyond these arbitrary limits if progress is being made and fetal heart tones are reassuring.5,6
| Prolonged second stage of labor, defined as: | |
| A lack of continuing progress for two hours without regional anesthetic, or three hours with regional anesthetic in nulliparous women | |
| or | |
| A lack of continuing progress for one hour without regional anesthetic, or two hours with regional anesthetic in multiparous women | |
| Nonreassuring fetal heart tones or other suspicion of immediate or potential fetal compromise | |
| Shortening of the second stage of labor for maternal benefit (e.g., maternal exhaustion) | |
Fetal position is important when contemplating operative vaginal delivery. The fetus must be in a cephalic presentation, and the sutures should be palpated to determine the position as occipitoanterior or occipitoposterior. The cervix needs to be completely dilated and the amniotic membranes ruptured. Vacuum-assisted delivery should not be performed if the fetus has a suspected bone mineralization or bleeding disorder, or if cephalopelvic disproportion exists (Table 2).4 Although there is little supportive evidence, it is recommended that vacuum deliveries not be routinely performed in pregnancies at less than 34 weeks' gestation because of the potential increased risk of fetal intracranial hemorrhage.
| Cephalopelvic disproportion |
| Fetal head not engaged |
| Gestational age less than 34 weeks |
| Known fetal conditions that affect bone mineralization or bleeding disorder |
| Noncephalic or facial presentation |
Fetal Position and Vacuum-Assisted Vaginal Delivery
Fetal engagement is defined as the passage of the biparietal diameter of the fetal head through the plane of the pelvic inlet. Clinical evidence of engagement on examination exists when the leading edge of the fetal skull is at or below the ischial spines. Careful examination must be done after a prolonged second stage of labor in which the fetal skull may be elongated and molded, resulting in the caput descending below the +2 cm station, whereas the skull itself is much higher. Zero station does not prove engagement, especially with a posterior presentation or a large degree of molding.7 Physicians can improve their clinical estimate of engagement by using the abdominal hand to feel how much of the fetal head is above the upper level of the pubic symphysis. Because of the difficulties of clinically estimating engagement, operative vaginal deliveries have been reclassified (Table 3).4 Delivery instruments should never be applied to an unengaged fetal head.
| Classification | Station |
|---|---|
| Outlet | The fetal skull has reached the pelvic floor; the scalp is visible at the introitus without separating the labia. |
| The fetal head is at or on the perineum. | |
| The sagittal suture is in the anteroposterior diameter or in the right or left occipitoanterior or occipitoposterior position. | |
| Rotation does not exceed 45 degrees. | |
| Low | The leading edge of the fetal skull is station +2 cm or more. |
| The head is not on the pelvic floor. | |
| Mid | The head is engaged, but the leading edge of the skull is above station +2 cm. |
| High | Forceps and vacuum are not included in this classification. |
Vacuum devices can be used when the fetal head is in the occipitoposterior position. However, in one study, the rates of anal sphincter lacerations with the use of forceps and vacuum for occipitoposterior deliveries were 72 and 33 percent, respectively, compared with 54 and 27 percent for occipitoanterior deliveries.8 The head often rotates from the occipitoposterior to occipitoanterior position during delivery. It is important to pull at an angle perpendicular to the plane of the cup as the head rotates.
