Am Fam Physician. 2010;82(8):971-972
Author disclosure: Nothing to disclose.
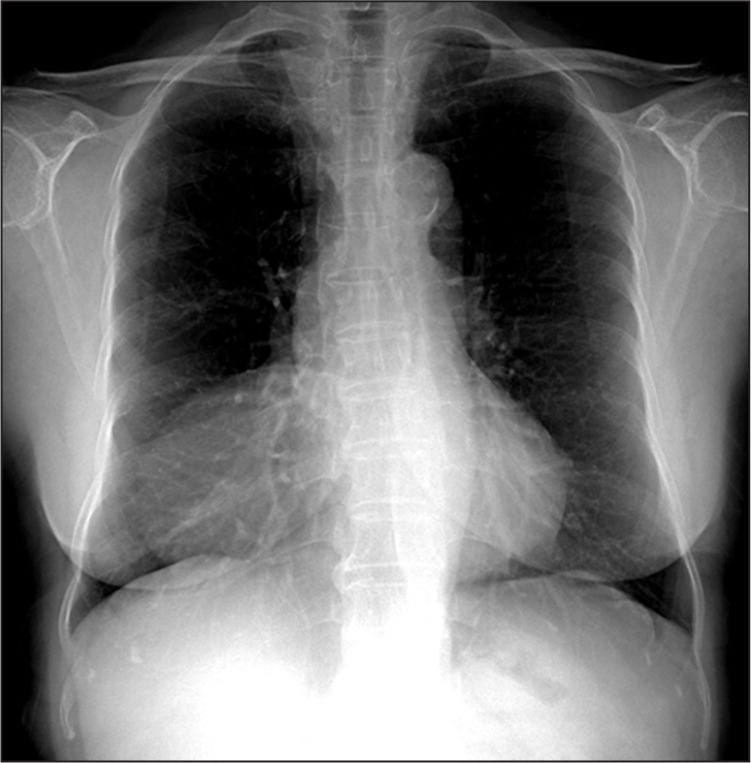
A 76-year-old, physically active woman presented for an annual physical examination. Chest radiography revealed a large right cardiophrenic mass (Figures 1 and 2). The patient had no remarkable medical history or physical examination findings. She had no history of tobacco use, fever, night sweats, anorexia, weight loss, shortness of breath, or dyspnea with exertion.

Question
Discussion
The answer is C: Morgagni hernia. A Morgagni hernia is a congenital diaphragmatic hernia and is not usually associated with other congenital anomalies.1 Morgagni hernias result from the failure of the sternal and costal components of the diaphragm to fuse during embryogenesis. The condition represents 3 percent of all diaphragmatic hernias and is more common in women.2 Most patients are asymptomatic, but the condition may be identified incidentally on chest radiographs. Occasionally, Morgagni hernias cause nonspecific cardiovascular, gastrointestinal, or respiratory symptoms.3
The hernias are always right-sided and located in the anterior cardiophrenic sulcus.2 More than 90 percent of cases have hernia sacs, which may involve the omentum, colon, stomach, and small intestine. Classic radiographic findings include a homogeneous, rounded soft tissue opacity in the right cardiophrenic angle. A lateral chest radiograph is needed to show the anterior location of the opacity. Although rare, an air-fluid level within the opacity is considered pathognomonic of a Morgagni hernia. Computed tomography can be diagnostic in more than 80 percent of patients by showing fat and omental vessels or abdominal viscera within the soft tissue mass.4 Once the condition is diagnosed, patients should be referred for reduction of the herniated organs and surgical repair of the anatomic defect.5
Carcinoma of the lung usually obscures bronchovascular markings and appears on radiography as an irregular or spiculated mass. Atelectasis, lymphadenopathy, or pleural effusion may be an associated finding.
Diaphragmatic eventration is nonparalytic weakening of the hemidiaphragm. It is usually partial and involves the anteromedial portion of the right hemidiaphragm. Radiography shows elevation of the affected area of the diaphragm, and the common pattern is a smooth hump along the contour of the diaphragm.6
Pericardial cysts are anomalous outpouchings of parietal pericardium. On radiography, the cysts are smoothly marginated masses touching the heart, particularly at the right anterior cardiophrenic angle. Pericardial cysts are sometimes difficult to distinguish from Morgagni hernias. Computed tomography or ultrasonography can demonstrate the cystic nature of the lesions.7
Enlarged pericardial fat pads are associated with Cushing syndrome, corticosteroid therapy, and obesity. They often occupy the right cardiophrenic angle. Although the fat pads may obliterate the angle, the cardiac and diaphragmatic borders are usually visible. The density of fat pads is not as great as that of Morgagni hernias, and their margins are not as sharply delineated.
| Condition | Characteristics |
|---|---|
| Carcinoma | Irregular or spiculated mass with obscured lung markings; possibly associated atelectasis, lymphadenopathy, or pleural effusion |
| Diaphragmatic eventration | Elevation of the affected area of the diaphragm; smooth hump along the contour of the diaphragm |
| Morgagni hernia | Homogeneous, rounded mass in the right anterior cardiophrenic angle; air-fluid level within the mass is considered pathognomonic |
| Pericardial cyst | Anomalous outpouching of parietal pericardium; smoothly marginated mass touching the heart |
| Pericardial fat pad | Associated with Cushing syndrome, corticosteroid therapy, and obesity; density not as great and margins not as sharply defined as those of Morgagni hernia or pericardial cysts |