
Am Fam Physician. 2013;87(3):217-219
Author disclosure: No relevant financial affiliations to disclose.
A 62-year-old nursing home patient presented with dyspnea. He had recently been discharged from the intensive care unit after treatment for urosepsis with multiple organ failure. While in the hospital, he required vasopressors and mechanical ventilation for more than three weeks.
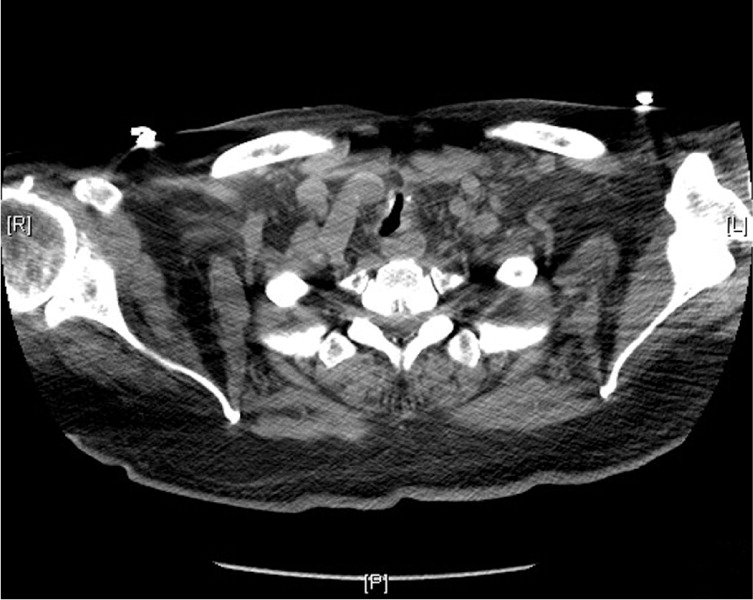
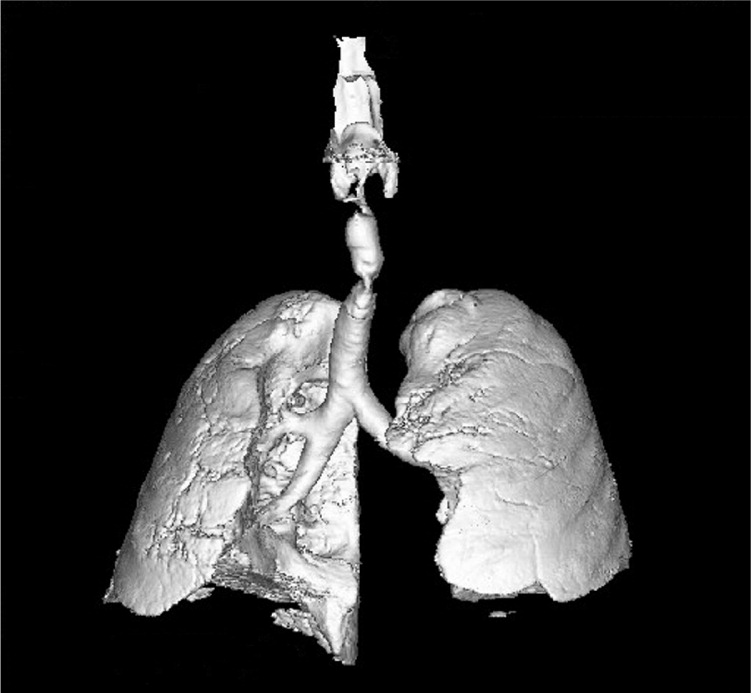
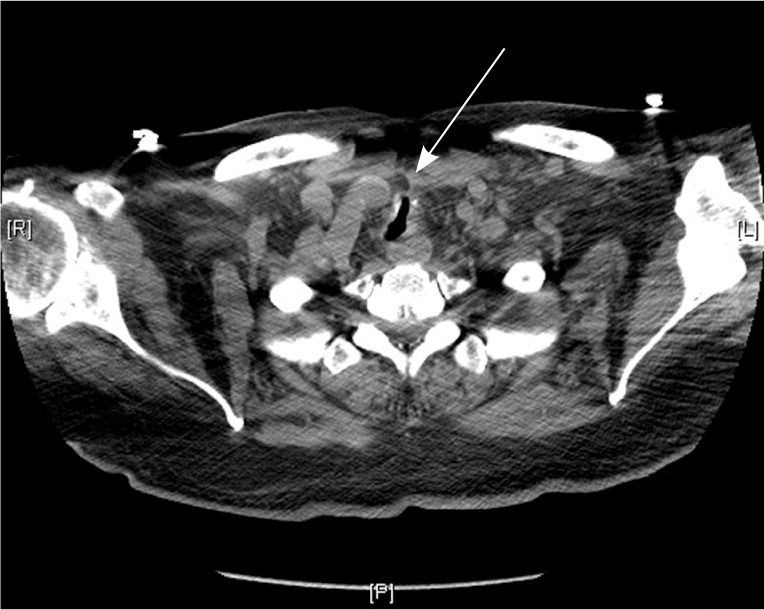
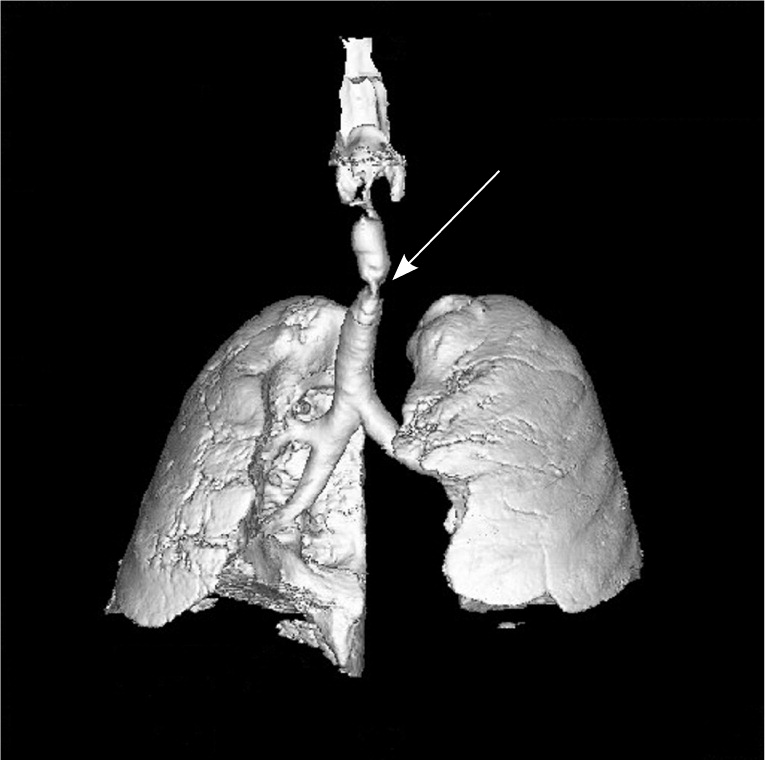
After discharge to a skilled nursing facility, the patient had several episodes of acute respiratory failure. The episodes were sudden and self-limited, resolving rapidly with minimal intervention, such as nebulizers, supplemental oxygen, or head repositioning, and were associated with clear lungs on auscultation. The episodes occurred when the patient was recumbent with his head slightly elevated, or when he was sitting and reached forward. Imaging was performed (Figures 1 and 2).
Question
Discussion
The answer is C: tracheomalacia. Tracheomalacia refers to diffuse or segmental tracheal cartilage weakness. It can be classified by appearance (anteroposterior tracheal narrowing or lateral), distribution (diffuse or segmental), or timing of appearance (congenital or acquired).1 The acquired form is most common in adults, particularly in those who were intubated or had a tracheostomy. Tracheostomy or endotracheal intubation can destroy tracheal cartilage at the stoma or inflatable cuff site, respectively, which weakens the tracheal wall.2 This type of tracheomalacia is usually segmental, with a length of 3 cm or less.
Possible risk factors for tracheomalacia include recurrent or prolonged intubation, and concurrent high-dose steroid therapy. The mechanism is uncertain but may be related to pressure necrosis, impaired blood flow, recurrent infections, mucosal friction, or mucosal inflammation.2 Other causes include recurrent infections, severe emphysema with chronic inflammation due to the inhalation of irritants (e.g., cigarette smoke), history of trauma from high-impact sports, and chronic external compression of the trachea (e.g., goiter, extrinsic vascular congestion).3
This patient's symptoms are explained by an anteroposterior, segmental narrowing of the trachea a few centimeters below the vocal cords (Figure 3). Air entry and movement were compromised when he moved his head forward or flexed at the neck while in a seated position. Figure 4 shows a three-dimensional reconstruction of the lungs and trachea, where the tracheomalacia lesion is evident.
