Am Fam Physician. 2012;85(4):383-384
Author disclosure: No relevant financial affiliations to disclose.
A 72-year-old man presented with shortness of breath and vomiting of three weeks' duration. Vomiting occurred without warning and consisted of undigested food. On the morning of this presentation, he awoke with food remnants in his nostrils and persistent coughing. The patient reported progressive difficulty with swallowing solids and liquids. He had occasional shortness of breath, constipation, and a 50-lb weight loss over the previous two years.
His medical history was significant for chronic obstructive pulmonary disease and gastroesophageal reflux disease. He had smoked one pack of cigarettes per day for more than 50 years, but did not abuse alcohol.

Question
Discussion
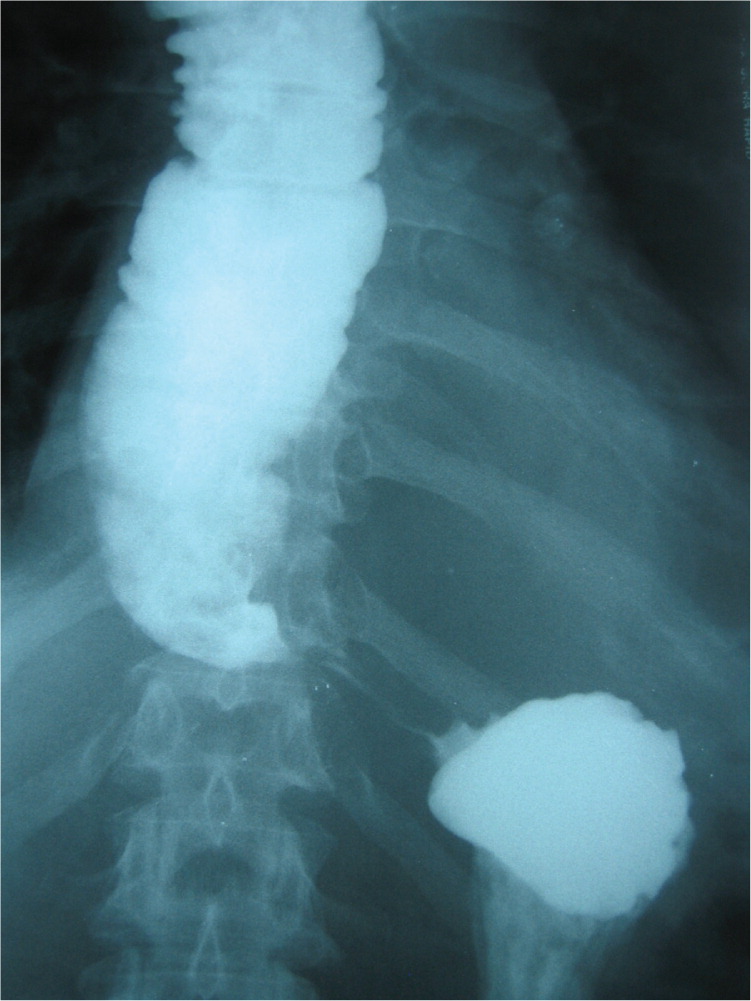
The correct answer is A: esophageal achalasia. Esophageal achalasia affects one per 100,000 persons annually.1 It is a motor disorder of the lower esophagus that is caused by a loss of the myenteric plexus of neurons.2 The lower esophageal sphincter (LES) fails to relax properly, which prevents food and liquids from passing into the stomach. Most persons with this condition are diagnosed between 25 and 60 years of age. Increasing difficulty with swallowing is usually the presenting symptom. Regurgitation of undigested food is an important diagnostic feature of esophageal achalasia, and rarely causes aspiration pneumonia. Some patients may also have heartburn, weight loss, cough, or chest pain.3
A barium esophagogram showing persistent narrowing at the gastroesophageal junction, which produces a “bird's beak” or “rat's tail” appearance, is characteristic of esophageal achalasia. Computed tomography often shows an air-fluid level in the dilated esophagus above the narrowing. Esophageal manometry demonstrates incomplete relaxation of the LES, an elevated basal LES pressure, and the absence of peristaltic contractions in the thoracic esophagus.
Treatment of esophageal achalasia includes medications such as nitrates, anticholinergics, and calcium channel blockers to reduce LES pressure. OnabotulinumtoxinA (Botox) injections into the sphincter can produce temporary paralysis of LES muscles.4 Balloon (pneumatic) dilatation or surgical myotomy can be used if more conservative therapies are ineffective.5 Early treatment can help prevent complications, such as perforation, mega-esophagus, esophageal strictures, and cancer. All patients undergoing treatment for esophageal achalasia should receive follow-up with endoscopy, because of the increased risk of squamous carcinoma and adenocarcinoma.6
Esophageal carcinoma usually occurs in older persons. Dysphagia is the most common presenting symptom followed by weight loss. Barium esophagography is sensitive for mucosal irregularities. If the clinical suspicion is high and mucosal abnormalities are present, endoscopy is essential for visualization and biopsy.
Patients with diffuse esophageal spasm may present with intermittent dysphagia and chest pain. Barium esophagography and manometry can demonstrate diffuse, uncoordinated contractions of the esophagus (“corkscrew” appearance).
In patients with peptic strictures, dysphagia initially includes solids and progresses to involve both solids and liquids. Peptic strictures are associated with heartburn, and pH monitoring is positive for acid reflux. There is smooth narrowing of the distal esophagus, usually at the squamocolumnar junction, on barium esophagography.7
The major clinical features of scleroderma are heartburn, reflux, and dysphagia to solids and liquids.8 Esophageal manometry and barium esophagography demonstrate hypomotility in the lower esophagus, and the LES is freely open. Multiorgan involvement with a positive antibody panel is characteristic of scleroderma.
| Condition | Characteristics |
|---|---|
| Esophageal achalasia | Progressive dysphagia; associated with respiratory symptoms and weight loss; barium esophagogram shows persistent narrowing at the gastroesophageal junction, and computed tomography often shows an air-fluid level above the narrowing; lower esophageal sphincter does not relax on manometry |
| Esophageal carcinoma | Progressive dysphagia, initially to solids only; associated with weight loss; mucosal irregularities on barium esophagography; endoscopic biopsy confirms the diagnosis |
| Esophageal spasm | Intermittent dysphagia and chest pain; “corkscrew” appearance on barium esophagography and manometry |
| Peptic stricture | Progressive dysphagia, initially to solids only; associated with heartburn; pH monitoring positive for acid reflux; smooth narrowing of the distal esophagus on barium esophagography |
| Scleroderma | Chronic progressive dysphagia to solids and liquids; heartburn and reflux; hypomotility in lower esophagus on manometry and barium esophagography; multiorgan involvement with a positive result on an antibody panel |