
Am Fam Physician. 2009;80(5):491-499
Author disclosure: Nothing to disclose.
Management of a wide variety of musculoskeletal conditions requires the use of a cast or splint. Splints are noncircumferential immobilizers that accommodate swelling. This quality makes splints ideal for the management of a variety of acute musculoskeletal conditions in which swelling is anticipated, such as acute fractures or sprains, or for initial stabilization of reduced, displaced, or unstable fractures before orthopedic intervention. Casts are circumferential immobilizers. Because of this, casts provide superior immobilization but are less forgiving, have higher complication rates, and are generally reserved for complex and/or definitive fracture management. To maximize benefits while minimizing complications, the use of casts and splints is generally limited to the short term. Excessive immobilization from continuous use of a cast or splint can lead to chronic pain, joint stiffness, muscle atrophy, or more severe complications (e.g., complex regional pain syndrome). All patients who are placed in a splint or cast require careful monitoring to ensure proper recovery. Selection of a specific cast or splint varies based on the area of the body being treated, and on the acuity and stability of the injury. Indications and accurate application techniques vary for each type of splint and cast commonly encountered in a primary care setting. This article highlights the different types of splints and casts that are used in various circumstances and how each is applied.
Family physicians often make decisions about the use of splints and casts in the management of musculoskeletal disorders. Because of this, they need to be familiar with indications for application, proper technique, and the potential pitfalls of casting and splinting to optimize patient care when treating common orthopedic injuries.
Splints and casts immobilize musculoskeletal injuries while diminishing pain and promoting healing; however, they differ in their construction, indications, benefits, and risks. When determining whether to apply a splint or a cast, the physician must make an accurate diagnosis, as well as assess the stage, severity, and stability of the injury; the patient's functional requirements; and the risk of complications (Table 1).1,2
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Use of a short arm radial gutter splint is recommended for initial immobilization of a displaced distal radial fracture. | B | 11 | RCT |
| Immobilization of the thumb with a removable splint after a ligamentous injury is strongly preferred by patients, and the functional results are equal to those of plaster cast immobilization after surgical and nonsurgical treatment. | B | 12 | RCT |
| Removable splinting is preferable to casting in the treatment of wrist buckle fractures in children. | B | 13 | RCT |
| Evidence supports a functional treatment approach to inversion ankle sprains with the use of a semirigid or soft lace-up brace. | B | 17 | Systematic review |
| Splint/cast | Construction | Indications | Advantages | Risks/disadvantages |
|---|---|---|---|---|
| Splint | Noncircumferential |
|
|
|
| Cast | Circumferential |
| More effective immobilization |
|
Because splints are noncircumferential immobilizers and are, therefore, more forgiving, they allow for swelling in the acute phase. Splinting is useful for a variety of acute orthopedic conditions such as fractures, reduced joint dislocations, sprains, severe soft tissue injuries, and post-laceration repairs. The purpose of splinting acutely is to immobilize and protect the injured extremity, aid in healing, and lessen pain. Splinting during the later phases of injury or for chronic conditions will assist with healing, long-term pain control, and progression of physical function, and it will slow progression of the pathologic process.3,4
Casting involves circumferential application of plaster or fiberglass to an extremity. Casts provide superior immobilization, but are less forgiving and have higher complication rates. Therefore, they are usually reserved for complex and/or definitive fracture management.
Application of any immobilizer comes with potential complications, including ischemia, heat injury, pressure sores, skin breakdown, infection, dermatitis, neurologic injury, and compartment syndrome. These conditions can occur regardless of how long the device is used.5 To maximize benefits while minimizing complications, the use of casts and splints is generally limited to the short term. Excessive immobilization from continuous use of a cast or splint can lead to chronic pain, joint stiffness, muscle atrophy, or more severe complications, such as complex regional pain syndrome.6 All patients who are placed in a splint or cast require careful monitoring to ensure proper recovery.7
Cast/Splint Choice and Application
This article highlights the different types of splints and casts that are used in various circumstances and how each is applied. In a previous article in American Family Physician, we discussed the principles and risks of casting and splinting, as well as proper techniques for safe application.6
Casting and splinting both begin by placing the injured extremity in its position of function. Casting continues with application of stockinette, then circumferential application of two or three layers of cotton padding, and finally circumferential application of plaster or fiber-glass. In general, 2-inch padding is used for the hands, 2- to 4-inch padding for the upper extremities, 3-inch padding for the feet, and 4- to 6-inch padding for the lower extremities.
Splinting may be accomplished in a variety of ways. One option is to begin as if creating a cast and, with the extremity in its position of function, apply stockinette, then a layer of overlapping circumferential cotton padding. The wet splint is then placed over the padding and molded to the contours of the extremity, and the stockinette and padding are folded back to create a smooth edge (Figure 1). The dried splint is secured in place by wrapping an elastic bandage in a distal to proximal direction. For an average-size adult, upper extremities should be splinted with six to 10 sheets of casting material, whereas lower extremities may require 12 to 15 sheets.

