
Am Fam Physician. 2009;79(5):374-376
Author disclosure: Nothing to disclose.
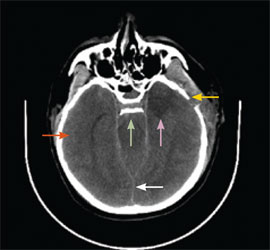
to the editor: A 45-year-old woman with a history of migraines and a recent diagnosis of hypertension presented with a two-day history of increasing headache. She had taken over-the-counter medications with some relief. On the second day, the patient awoke with terrible pain located in the occiput and radiating to the forehead, associated with photophobia, nausea, and vomiting. The headache was unlike any she had ever experienced. Physical examination revealed a dehydrated, distressed woman with a blood pressure of 180/120 mm Hg, pulse of 110 beats per minute, and body temperature of 97°F (36.1°C). There were no neurologic deficits. A computed tomography (CT) scan of the head showed a subarachnoid hemorrhage (see accompanying figure).
The patient was admitted and underwent cerebral angiography two days later, which demonstrated multiple aneurysms. She remained unconscious after brain surgery and required mechanical ventilation. Her condition continued to deteriorate. After a nuclear brain scan demonstrated absence of blood flow to the brain, the patient was pronounced brain dead.
Patients presenting with subarachnoid hemorrhage have a high likelihood of being misdiagnosed initially. In a hospital-based series of 482 patients admitted with sub-arachnoid hemorrhage, initial misdiagnosis occurred in 12 percent of patients.1 Failure to obtain a head CT scan at initial contact was the most common error, occurring in 73 percent of misdiagnosed patients. Among patients with subarachnoid hemorrhage who had normal mental status at first contact (45 percent), the misdiagnosis rate rose to 20 percent; this was associated with a nearly fourfold increase in mortality at 12 months as well as increased morbidity among survivors.2
Sudden “thunderclap” (also known as sentinel) headache, regardless of severity or headache history, should raise the clinical suspicion for subarachnoid hemorrhage. Noncontrast head CT, with or without lumbar puncture, usually establishes the diagnosis of subarachnoid hemorrhage.2 Cerebral angiography should be considered if diagnostic doubt remains.3
Subarachnoid hemorrhage may be caused by trauma or occur spontaneously. It is a medical emergency that can lead to death or severe disability even if recognized and treated at an early stage.4 Treatment includes careful observation for signs of intracranial mass effect, medication, and early neurosurgical intervention. Ten to 15 percent of persons with subarachnoid hemorrhage die before arriving at the hospital,5 and only one half survive to hospital discharge. It is important that family physicians recognize subarachnoid hemorrhage in a timely fashion, because early identification of sentinel headache is key to reducing mortality and morbidity rates.