Instrument Choice
Either vacuum or forceps can be effective and safe if used appropriately, but there are still potential risks. The choice of instrument is based on the physician's level of experience, as well as the clinical scenario. For those interested in learning the techniques of forceps and vacuum deliveries, the American Academy of Family Physician's Advanced Life Support in Obstetrics (ALSO) course provides an introduction to these skills.9,10
MATERNAL RISKS
A systematic review of 10 trials comparing vacuum with forceps found that vacuum deliveries were associated with less maternal soft-tissue trauma (odds ratio [OR] = 0.41; 95% confidence interval [CI], 0.33 to 0.50) and required less general and regional anesthetic.11 However, vacuum extraction was more likely than forceps deliveries to fail (OR = 1.69; 95% CI, 1.31 to 2.19).11 A retrospective review of 50,210 vaginal deliveries at a single institution showed the rates of third- and fourth-degree lacerations were 1.7 percent for spontaneous vaginal delivery, 9.3 percent for vacuum extraction, and 19.2 for forceps delivery.12 Several other cohort studies from other institutions also showed increased rates of third- and fourth-degree lacerations with forceps compared with vacuum.13,14
NEONATAL RISKS
Vacuum delivery increases the rates of neonatal cephalohematoma (OR = 2.38; 95% CI, 1.68 to 3.37) and retinal hemorrhage (OR = 1.99; 95% CI, 1.35 to 2.96) compared with forceps delivery.11 Hemorrhages typically resolve without sequelae within four weeks of birth, but cephalohematoma (Figure 1A10) can lead to hyperbilirubinemia. One study showed no differences in vision problems or in child development five years after vacuum or forceps delivery.15 Operative vaginal delivery is a risk factor for shoulder dystocia, and it appears to be more common with vacuum delivery than with forceps delivery (OR = 2.00; 95% CI, 1.62 to 2.48).16 The incidence of shoulder dystocia increases in cases of fetal macrosomia.4
Intracranial hemorrhage and subgaleal or subaponeurotic hematomas (Figure 1B10) are rare but serious events reported with the use of vacuum. In 1998, the U.S. Food and Drug Administration issued a warning about the potential risk of serious intracranial injury or death with the use of vacuum devices.17 The report cited a fivefold increase in reports of fetal death and serious injury that could likely be attributed to the increasing use of vacuum rather than an actual change in the risk of complications. Specific recommendations were made for the use of vacuum, including applying steady traction instead of using a rocking motion, as well as notifying participants in the initial neonatal care that a vacuum was used so that appropriate monitoring could occur.17 Signs and symptoms of serious intracranial injury in a neonate are listed in Table 4.17 A study reviewing 583,340 live births showed increased rates of cerebral hemorrhage with operative vaginal delivery compared with spontaneous vaginal birth, but no statistical difference in the rates of hemorrhage with use of vacuum, forceps, or cesarean delivery; this suggests that abnormal labor may contribute more to intracranial hemorrhage than does method of delivery.18
| Intracranial hemorrhage |
| Apnea |
| Bradycardia |
| Bulging fontanel |
| Convulsions |
| Irritability |
| Lethargy |
| Poor feeding |
| Subgaleal hematoma |
| Diffuse head swelling that shifts with repositioning and indents on palpation |
| Signs of hypovolemic shock (hypotension, pallor, tachycardia, tachypnea) |
| Swelling not limited by suture lines (unlike cephalohematoma) |
Types of Vacuum Devices
Originally, vacuum devices had a rigid metal cup with a separate suction catheter attached laterally and connected to a foot-operated pedal. Today's vacuum cups can be soft or rigid and can be different shapes and sizes. Examples of different types of cups include soft or rigid anterior cups and rigid posterior cups. Posterior cups (Kiwi Omnicup [Figure 2A], Mityvac M-cup, and Bird or O'Neil cups) have been designed for occipitoposterior and asynclitic deliveries. The flatter cup allows for better placement at the flexing position on the fetal head, which is usually much further back in the sacral hollow during occipitoposterior presentation. Newer devices allow for an assistant to hand-pump suction using a separate device (Figure 2B) or for the user to hand-pump suction with a single handheld device (Figure 2C). In the United States, these handheld devices are intended for single use and are disposable.
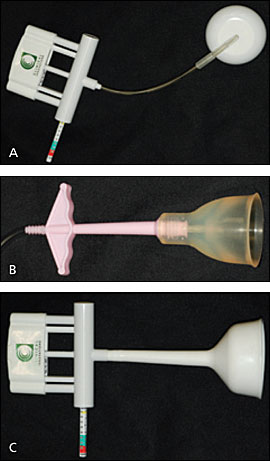
A Cochrane review of nine trials comparing soft and rigid cups showed that soft cups were significantly more likely to fail to achieve vaginal delivery (OR = 1.65; 95% CI, 1.19 to 2.29).19 Failure rates were 10 percent with rigid cups and 22 percent with soft cups. Soft cups, however, were associated with less scalp injury (OR = 0.45; 95% CI, 0.15 to 0.60). There were no significant differences in maternal injury.19 Randomized controlled trials of the Kiwi Omnicup for occipitoposterior and occipitoanterior deliveries showed increased failure rates (relative risk = 1.58; 95% CI, 1.10 to 22.4 in one study), but comparable safety profiles.20,21
Using the “ABCDEFGHIJ” Mnemonic
The ALSO course uses the mnemonic “ABCDEFGHIJ” to describe the steps performed in vacuum extraction.10 Practicing the techniques on mannequins can provide an introduction to the skills of operative vaginal delivery.