An acceptable alternative is to create a splint without the use of stockinette or circumferential padding. Several layers of padding that are slightly wider and longer than the splint are applied directly to the smoothed, wet splint. Together they are molded to the extremity and secured with an elastic bandage (Figure 2). Prepackaged splints consisting of fiberglass and padding wrapped in a mesh layer also exist. These are easily cut and molded to the injured extremity; however, they are more expensive and are not always available. Prefabricated and over-the-counter splints are the simplest option, although they are less “custom fit,” and their use may be limited by cost or availability.

| Area of injury | Type of splint | Type of cast |
|---|---|---|
| Hand/finger | Ulnar gutter, radial gutter, thumb spica, finger | Ulnar gutter, radial gutter, thumb spica |
| Forearm/wrist | Volar/dorsal forearm, single sugar-tong | Short arm, long arm |
| Elbow/forearm | Long arm posterior, double sugar-tong | Long arm |
| Knee | Posterior knee, off-the-shelf immobilizer | Long leg |
| Tibia/fibula | Posterior ankle (mid-shaft and distal fractures), bulky Jones | Long leg (proximal fracture), short leg (mid-shaft and distal) |
| Ankle | Posterior ankle (“post-mold”), stirrup, bulky Jones, high-top walking boot | Short leg |
| Foot | Posterior ankle with or without toe box, hard-soled shoe, high-top walking boot | Short leg, short leg with toe box for phalanx fracture |
| Region | Type of splint/cast | Indications | Pearls/pitfalls | Follow-up/referral |
|---|---|---|---|---|
| Ulnar side of hand | Ulnar gutter splint/cast | Fourth and fifth proximal/middle phalangeal shaft fractures and select metacarpal fractures | Proper positioning of MCP joints at 70 to 90 degrees of flexion, PIP and DIP joints at 5 to 10 degrees of flexion | One to two weeks Refer for angulated, displaced, rotated, oblique, or intra-articular fracture or failed closed reduction |
| Radial side of hand | Radial gutter splint/cast | Second and third proximal/middle phalangeal shaft fractures and select metacarpal fractures | Proper positioning of MCP joints at 70 to 90 degrees of flexion, PIP and DIP joints at 5 to 10 degrees of flexion | One to two weeks Refer for angulated, displaced, rotated, oblique, or intra-articular fracture or failed closed reduction |
| Thumb, first metacarpal, and carpal bones | Thumb spica splint/cast | Injuries to scaphoid/trapezium Nondisplaced, nonangulated, extra-articular first metacarpal fractures Stable thumb fractures with or without closed reduction | Fracture of the middle/proximal one third of the scaphoid treated with casting | One to two weeks Refer for angulated, displaced, intra-articular, incompletely reduced, or unstable fracture Refer displaced fracture of the scaphoid |
| Finger injuries | Buddy taping | Nondisplaced proximal/middle phalangeal shaft fracture and sprains | Encourage active range of motion in all joints | Two weeks Refer for angulated, displaced, rotated, oblique, or significant intra-articular fracture or failure to regain full range of motion |
| Aluminum U-shaped splint | Distal phalangeal fracture | Encourage active range of motion at PIP and MCP joints | ||
| Dorsal extension-block splint | Middle phalangeal volar plate avulsions and stable reduced PIP joint dislocations | Increase flexion by 15 degrees weekly, from 45 degrees to full extension | ||
| Buddy taping permitted with splint use | ||||
| Mallet finger splint | Extensor tendon avulsion from the base of the distal phalanx | Continuous extension in the splint for six to eight weeks is essential | ||
| Wrist/hand | Volar/dorsal forearm splint | Soft tissue injuries to hand and wrist Acute carpal bone fractures (excluding scaphoid/trapezium) Childhood buckle fractures of the distal radius | Consider splinting as definitive treatment for buckle fractures | One week Refer for displaced or unstable fractures Refer lunate fractures |
| Short arm cast | Nondisplaced, minimally displaced, or buckle fractures of the distal radius Carpal bone fractures other than scaphoid/trapezium | |||
| Forearm | Single sugar-tong splint | Acute distal radial and ulnar fractures | Used for increased immobilization of forearm and greater stability | Less than one week Refer for displaced or unstable fractures |
