
Am Fam Physician. 2011;84(1):92-94
Author disclosure: No relevant financial affiliations to disclose.
A 48-year-old woman presented to the emergency department with nausea, vomiting, and intermittent abdominal pain that had persisted for two days. The pain radiated from the epigastrium and left upper quadrant to her back. Nothing relieved the pain, and eating made it worse. The patient noted having two or three foul-smelling, loose stools during the previous two days. She denied fever or the presence of blood or mucus in her stools. Her medical history included type 2 diabetes mellitus requiring insulin therapy, alcoholism, many years of chronic abdominal pain, and chronic diarrhea. She had a cholecystectomy several years prior.
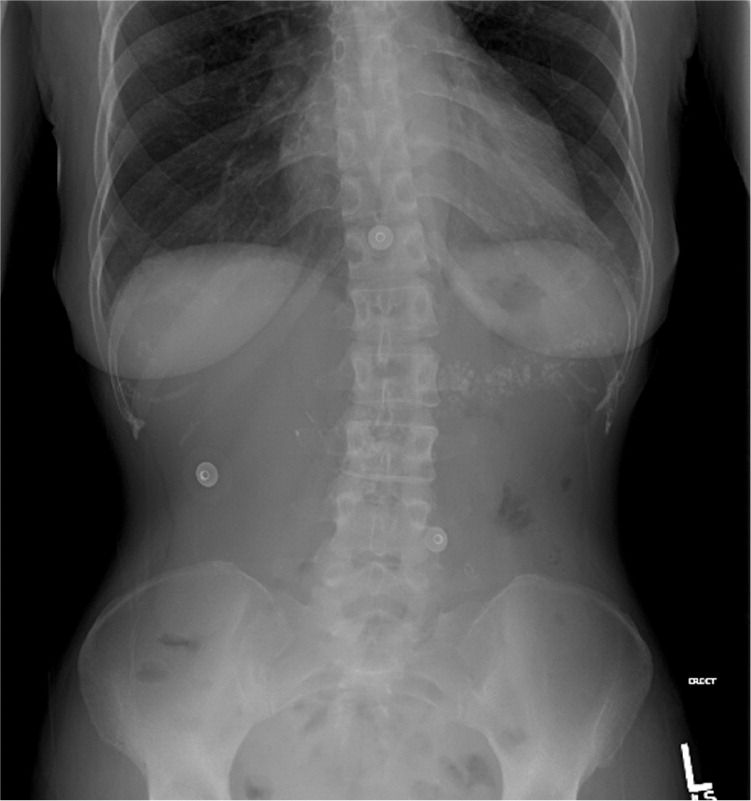
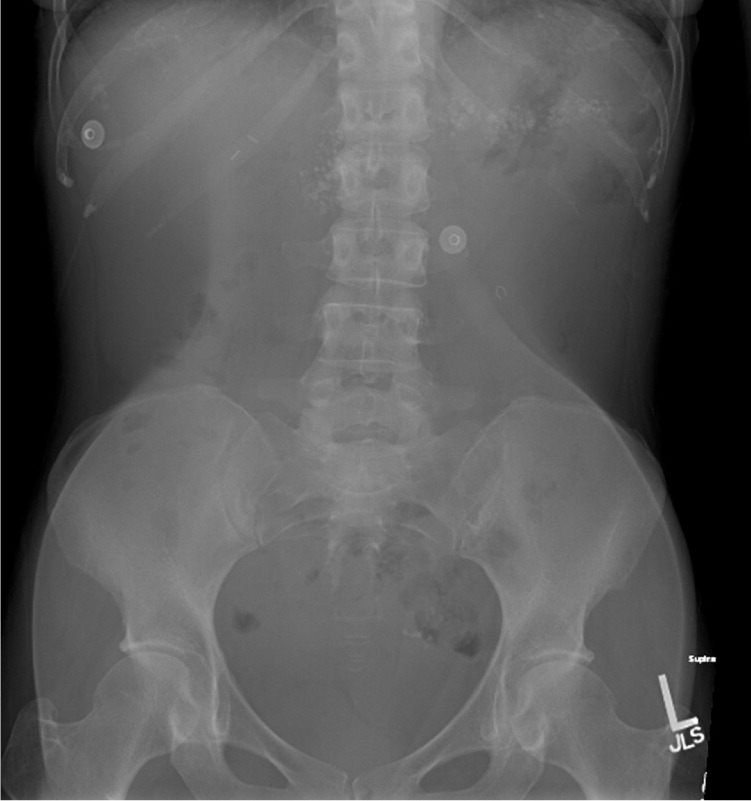
On examination, she was afebrile, her blood pressure was 130/80 mm Hg, her pulse was 96 beats per minute, and her respiratory rate was 16 breaths per minute. The patient appeared malnourished. She had tenderness in the epigastrium and left upper quadrant, but no rigidity or guarding. She had hyperactive bowel sounds, but no abdominal bruits or palpable masses. Her cardiac and pulmonary examinations were unremarkable. She had a blood glucose level of 250 mg per dL (13.88 mmol per L). Her liver function tests, amylase level, lipase level, complete blood count including white blood cell count and differential, and lipid panel were normal. Her albumin and prealbumin levels were low at 2.5 g per dL (25 g per L) and 8 mg per dL (80 mg per L), respectively, and her A1C level was 7.5 percent. Supine and erect abdominal radiography was performed (Figures 1 and 2).