Reviewing this acronym, physicians should Address the patient and discuss the risks and benefits of operative vaginal delivery. Assistants should be on hand for delivery and for neonatal resuscitation, and should be made aware of the use of instruments.4,17 Also, Analgesics should be administered, if needed. Regional or pudendal anesthesia is recommended for forceps delivery; however, vacuum delivery without regional or pudendal anesthesia is not uncommon.11,22
The Bladder should be emptied to avoid risk of injury. The Cervix should be completely dilated. The position of the fetal head should be Determined. The physician should check the vacuum Equipment to ensure adequate suction. With the suction off, the center of the cup should be applied 3 cm anterior to the posterior fontanel, centering the sagittal suture under the vacuum (Figures 3A and 3B10). The edge of the cup will be over the posterior fontanel (most cups have a diameter of 5 to 7 cm). This point, located in the midline along the sagittal suture, approximately 3 cm in front of the posterior fontanel and approximately 6 cm from the anterior fontanel, is called the Flexion point. The flexion point is an important point in maximizing traction and minimizing detachment of the cup. Checking for placement of the cup by using the anterior fontanel as the landmark may be easier because the posterior fontanel will be obscured by the cup. No maternal tissue, including the vagina, should be under the cup. The risk of subgaleal hemorrhage increases if the cup edge is placed on the sagittal suture.23 Improper application appears to be common with attempted vacuum-assisted delivery24 and is thought to be a primary factor in unsuccessful attempts.25
The physician should increase the vacuum suction with the manometer at the recommended range and apply Gentle traction at right angles to the plane of the cup during the contraction (Figure 3C10). Some physicians will lower the level of suction between contractions to decrease rates of scalp injury, whereas others will maintain suction in cases of nonreassuring fetal heart tones to aid in more rapid delivery. One randomized controlled trial using the semirigid M-cup vacuum compared intermittent suctioning with constant suctioning to prevent fetal loss of station between contractions. There were no differences in time to delivery or rates of cephalohematoma between the two groups.26 Use of vacuum should be Halted when there are three disengagements of the vacuum (or “pop-offs”), more than 20 minutes have elapsed, or three consecutive pulls result in no progress or delivery. Cephalohematoma rates, as well as brachial plexus injuries, increase with longer application times.27,28
Although it is in the original “ABCDEFGHIJ” mnemonic, performing an Incision for episiotomy increases the risk of perineal trauma and, therefore, is no longer recommended. Compared with nulliparous women who have spontaneous vaginal delivery without episiotomy, the odds of having a severe (third- or fourth-degree) perineal laceration are increased in women who have vacuum delivery without episiotomy (OR = 3.1; 95% CI, 1.9 to 4.3). The odds of a severe perineal laceration are even higher in women who have vacuum delivery with episiotomy (OR = 13.7; 95% CI, 10.1 to 17.3).29 Similar results were noted in multiparous women.
Using Forceps Following Failed Vacuum Delivery
In the past, use of forceps was often considered after an unsuccessful attempt at vacuum delivery. However, several recent studies have shown an increase in neonatal intracranial injury when both vacuum and forceps are applied.18,30 One study showed much higher neonatal risk when using both instruments, with an intracranial hemorrhage rate of one in 256. This is 3.4 times the rate of hemorrhage using vacuum alone.18 Another cohort study saw higher rates of intracranial hemorrhage, brachial or facial nerve injury, and need for assisted ventilation with the use of sequential instruments compared with spontaneous delivery. The relative risk of using both instruments approached the sum of the relative risk of using vacuum or forceps alone.30 ACOG advises against the use of sequential instruments, except in emergent cases in which cesarean delivery is not readily available.4
Postdelivery Care
It is important to carefully inspect the mother for any cervical, sulcal, or anal sphincter tears after operative vaginal delivery. Anal sphincter lacerations are often missed31 and can lead to anal incontinence.32 The neonate should also be examined to look for signs of trauma. The mother should be questioned about her perceptions on the need for operative vaginal delivery and how the delivery went. Good documentation is essential33; components of a well-documented note are included in Table 5.33
| Indications for intervention |
| Position and station of the fetal head |
| Amount of molding and caput present |
| Assessment of maternal pelvis |
| Assessment of fetal heart rate and contractions |
| Record of discussion with the woman of the risks, benefits, and options |
| Number of attempts and ease of application of vacuum or forceps |
| Duration of traction and force used |
| Description of maternal and neonatal injuries |