| Elbow, proximal forearm, and skeletally immature wrist injuries | Long arm posterior splint, long arm cast | Distal humeral and proximal/midshaft forearm fractures Nonbuckle wrist fractures | Ensure adequate padding at bony prominences | Within one week Refer for displaced or unstable fractures |
| Double sugar-tong splint | Acute elbow and forearm fractures, and nondisplaced, extra-articular Colles fractures | Offers greater immobilization against pronation/supination | Less than one week Refer childhood distal humeral fractures |
| Region | Type of splint/cast | Indications | Pearls/pitfalls | Follow-up/referral |
|---|---|---|---|---|
| Ankle | Posterior ankle splint (“post-mold”) | Severe sprains | Splint ends 2 inches distal to fibular head to avoid common peroneal nerve compression | Less than one week |
| Isolated, nondisplaced malleolar fractures | Refer for displaced or multiple fractures or significant joint instability | |||
| Acute foot fractures | ||||
| Ankle | Stirrup splint | Ankle sprains | Mold to site of injury for effective compression | Less than one week |
| Isolated, nondisplaced malleolar fractures | ||||
| Lower leg, ankle, and foot | Short leg cast | Isolated, nondisplaced malleolar fractures | Compartment syndrome most commonly associated with proximal mid-tibial fractures, so care is taken not to over-compress | Two to four weeks |
| Refer for displaced or angulated fracture or proximal first through fourth metatarsal fractures | ||||
| Foot fractures—tarsals and metatarsals | ||||
| Weight-bearing status important; initially non–weight bearing with tibial injuries | ||||
| Knee and lower leg | Posterior knee splint | Acute soft tissue and bony injuries of the lower extremity | If ankle immobilization is necessary, as with tibial shaft injuries, the splint should extend to include the metatarsals | Days |
| Foot | Short leg cast with toe plate extension | Distal metatarsal and phalangeal fractures | Useful technique for toe immobilization | Two weeks |
| Often used when high-top walking boots are not available | Refer for displaced or unstable fractures |
GENERAL FRACTURE MANAGEMENT PRINCIPLES
It is important to maintain good anatomic fracture alignment throughout treatment. Acceptable angular deformity in the hand varies depending on the fracture site. Rotational deformity in the hand is never acceptable.
Stable fractures are generally reevaluated within one to two weeks following cast application to assess cast fit and condition, and to perform radiography to monitor healing and fracture alignment. Hand and forearm fractures, however, are often reevaluated within the first week.
Displaced fractures require closed reduction, followed by post-reduction radiography to confirm bone alignment. Both displaced and unstable fractures should be monitored vigilantly to ensure maintained positioning. If reduction or positioning is not maintained, urgent referral to an orthopedic subspecialist is warranted.8–10
Upper Extremity Splints and Casts
ULNAR GUTTER SPLINT
Common Uses. Nondisplaced, stable fractures of the head, neck, and shaft of the fourth or fifth metacarpal with mild angulation and no rotational deformities; nondisplaced, non-rotated shaft fractures and serious soft tissue injuries of the fourth or fifth, proximal or middle phalanx; boxer's fractures (distal fifth metacarpal fractures, the most common injury for which ulnar gutter splint/cast used).
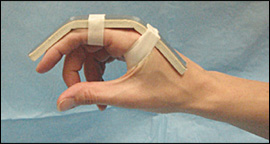
Application. The splint begins at the proximal forearm and extends to just beyond the distal interphalangeal (DIP) joint (Figure 1). Cast padding is placed between the fingers.
Position of Function. The wrist is slightly extended, with the metacarpophalangeal (MCP) joints in 70 to 90 degrees of flexion, and the proximal interphalangeal (PIP) and DIP joints in 5 to 10 degrees of flexion.
ULNAR GUTTER CAST
Common Uses. Definitive or alternative treatment of injuries commonly treated with ulnar gutter splint.8
Application. Ideally, the cast is applied 24 to 48 hours or more after the initial injury to allow swelling to decrease. Placement of the casting materials is similar to that of the ulnar gutter splint, except the plaster or fiberglass is wrapped circumferentially (Figure 3).