Question
Discussion
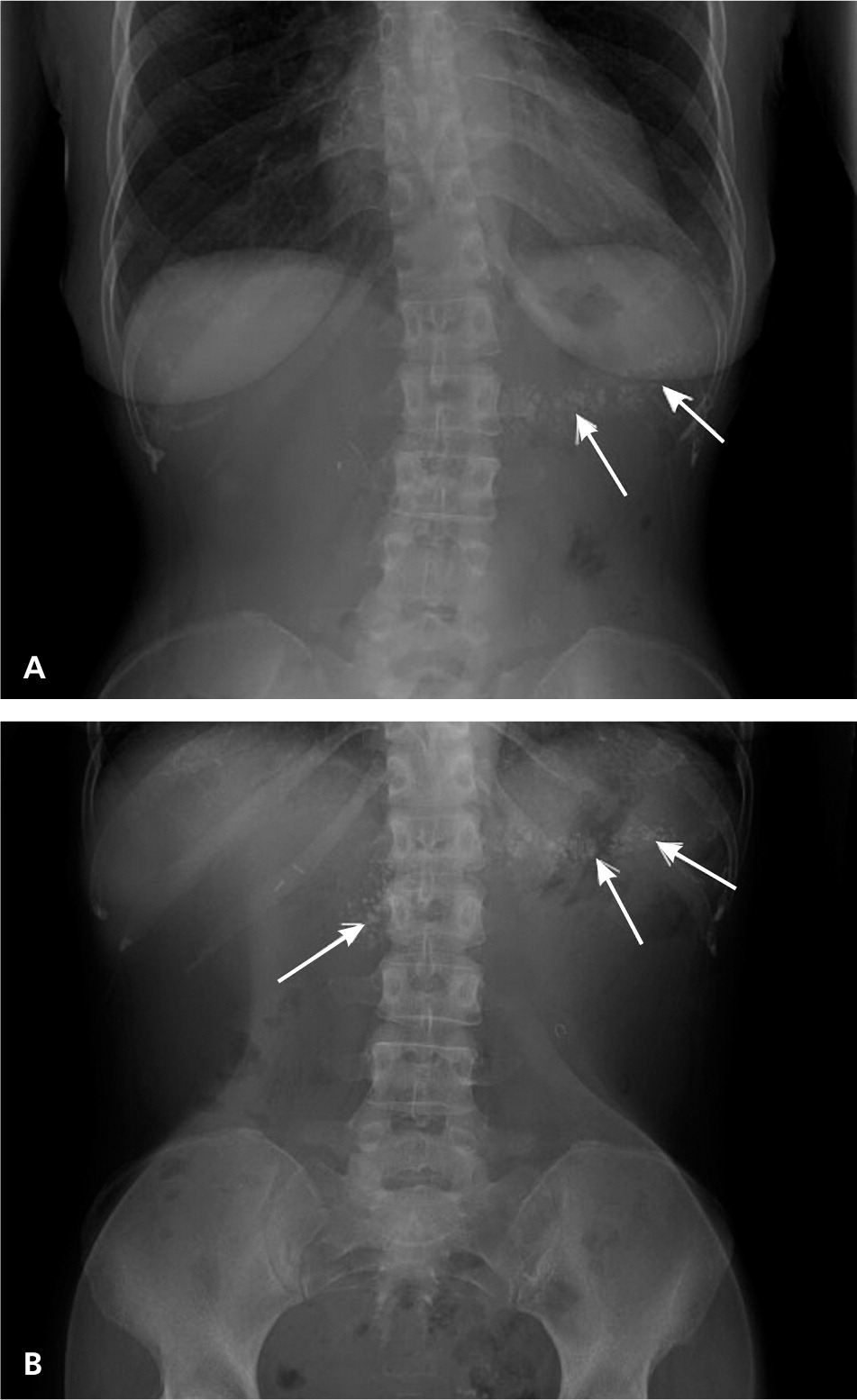
Answer C: chronic pancreatitis. Chronic pancreatitis is an inflammatory disease characterized by progressive fibrosis of the pancreas resulting in a loss of its exocrine and endocrine functions. The diagnosis is based on clinical presentation, laboratory findings, and imaging studies. The triad of steatorrhea, diabetes, and pancreatic calcifications on abdominal radiography strongly suggests the presence of chronic pancreatitis in this patient. The prevalence of chronic pancreatitis is difficult to estimate, primarily because acute and chronic pancreatitis are considered to be part of a spectrum rather than individual entities. Risk factors for chronic pancreatitis include alcoholism, hyperlipidemia, hypercalcemia, smoking, autoimmune pancreatitis, and a genetic predisposition to chronic pancreatitis.1 Recurrent episodes of acute pancreatitis are usually the precursor to chronic pancreatitis. 2,3 Most patients with alcoholism and recurrent pancreatitis will develop chronic pancreatitis in approximately five years.1,2
Epigastric pain that radiates to the back is the most common presenting symptom of chronic pancreatitis.4 The pain can be intermittent or continuous and may vary in severity. Amylase and lipase levels are elevated during acute attacks in the early phase of the disease, but may remain normal as the disease progresses to a more chronic state. As the condition progresses, patients develop deficiencies in the endocrine and exocrine function of the pancreas due to fibrosis and calcifications. This results in diabetes5 and fat malabsorption, leading to steatorrhea and malnutrition.
The pancreas usually cannot be visualized with standard abdominal radiography. However, in the later stages of chronic pancreatitis, calcifications form in the pancreatic ducts and then can be seen radiographically.6 In this patient, the abdominal radiographs show coarse calcifications in a horizontal distribution over the first and second lumbar vertebral bodies that extend to the patient's left side over the typical location of the pancreas (Figure 3). The diagnosis can be confirmed with contrast-enhanced computed tomography of the abdomen.1