Sudden shortness of breath in a frail patient with recent intubation and multiple organ failure raises the possibility of flash pulmonary edema. This patient's shortness of breath was related to positional changes of his head or neck and was not associated with signs of volume overload. Flash pulmonary edema leads to decreased breath sounds, rales, rhonchi, or wheezing, and jugular venous distention.
Gastroesophageal reflux causing a chronic aspiration syndrome with bronchospasm is associated with signs of bronchospasm, such as wheezing, rales, and fine expiratory rhonchi. A history of gastroesophageal reflux disease would make this diagnosis more likely.
Lung damage, such as barotrauma, that causes gross air leaks or volutrauma is a more subtle type of lung injury that can occur secondary to pulmonary overdistention. This type of damage can be induced by mechanical ventilation. Cyclical atelectasis, also called atelectrauma, refers to the damage that can occur when lungs become atelectatic and then are reexpanded. Biotrauma is the inflammatory response to increased cytokine recruitment in the alveoli after overstretching lung cells. The presentation is slower than tracheomalacia, and it does not resolve spontaneously. There are no breath sounds in the affected hemithorax, but there are signs of intrathoracic hypertension.
Persistent pneumonia and atelectasis arising after mechanical ventilation has a slower presentation. It causes systemic symptoms, such as fever and cough, accompanied by respiratory signs (e.g., rales, rhonchi) on physical examination.
| Condition | Characteristics |
|---|---|
| Flash pulmonary edema | Decreased breath sounds, rales, rhonchi, or wheezing, and jugular venous distention |
| Gastroesophageal reflux with sudden aspiration and pneumonitis | Bronchospasm symptoms after aspiration, such as wheezing, rales, and fine expiratory rhonchi |
| Tracheomalacia | Diffuse or segmental tracheal cartilage weakness related to recent intubation; symptoms occur suddenly and resolve spontaneously |
| Ventilator-induced lung damage | Findings during or immediately after mechanical ventilation, no breath sounds in the affected hemithorax, signs of intrathoracic hypertension |
| Ventilator-related persistent pneumonia and atelectasis | Findings arising after mechanical ventilation; respiratory symptoms, such as rales and rhonchi; systemic symptoms, such as fever and cough; not relieved with changes in position; insidious onset |