RADIAL GUTTER SPLINT
Common Uses. Nondisplaced fractures of the head, neck, and shaft of the second or third metacarpal without angulation or rotation; nondisplaced, nonrotated shaft fractures and serious injuries of the second or third, proximal or middle phalanx; initial immobilization of displaced distal radius fractures.11
Application. The splint runs along the radial aspect of the forearm to just beyond the DIP joint of the index finger, leaving the thumb free (Online Figure A). Cast padding is placed between the fingers.

Position of Function. The wrist is placed in slight extension, with the MCP joints in 70 to 90 degrees of flexion, and the PIP and DIP joints in 5 to 10 degrees of flexion.
RADIAL GUTTER CAST
Common Uses. Definitive or alternative treatment of fractures initially managed with a radial gutter splint.
Application. Placement of the casting materials is similar to that of the radial gutter splint, except the plaster or fiberglass is wrapped circumferentially (Figure 4). The cast is usually placed two to seven days after the initial injury to allow for resolution of swelling.

Pearls and Pitfalls. Minimal angulation or rotation at the fracture site may cause functional problems, such as difficulty with grasp, pinch, or opposition. Therefore, meticulous evaluation and follow-up are essential.
THUMB SPICA SPLINT
Common Uses. Suspected injuries to the scaphoid; stable ligamentous injuries to the thumb; initial treatment of nonangulated, nondisplaced, extra-articular fractures of the base of the first metacarpal; de Quervain tenosynovitis; first carpometacarpal joint arthritis.
Application. The splint covers the radial aspect of the forearm, from the proximal one third of the forearm to just distal to the interphalangeal joint of the thumb, encircling the thumb (Figure 2).
Position of Function. The forearm is in the neutral position with the wrist extended to 25 degrees and the thumb in a position of function (i.e., “holding a soda can”).
Pearls and Pitfalls. Immobilization of the thumb with a removable splint after a ligamentous injury is strongly preferred by patients, and the functional results are equal to those of plaster cast immobilization after surgical and nonsurgical treatment.12
THUMB SPICA CAST
Common Uses. Suspected or nondisplaced, distal fractures of the scaphoid; nonangulated, nondisplaced, extra-articular fractures of the base of the first metacarpal.
Application. The cast uses the same position of function as described for a thumb spica splint, but requires circumferential application of casting materials (Figure 5).