Calcifications associated with abdominal aortic aneurysms are often incidental findings on imaging studies and appear as a curvilinear rim of calcification in the wall of the aneurysm along the spine.
In patients with bowel obstruction, abdominal radiography shows dilated loops of bowel with multiple air-fluid levels within the bowel loops, typically without calcifications.
Mesenteric lymph node calcifications do not cause abdominal pain and are usually secondary to an infection, an inflammatory process, or a malignancy elsewhere in the body. Abdominal radiographs demonstrate rounded or “popcorn” calcifications mostly in the right midabdomen and may appear to move inferiorly on upright abdominal films as the mesentery move inferiorly due to gravity.
Splenic artery calcifications and aneurysms appear as focal rounded calcifications in the left upper quadrant, usually in conjunction with calcifications elsewhere in the artery.7,8 These calcifications are not normally seen in a horizontal distribution or in the midline of the abdomen, but are typically serpiginous in nature because the splenic artery is usually tortuous in its course.
| Condition | Findings on abdominal radiography |
|---|---|
| Abdominal aortic aneurysm | Curvilinear rim of calcification in the wall of the aneurysm along the spine |
| Bowel obstruction | Multiple air-fluid levels and dilated bowel loops (diameter greater than 1.2 in [3 cm] in small intestine, greater than 2.4 in [6 cm] in large intestine) |
| Chronic pancreatitis | Spotted or mottled calcifications lying in a horizontal distribution over first and second vertebral bodies and extending into left upper quadrant of the abdomen |
| Mesenteric lymph node calcifications | Rounded or “popcorn” calcifications, mostly in the right midabdomen; calcifications appear to move inferiorly on upright abdominal films |
| Splenic artery aneurysms and calcifications | Splenic artery aneurysms appear like focal rounded calcifications in left upper quadrant, usually in conjunction with calcifications elsewhere in the artery; calcifications are usually serpiginous in nature |