Pearls and Pitfalls. Because these types of fractures are often serious and have a high rate of complications, long-term splinting is not an appropriate definitive treatment. Angulated, displaced, incompletely reduced, or intra-articular fractures of the first metacarpal base should be referred for orthopedic subspecialist evaluation.8 Non-displaced distal fractures of the scaphoid have a greater potential to heal and may be placed in a short arm thumb spica cast and reevaluated out of the cast by radiography in two weeks.2,9 Nondisplaced fractures of the middle or proximal one third of the scaphoid are treated with a long arm thumb spica cast initially and require vigilant monitoring for nonunion.2
BUDDY TAPING (DYNAMIC SPLINTING)
Application. The injured finger is taped to the adjacent finger for protection and to allow movement (Online Figure B).

DORSAL EXTENSION-BLOCK SPLINT
Common Uses. Larger, middle phalangeal volar avulsions with potential for dorsal subluxation; reduced, stable PIP joint dorsal dislocations.
Application. In reduced, volar avulsion fractures, the splint is applied with the PIP joint at 45 degrees of flexion and secured at the proximal finger, allowing flexion at the PIP joint (Figure 6). With weekly lateral radiography, the flexion is decreased 15 degrees until reaching full extension over four weeks. Buddy taping should follow. Treatment of reduced PIP joint dislocations is similar, but requires a starting angle of 20 degrees.
ALUMINUM U-SHAPED SPLINT
Common Uses. Distal phalangeal fractures.
Application. The aluminum splint wraps from the dorsal fingertip around to the volar fingertip and immobilizes only the DIP joint in extension (Online Figure C).
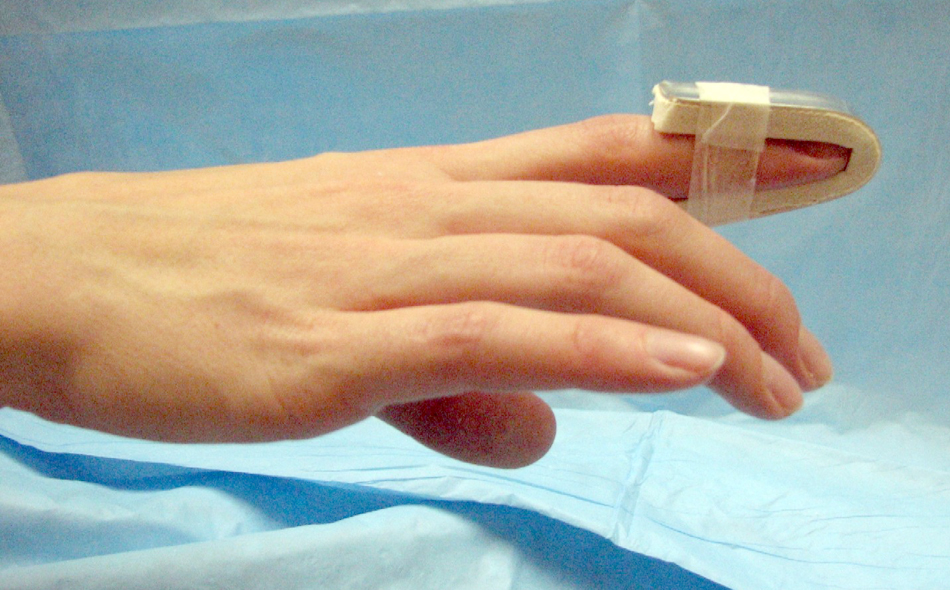
MALLET FINGER SPLINTS
Common Uses. Avulsion of the extensor tendon from the base of the distal phalanx (with or without an avulsion fracture).
Application. The DIP joint is placed in slight hyperextension with a padded dorsal splint, an unpadded volar splint, or a prefabricated mallet finger splint. Continuous extension in the splint for six to eight weeks is essential, even when changing the splint. Compliance is assessed every two weeks. Night splinting for an additional two to three weeks is recommended.
VOLAR/DORSAL FOREARM SPLINT
Common Uses. Soft tissue injuries of the hand and wrist; temporary immobilization of carpal bone dislocations or fractures (excluding scaphoid and trapezium).
Application. The splint extends from the dorsal or volar mid-forearm to the distal palmar crease (Figure 7).

Position of Function. The wrist is slightly extended.
Pearls and Pitfalls. The splint does not limit forearm pronation and supination, and is generally not recommended for distal radial or ulnar fractures. A recent study, however, demonstrated that compared with casting for definitive treatment of wrist buckle fractures in children, a removable plaster splint improves physical functioning and satisfaction, with no difference in pain or healing rates.13
SHORT ARM CAST
Common Uses. Nondisplaced or minimally displaced fractures of the distal wrist, such as Colles and Smith fractures or greenstick, buckle, and physeal fractures in children; carpal bone fractures other than scaphoid or trapezium.
Application. The cast extends from the proximal one third of the forearm to the distal palmar crease volarly and just proximal to the MCP joints dorsally (Online Figure D).

Position of Function. The wrist is in a neutral position and slightly extended; the MCP joints are free.
Pearls and Pitfalls. These are the same as for a forearm splint.
SINGLE SUGAR-TONG SPLINT
Common Uses. Acute management of distal radial and ulnar fractures.
Application. The splint extends from the proximal palmar crease, along the volar forearm, around the elbow to the dorsum of the MCP joints (Figure 8).

Position of Function. The forearm is neutral and the wrist is slightly extended.
Pearls and Pitfalls. The splint stabilizes the wrist elbow and limits, but does not eliminate, forearm supination and pronation.
LONG ARM POSTERIOR SPLINT
Common Uses. Acute and definitive management of elbow, proximal and mid-shaft forearm, and wrist injuries; acute management of distal radial (nonbuckle) and/or ulnar fractures in children.
Application. The splint extends from the axilla over the posterior surface of the 90-degree flexed elbow, and along the ulna to the proximal palmar crease (Online Figure E).
Pearls and Pitfalls. The posterior splint is not recommended for complex or unstable distal forearm fractures.
LONG ARM CAST
Common Uses. Definitive treatment of injuries initially treated with a posterior splint.
Application. The cast extends from the mid-humerus to the distal palmar crease volarly and just proximal to the MCP joints dorsally.
Position of Function. The elbow is flexed to 90 degrees with the wrist in a neutral, slightly extended position (Online Figure F).

Pearls and Pitfalls. Adequate padding at the olecranon, ulnar styloid, and antecubital fossa prevents skin breakdown. Physicians should avoid applying the edge of the casting tape over the antecubital fossa, particularly with the initial layer. Long arm casts are used most often in childhood because of the frequency of distal radial, ulnar, and distal humeral fractures.2,10,14
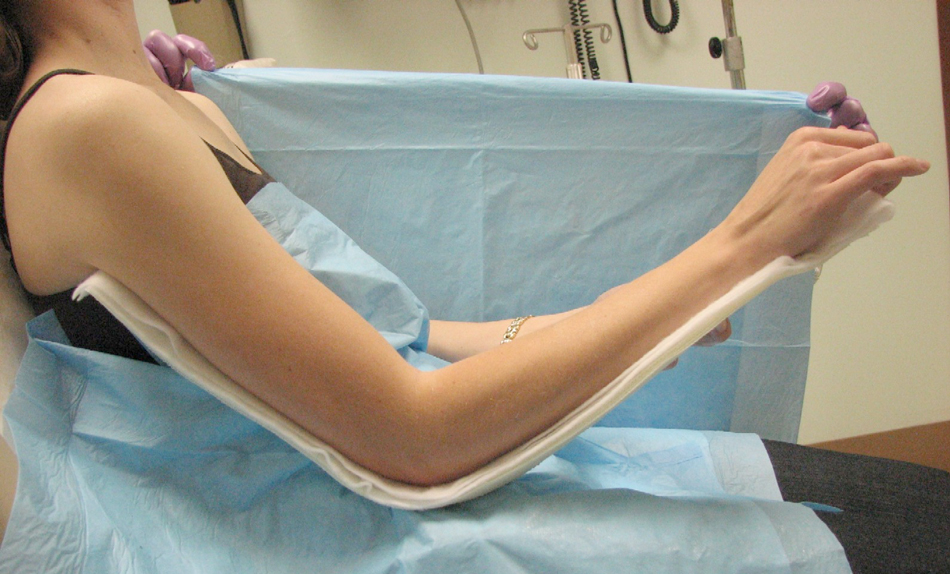
DOUBLE SUGAR-TONG SPLINT
Common Uses. Acute management of elbow and forearm injuries, including Colles fractures.

Pearls and Pitfalls. The splint provides superior pronation and supination control, and is preferable with complex or unstable fractures of the distal forearm and elbow.
Lower Extremity Splints and Casts
POSTERIOR ANKLE SPLINT (“POST-MOLD”)
Common Uses. Acute, severe ankle sprain; nondisplaced, isolated malleolar fractures; acute foot fractures and soft tissue injuries.
Application. The splint extends from the plantar surface of the great toe or metatarsal heads along the posterior lower leg and ends 2 inches distal to the fibular head to avoid compression of the common peroneal nerve (Online Figure G).

STIRRUP SPLINT
Common Uses. Acute ankle injuries; nondisplaced, isolated malleolar fractures.
Application. The splint extends from the lateral mid-calf around the heel, and ends at the medial mid-calf (Online Figure H).16 The position of function is with the ankle flexed to 90 degrees (neutral).

Pearls and Pitfalls. Stirrup and posterior ankle splints provide comparable ankle immobilization. Although the stirrup splint is adequate for short-term treatment of acute ankle sprains, the evidence favors a functional approach to inversion ankle sprain treatment with the use of a semirigid or soft lace-up brace.17
A bulky Jones splint is a variation on the stirrup splint used acutely for more severe ankle injuries. The lower extremity is wrapped with cotton batting and reinforced with a stirrup splint, providing compression and immobilization while allowing for considerable swelling.16
SHORT LEG CAST
Common Uses. Definitive treatment of injuries to the ankle and foot.
Application. The cast begins at the metatarsal heads and ends 2 inches distal to the fibular head. Additional padding is placed over bony prominences, including the fibular head and both malleoli (Online Figure I).

Position of Function. The ankle is flexed to 90 degrees (neutral).
Pearls and Pitfalls. Weight-bearing recommendations are determined by the type and stability of the injury and the patient's capacity and discomfort. Short leg walking casts are adequate for nondisplaced fibular and metatarsal fractures.2,18 Commercially produced high-top walking boots are acceptable alternatives for injuries at low risk of complications.2,19
TOE PLATE EXTENSIONS
Common Uses. Toe immobilization (comparable to a high-top walking boot or cast shoe); distal metatarsal and phalangeal fractures, particularly of the great toe.

Pearls and Pitfalls. The cast must be molded to the medial longitudinal arch with the ankle at 90 degrees to allow for successful ambulation.
POSTERIOR KNEE SPLINT
Common Uses. Stabilization of acute soft tissue injuries (e.g., quadriceps or patellar tendon rupture, anterior cruciate ligament rupture), patellar fracture or dislocation, and other traumatic lower extremity injuries, particularly when a knee immobilizer is unavailable or unusable because of swelling or the patient's size.
Application. The splint should start just below the gluteal crease and end just proximal to the malleoli (Online Figure J).

Position of Function. The knee is positioned in slight flexion.
Pearls and Pitfalls. If ankle immobilization is necessary, as with tibial shaft injuries, the splint should extend to include the metatarsals.